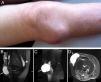
We present the case of an 80-year-old woman with obesity (BMI: 32.4), who had Kellgren–Lawrence stage IV osteoarthritis of the right knee. She had a history of an anterolateral mass on her right knee for the past 6 years which was round, fluctuating in consistency, non-painful and with no associated erythema, and did not impede movement (Fig. 1A). No prior trauma had been documented. She had recently undergone a Magnetic Resonance Imaging study (MRI) which described the presence of a cyst in the lateral region of the knee and which came into contact with the joint space at the meniscal space level (Fig. 1B–D). This parameniscal cyst had been drained on several occasions obtaining mucoid, aseptic material, with no complications. The most recent drainage had been performed 2 months prior to the hospitalization date. The patient came to the clinic due to enlargement of the parameniscal cyst and due to the appearance of a second mass on the same leg, distal and lateral to the original. This new mass had developed over the past 30 days, was accompanied by pain upon light touch and showed unequivocal local signs of inflammation. In the 2 days prior there had been spontaneous drainage of pus from the new mass which coincided with the appearance of fever.
(A) External aspect of the right knee. (B) MRI of the right knee, T2 potentiated, coronal scan. Demonstration of the communication of the cytic cavity with the joint cavity. The long arrow points to the parameniscal cyst. The arrowheads show the continuity of signal to the joint recess. The hollow arrowhead points to part of the communication between the meniscal cyst and the synovial capsule. (C and D) Sagittal and axial scan, respectively, of the right knee. Arrows point to the parameniscal cyst.
X-rays showed an ovoid, well limited structure with an air–liquid level 8cm distal from the parameniscal cyst, on the upper, lateral third of the leg, as well as an increase in the opacity of soft tissue at that level (Fig. 2). The culture of the fluid obtained from this newer collection isolated methicillin-sensitive Staphylococcus aureus. Faced with the possibility of a macroscopic communication between the collection, the parameniscal syst and the joint, we proceeded to surgically drain it, perform a joint lavage and abscess debridement. During the intervention, communication between the parameniscal cyst, the joint and the collection was demonstrated, with spontaneous drainage however, synovial fluid culture confirmed the absence of a joint infection.
The prevalence of meniscal cysts has been estimated around 1%–8%.1–3 They may present as intrameniscal or parameniscal collections, the latter more frequent at a rate of 2:1.2 Parameniscal cysts are defined as a formation lined by evaginated synovial tissue from the meniscal space, connected to the latter and containing synovial fluid.1,2,4–6 The presence of a parameniscal cyst was associated to the existence of a traumatic or degenerative meniscal lesion, most frequently found adjacent to the medial meniscus with respect to the lateral (at a rate of 3:2),2 however, clinical detection is easier for lateral parameniscal cysts. As in synovial cysts, parameniscal cysts are formed as a consequence of a synovial evagination produced by unidirectional pressure in an extraarticular direction.4,6,7 When symptomatic, parameniscal cysts may be resolved surgically, arthroscopically, obliterating the communication channel with the joint.8
Dissecting proliferation of the content of a parameniscal cyst and the consequent infection has no precedent in the medical literature. The case implies a previously undescribed infectious complication. In light of the results of the bacteriologic tests, which circumscribed the infection to the fluid collection which formed distally, the most plausible mechanism for our case would be the formation of a parameniscal cyst, dissection of the content distally due to gravity, formation of a new collection laterally and proximally in the leg, opening of the collection to the skin, infection and inoculation by skin germs and formation of an abscess in the new collection with concomitant regional and systemic affection. The absence of infection in the parameniscal cyst and the joint itself may be explained by the presence of an evacuation channel to the exterior through which fluid flowed unidirectionally favored by gravity and a greater intraarticular pressure with respect to the parameniscal cyst, as well as the distal collection.
Ethical ResponsibilitiesProtection of people and animalsThe authors state that no experiments were performed on people or animals for this study.
Data confidentialityThe authors state that the protocols of their center regarding the publication of patient data have been followed.
Right to privacy and informed consentThe authors have obtained informed consent from the patients and/or subjects referred to in the article. This document is in the possession of the corresponding author.
To the Department of Rheumatology of the Hospital Universitario Ramón y Cajal.
Please cite this article as: Sobrino Grande C, Blázquez Cañamero MÁ, Astete CG, de la Puente Bujidos C. Quiste parameniscal gigante complicado con disección distal e infección regional. Reumatol Clin. 2015;11:116–117.