A 6-year-old boy was admitted because of pain, swelling and loss of function in his left knee, with an onset 2 weeks prior.
His past medical history included the repeated bouts of otitis, without other diseases.
Two days before, he had presented fever and abdominal pain, which limited itself. The patient had no other musculoskeletal symptoms or oropharyngeal manifestations.
The physical examination showed clear signs of inflammation in his left knee with flexion limitation but full extension. Arthrocentesis was performed, yielding 15cc of synovial fluid of purulent appearance, and samples were sent to the laboratory for culture.
Laboratory tests highlighted a normal leukocyte count, C-reactive protein and elevated erythrocyte sedimentation rate (CRP: 124mg/l and ESR: 30mm/h). Infectious serology was negative (Brucella, Yersinia, Borrelia, Chlamydia, Campylobacter, parvovirus B19), as were blood cultures, Mantoux testing and autoimmunity tests (negative ANA, anti-DNA, ANCA, HLA B27, immunoglobulins and RF). Synovial fluid analysis from the left knee showed signs of inflammation, with 125,200leukocytes/mm3, predominance of polymorphonuclear cells (95%), a glucose of 22mg/dl and elevated proteins (5.9g/dl).
The cultures isolated Fusobacterium nucleatum, and there was no antibiotic resistance.
Imaging tests found a diffuse opacity of the right maxillary sinus, with accumulation of secretions inside it and without associated clinical sinusitis.
An ultrasound of the left knee showed moderate synovial effusion and high echogenicity in the posterior recess.
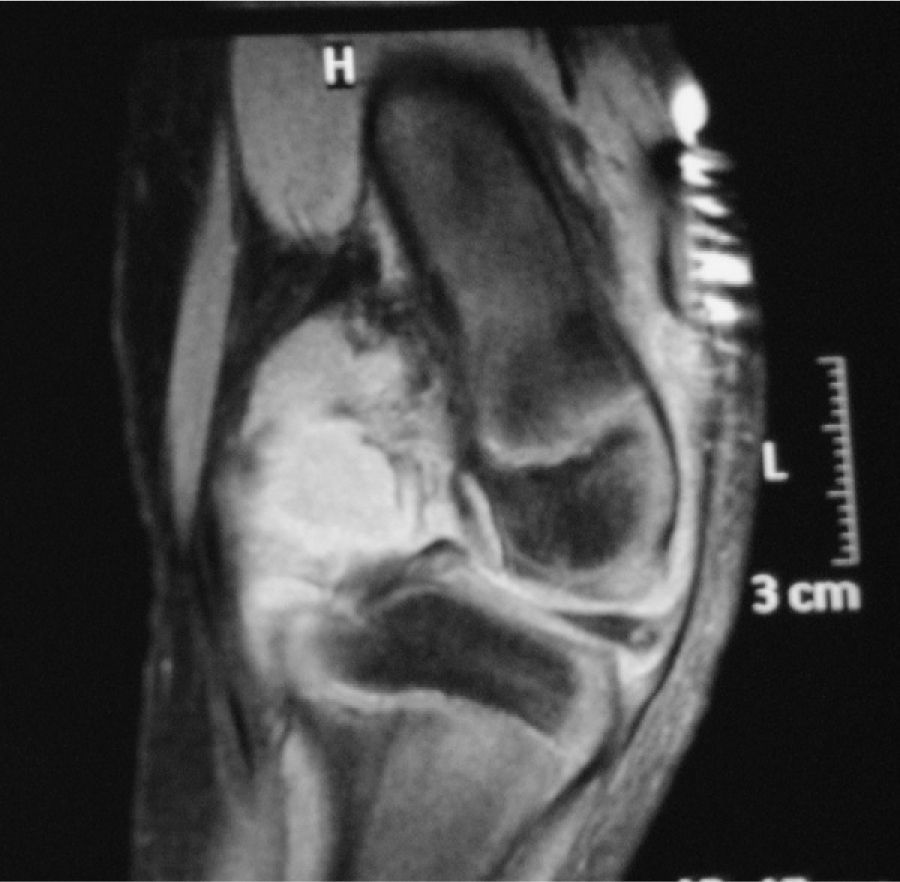
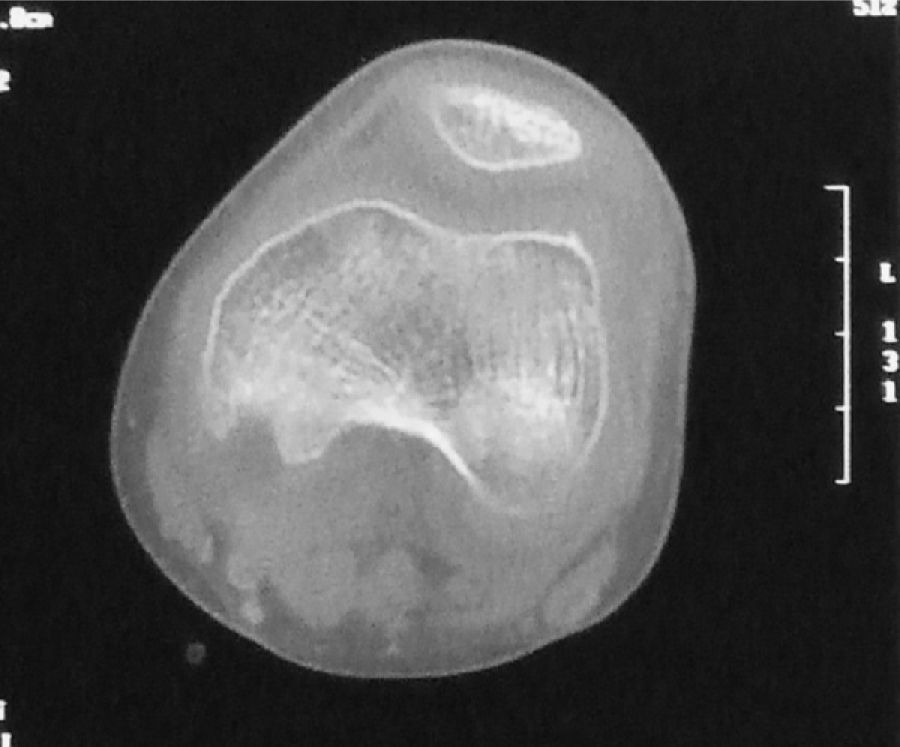
Nine days after admission, an MRI was performed which showed a moderate collection in the joint cavity, mainly in the intercondylar notch and showing contrast uptake compatible with synovial proliferation (Fig. 1). In the back of the left femoral condyle, we identified a small lytic lesion of approximately 7mm×5mm in diameter, associated with a collection that had peripheral contrast uptake, compatible with small bone inflammation. A CT was performed within 20 days, and a 6-mm lytic lesion was seen in the posterior aspect of the medial femoral condyle, with involvement of the cortical bone without any periosteal reaction observed (Fig. 2).
Septic arthritis of the left knee by Fusobacterium nucleatum, with secondary erosion of the left posterior femoral condyle. Right maxillary sinusitis.
ProgressionOn admission, parenteral antibiotic treatment was begun with cephotaxime and cloxacyllin. After receiving the culture positive for Fusobacterium nucleatum, we started treatment with intravenous metronidazole for 21 days. Given the initial evolution showing marked swelling and flexion deformity of the joint, we decided to perform the arthrotomy with debridement and partial synovectomy with surgical drainage and placement of a continuous lavage system, which was maintained for 5 days.
After discharge, oral treatment continued for 2 weeks and the patient underwent rehabilitation. The clinical course was favorable, showing no residual deformity or loss of function.
In later visits, a left knee CT and scintigraphy were performed and were normal, with disappearance of the bone erosion.
DiscussionSeptic arthritis caused by anaerobic microorganisms is rare. It is estimated that its prevalence is below 1%,1 and Fusobacterium spp. is the most frequently found germ.
Fusobacterium spp. is a strictly anaerobic bacterium that is part of the flora of the oral, vaginal and intestinal mucosa. There have been reports of septic arthritis by this bacterium after dental procedures, tonsillectomy, dental abscess drainage and other pharyngeal infections.2,3 In the case of our patient, there was a history of frequent otitis, and signs of right maxillary sinus inflammation as potential risk factors, with normal immunological tests.
Fusobacterium necrophorum is the most virulent germ of the species, classically associated with Lemierre syndrome, which characteristically presents with thrombophlebitis of the internal jugular vein. Only rarely does it cause septic arthritis.
Fusobacterium nucleatum septic arthritis in immunocompetent patients is extremely rare,3 with few published cases in children.4–7 Hence, the peculiarity of the case is presented.
In septic arthritis it is important to establish a specific treatment early because of the possibility of rapid joint destruction, which would be accompanied by an irreversible loss of functionality. Treatment involves drainage of the joint along with appropriate antibiotic therapy. Drainage can be accomplished through arthrocentesis, arthroscopy, or through open surgical drainage or arthrotomy, as in this case.
Please cite this article as: Carrasco Cubero C, et al. Artritis séptica por Fusobacterium nucleatum en paciente inmunocompetente. Reumatol Clin. 2012;8(2):98–9.