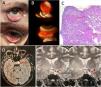
A 59-year-old woman with a history of acute bilateral conjunctival lesion episodes since the age of 18, with nodular characteristics, under 2 mm in diametre, yellow-erythematous with conjunctival erythema, some painful, requiring topical treatments. At the age of 57 years, polyarthritis was added to the clinical background.
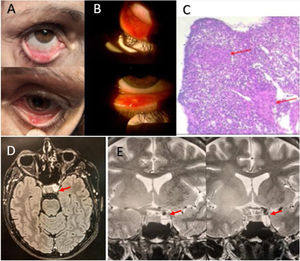
Laboratory: anaemia of chronic diseases, erythrocyte sedimentation rate of 60 mm/h and C-reactive protein of 12. Rheumatoid factor, anti-CCP negative, FAN (HEp-2), ENA (Ro, La, RNP, Sm), anti-DNA and HLA-B27 negative, C3, C4 and angiotensin converting enzyme normal. Serologies for HIV, VDRL, HCV, HBV, EBV, CMV, parvovirus, chlamydia and Chagas negative. Chest X-ray and high-resolution tomography of the chest, abdomen and pelvis: normal. Magnetic resonance imaging of the brain with gadolinium: space-occupying lesion in the left selar region measuring 10 × 10 mm, with involvement of the cavernous sinus, where it encompasses the left internal carotid artery. A respected flow void was observed in the intracavernous internal carotid artery. Biopsy of conjunctival nodules: diagnosis of sarcoidosis (Fig. 1).
Clinical, imaging and pathological anatomical observations of hierarchy. A: Nodular conjunctival lesions on an erythematous base. B: Multiple rounded yellow-erythematous lesions, smaller than 2 mm in diameter. C: Biopsy of conjunctival nodules, showing non-caseating granulomas, compatible with sarcoidosis (red arrows) (courtesy of Dr Naves Ariel, Anatomic Pathology, Instituto de Histopatología, Rosario, Santa Fe, Argentina). D: Axial MRI with left selar space-occupying lesion (red arrow). E: MRI sagittal view, lesion of 10 × 10 mm, with involvement of the cavernous sinus, where it engulfs the left internal carotid artery (red arrows).
Since the onset of joint symptoms, treatment was with methotrexate, and subsequent addition of leflunomide. Following flare-up of the conjunctival lesions and arthritis and after diagnosis of sarcoidosis by biopsy, adalimumab was indicated. A marked improvement was observed after one week of treatment and complete remission after one month.
Ocular involvement in sarcoidosis occurs in up to 25% of patients, with ocular involvement being the form of presentation in less than 5%. The most common ocular involvement is uveitis and less frequently conjunctival, corneal, scleral, lacrimal and adnexal involvement (less than 40%). Conjunctival biopsy is a simple and useful procedure for patients with conjunctival nodules. A high index of suspicion is necessary for early diagnosis and treatment, preventing sequelae and improving the patient's quality of life1–8.
Conflict of interestsThe authors have no conflict of interests to declare.
Please cite this article as: Ringer A, Grossi DG, García Tentella B, Siegrist C. Sarcoidosis ocular conjuntival como primera manifestación de la enfermedad. Reumatol Clin. 2022;18:437–438.