A 37-year-old woman with a history of undergoing bariatric surgery and a tummy tuck was diagnosed at age 32 as HLA B27 positive and with ankylosing spondylitis and stage IV bilateral sacroiliitis according to the modified New York criteria. She currently showed no signs of arthritis or enthesitis. She was initially treated with Etanercept® and Abdalimumab®, but presented symptoms of peripheral polyneuropathy that were probably secondary to the use of these drugs and which had to be replaced by Abatacept®, with a compassionate care indication in this case.
In March 2010, with the patient undergoing follow-up by the rheumatology department, she began with episodes of acute back pain radiating to the ribs, of a mechanical nature and which intensified during the last week appearing even at rest. She had no neurological deficits or any other symptoms. On physical examination the patient had a modified Schober test of 12.5cm, a Bath Ankylosing Spondylitis Functional Index Index (BASFI) of 1 and a Bath Ankylosing Spondylitis Disease Activity Index (BASDAI) of 2.8. Bone densitometry showed femoral osteopenia (T-score −2.2, Z-score −2.9) but there was no lumbar osteopenia or osteoporosis (T-score 0.2, Z-score −0.8). She had not received prior glucocorticoid treatment or had other risk factors for osteoporosis.
On the last visit, the patient presented mechanical pain so intense that she was hospitalized in the unit of spinal trauma for pain management and complementary testing:
- -
Laboratory tests showed: hemoglobin 10.6g/dl (12–15), mean corpuscular volume, 74fl (78–100), ESR 35 (0–20). The biochemistry, protein profile, and urinalysis were normal. PPD was negative and blood cultures were negative.
- -
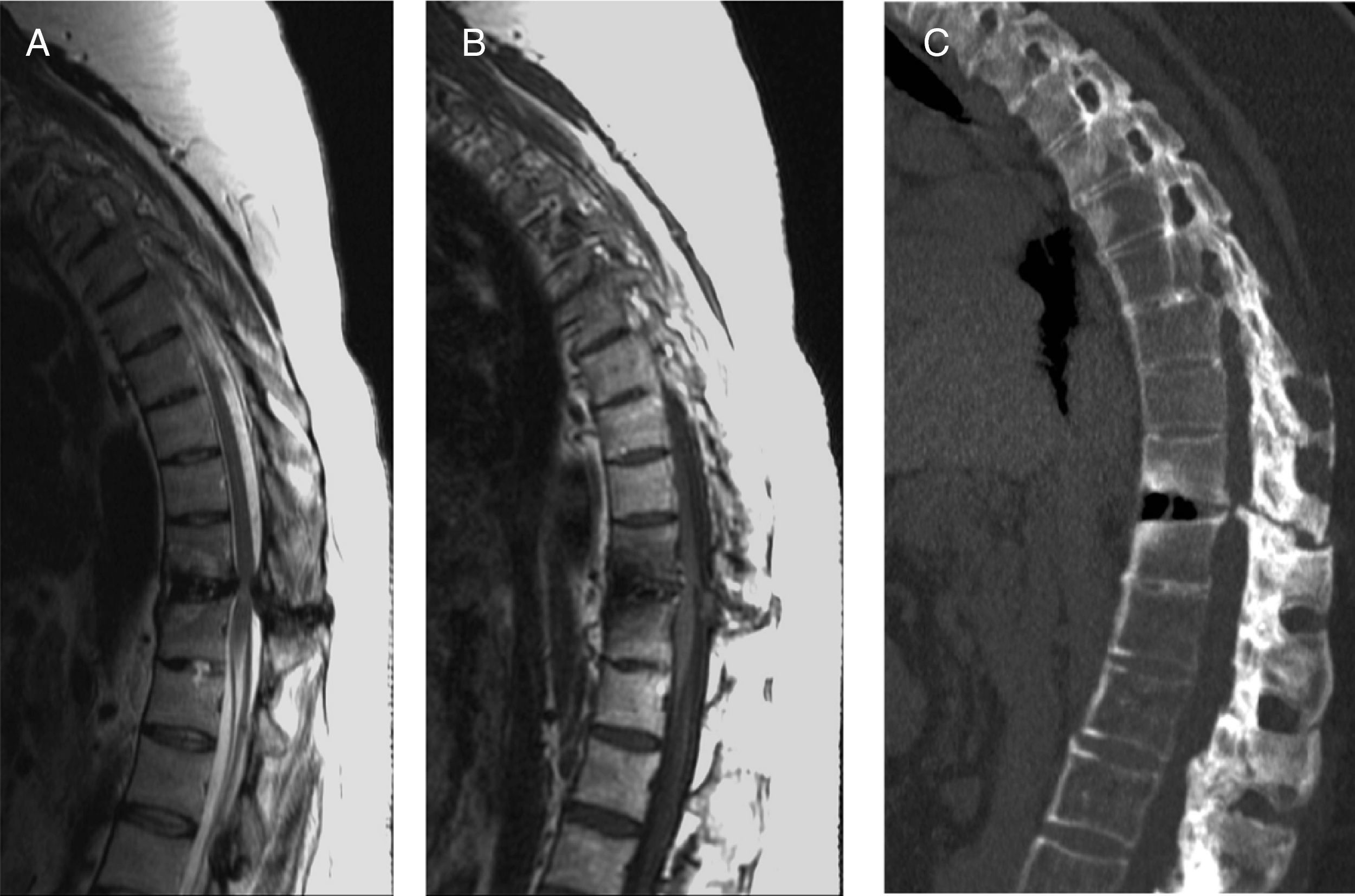
Magnetic resonance imaging (MRI) and computed tomography (CT) of the thoracolumbar spine (Fig. 1) observed: vertebral fracture at D11–D12 with involvement of the disc and interapophyseal joints. Signs of ankylosing spondylitis with ossification of posterior longitudinal ligaments and interapophyseal joint facet fusion. Signs of degenerative sclerosis of the articular surfaces, osteochondrosis, osteophytes, and calcification of yellow ligaments, causing a decrease in spinal canal caliber and resulting in stenosis at that level. Alteration of signal strength of the bone on D11–D12 (hyperintense in T2) was consistent with compressive myelopathy.
Fig. 1.(A and B) Sagittal images of the thoracolumbar spine in T2 and T1 potentiated sequences, respectively. (C) Sagittal CT scan of the thoracolumbar spine. An alteration in the signal intensity at the D11–D12 level can be seen, corresponding with compressive myelopathy. The CT shows signs of ankylosing spondylitis (fusion of the interapophyseal facets and ossification of the common posterior vertebral ligament) along with signs of degeneration. At the level of D11–D12 the compressive myelopathy's secondary nature can be seen, as the vertebral fracture is evident.
Given these findings, a diagnosis of compressive myelopathy at D11–D12 secondary to vertebral transdiscal fracture was made. Hospital treatment was begun with rest and administration of intravenous analgesia. After 8 weeks the patient improved clinically from her back pain and was discharged with conservative treatment and bracing.
The patient continued to have episodes of exacerbation of pain during the following year, and a control MRI was performed at 11 months showing persistent signs of compressive myelopathy. The persistence of pain and the ineffectiveness of conservative treatment led to opting for bone fusion treatment.
DiscussionAnkylosing spondylitis (AS) is a chronic inflammatory disease characterized by back pain due to involvement of the spine and sacroiliac joints, with syndesmophyte formation leading to vertebral ankylosis, and frequently associated with peripheral arthritis, enthesitis, and a history of acute uveitis.1 Osteoporosis, stiffness, and deformity that appear throughout the disease are conditions associated with an increase in the prevalence of fractures (10%–17%).2
Anderson classified fractures into 3 groups: vertebral fractures that can occur in patients with ankylosing spondylitis: transdiscal (through the intervertebral space), transvertebral (which concerns the vertebral body) or mixed.3,4. Their pathophysiologic mechanism is not entirely clear in the literature4; the most likely causes being inflammatory, infectious, and traumatic. They are more common in patients with longstanding disease and those with syndesmophytes, with more intense lumbar spine bone loss.5
Clinically it may present as acute pain, usually after a history of trauma, or progressive pain.3,4 Sometimes they are asymptomatic, and if there is compressive myelopathy, the symptoms of intermittent claudication or root compression may be present.4 Thumbikat et al.2 conducted a retrospective study in 18 patients with ankylosing spondylitis who had suffered spinal cord injury and found that the most frequent cause was predominantly trauma to the low cervical region.
The diagnosis is based on: radiography (initially determining the location of the lesion), CT (which is useful to determine the exact location and degree of stenosis of the spinal canal) and MRI (which determines the existence of spinal cord injuries or other complications).4
The initial treatment is conservative (NSAIDs and immobilization),4,6 reserving surgery for cases in which it fails, or where there are progressive neurologic deficit symptoms.4,6
Other complications that may be associated with these fractures are epidural hematoma and vertebral artery lesions.4,5,7
The interest of the case lies in the role of MRI in assessing the complications that can occur with vertebral fractures in patients with AS and that in many cases may be undetectable with other imaging techniques. In fact, although simple radiography is the initial test to assess spinal lesions in patients with AS, it is of no use in the study of spinal cord involvement which may occur in the vertebral spine.
Please, cite this article as: Bueno Palomino A, et al. Mielopatía compresiva como forma de presentación de una fractura transdiscal de bloque vertebral en una paciente con espondilitis anquilosante. Reumatol Clin. 2012;8(2):100–101.