To determine whether primary drug prevention of osteoporotic hip fracture is a useful measure in Catalonia and what would be their budgetary impact.
Materials and methodsWe performed a cost-utility social perspective study with a time horizon of 10–20 years. Univariate sensitivity analysis was performed. Doing nothing is compared with an intervention that includes screening for osteoporosis in women >64 years and in those diagnosed and who received treatment with generic alendronate for 10 years. Decision trees are developed for groups of 65–69, 70–74 and 75–79. HF data are from 2009 hospital discharges. Costs are derived from fees paid by public insurance.
ResultsIn 2009 there were 9262 HF. The direct cost was € 55 million (€ 5943.4/patient). The total cost was € 227 million for 10 years. The intervention dominates in all age groups in a 20-year perspective. In any horizon and age group, the different scenario puts the value per QALY below or within the proposed values for Spain. The budgetary impact is estimated at € 8.9 million which increased by 31% the actual direct cost, and 0.5% of the public pharmacy budget. Considering the total costs and the prospect of 20 years, annual savings of 7.4 million € were seen.
ConclusionsThe prevention of HF with alendronate in osteoporotic women >64 years is cost-useful in the long term (20 years) with a low budgetary impact in the 75–79 year group.
Determinar si la prevención farmacológica primaria de la fractura osteoporótica de cadera es una medida coste-útil en Cataluña y conocer cuál sería su impacto presupuestario.
Material y métodosSe realiza un análisis de coste-utilidad con perspectiva social y horizonte temporal de 10 y 20 años. Análisis de sensibilidad univariante. Se compara no hacer nada con una intervención que incluye el cribado de osteoporosis en mujeres > 64 años y, en las diagnosticadas, el tratamiento con alendronato genérico durante 10 años. Se elaboran árboles de decisión para los grupos de 65-69, 70-74 y 75-79 años. Los datos de FC provienen de las altas de 2009. Para los costes se utilizan las tasas pagadas por la aseguradora pública.
ResultadosEn 2009 hubo 9.262 FC. El coste directo fue de 55 millones de euros (5.943,4 €/paciente). El coste total es de 227 millones de euros en 10 años. La intervención domina en todos los grupos de edad en una perspectiva de 20 años. En cualquier horizonte y grupo de edad, los diferentes escenarios sitúan el valor por AVAC inferior o dentro de los valores propuestos para España. El impacto presupuestario se calcula en 8,9 millones de euros que incrementa en un 31% el coste directo actual, y en un 0,5% el presupuesto público de farmacia. Considerando los costes totales y la perspectiva de 20 años, el ahorro anual es de 7,4 millones de euros.
ConclusionesLa prevención de FC con alendronato en mujeres osteoporóticas > 64 años es coste-útil a largo plazo (20 años) con bajo impacto presupuestario en el grupo de 75-79 años.
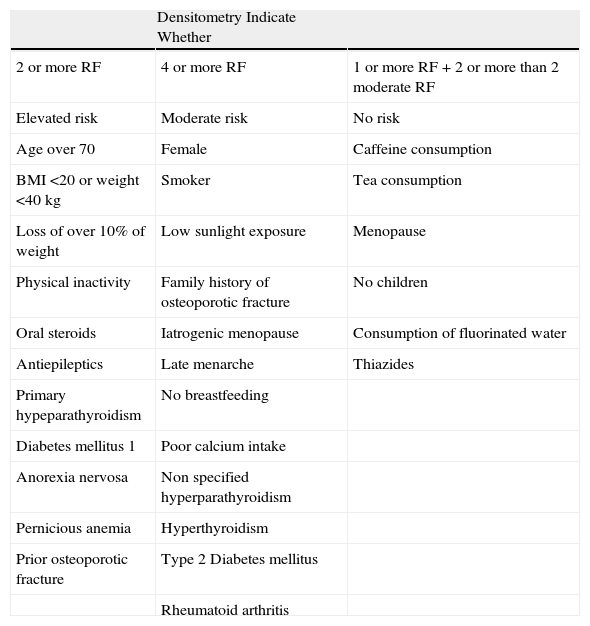
Osteoporosis is a metabolic bone disease characterized by low bone mass and microarchitectural deterioration of bone tissue leading to increased risk of fractures. The most common fractures are distal forearm, spine and hip fractures (HF). Catalonia is the region with the highest incidence of HF in Spain.1 According to the recorded minimum set of hospitalization database (MDS) of 2008,2 the fracture rate was 74.2 cases per 10,000 in persons over 64 years of age. HF usually occurs in older people and causes major economic costs and an even greater loss of quality of life.3 The diagnosis of osteoporosis can be performed by densitometry which should be performed only in those who have risk factors for osteoporosis. Among the different existing criteria, we selected the criteria proposed by the Agency of Information, Evaluation and Quality in Health in Catalonia (AIEHQC) collected in Table 1.4 These criteria were developed as a proposal of the Department of Health and are directed at health care professionals in our community. Alendronate is the drug of choice for osteoporosis and is effective in preventing vertebral and nonvertebral fractures, especially in women aged 70 years or older at high risk of fracture. The relative risk (RR) of HF in postmenopausal women after treatment with this bisphosphonate, with calcium and vitamin D (Ca+ DV), is 0.61 (level of evidence 1++ as indicated in a recent systematic review5). Treatment with bisphosphonates should be maintained for a minimum of about 5 years, stretching up to 7–10 years. Systematic review of economic studies conducted by García-Ruiz et al.5 shows that drug treatment of osteoporosis, especially with alendronate, is cost-effective for people with major risk factors: higher age, low bone density and a history of previous fractures. It is currently difficult to clearly define what is the cutoff age at which treatment should be started. Because drugs for treating osteoporosis can reduce the incidence of HF, the objective of this study was to determine the rate of HF in Catalonia and to determine whether primary drug prevention with alendronate for HF can be a measure implemented in our public health system based on cost-utility criteria, and which would counteract the diseases’ budgetary impact.
Densitometry Indication Criteria. AIEHQC.
| Densitometry Indicate Whether | ||
| 2 or more RF | 4 or more RF | 1 or more RF+2 or more than 2 moderate RF |
| Elevated risk | Moderate risk | No risk |
| Age over 70 | Female | Caffeine consumption |
| BMI<20 or weight <40kg | Smoker | Tea consumption |
| Loss of over 10% of weight | Low sunlight exposure | Menopause |
| Physical inactivity | Family history of osteoporotic fracture | No children |
| Oral steroids | Iatrogenic menopause | Consumption of fluorinated water |
| Antiepileptics | Late menarche | Thiazides |
| Primary hypeparathyroidism | No breastfeeding | |
| Diabetes mellitus 1 | Poor calcium intake | |
| Anorexia nervosa | Non specified hyperparathyroidism | |
| Pernicious anemia | Hyperthyroidism | |
| Prior osteoporotic fracture | Type 2 Diabetes mellitus | |
| Rheumatoid arthritis |
Source: Estrada et al.4
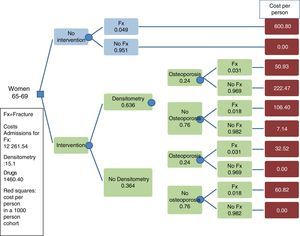
In the cost-utility analysis we compared 2 alternatives: the current strategy of “no prevention” versus the alternative “intervention” based on drug prevention in women aged 64 years or older diagnosed with osteoporosis by densitometry. A societal perspective was adopted and the time horizons considered were 20 and 10 years. We used a reduction rate of 5%. In the description of the budgetary impact we adopted the payer's perspective.
Description of AlternativesDescription of Current SituationIn 2009 there were 9262 hospital admissions of people over 64 due to HF in Catalonia, and 72.5% were female with a mean age of 80.8 years. The average stay was 12.5 days and 29.4% of cases were discharged to a geriatric hospital. Hospital mortality was 4.7%. Studies in our country estimate that about 30% of patients lose their autonomy and become dependent after FC.3
Description of the InterventionThe intervention proposed in this study consisted of an osteoporosis screening by densitometry in women 65 years or older who presented risk factors defined by the AIEHQC (Table 1). Women in whom osteoporosis was diagnosed were given generic alendronate (70mg per week) plus Ca+ vitamin D daily for 10 years.
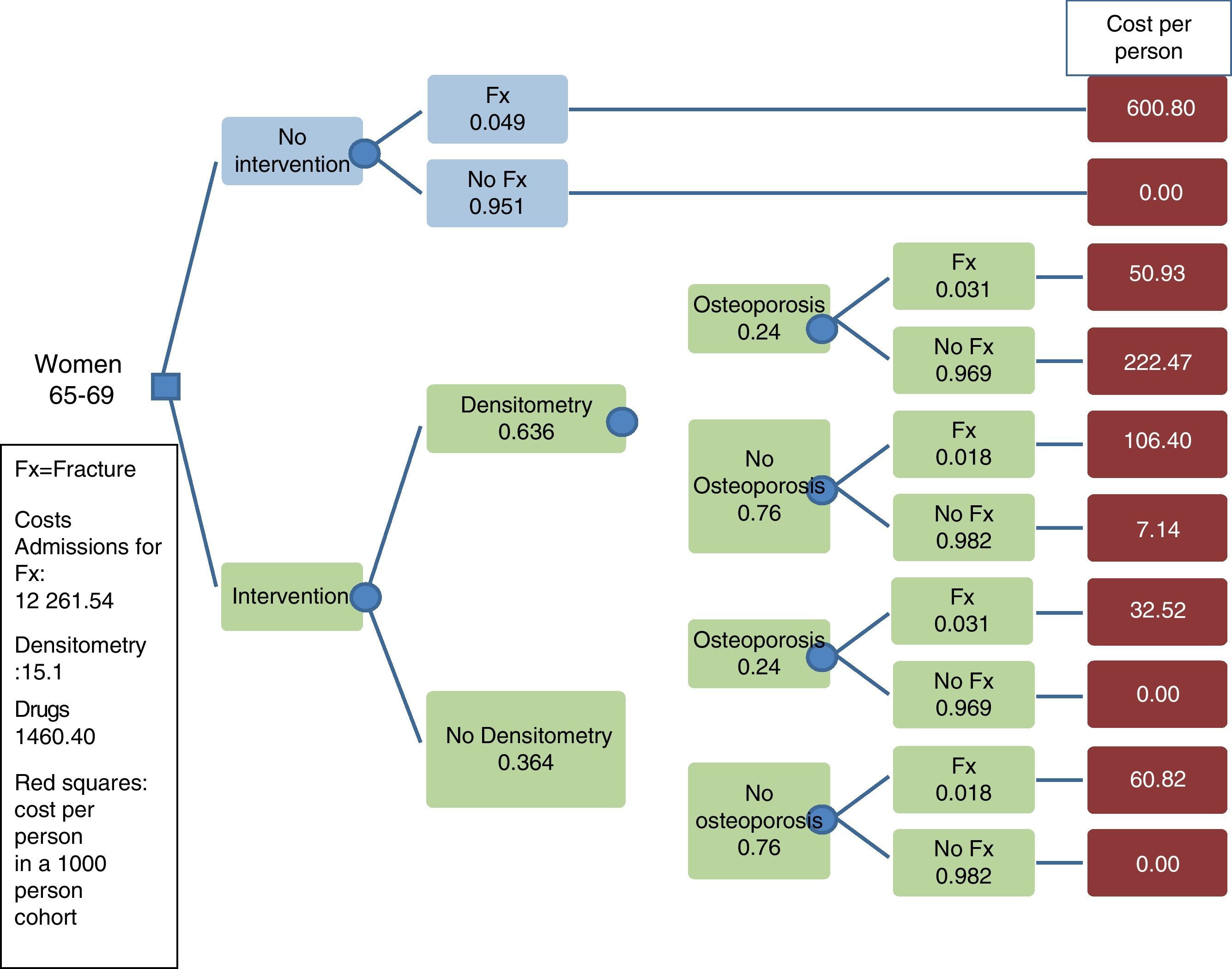
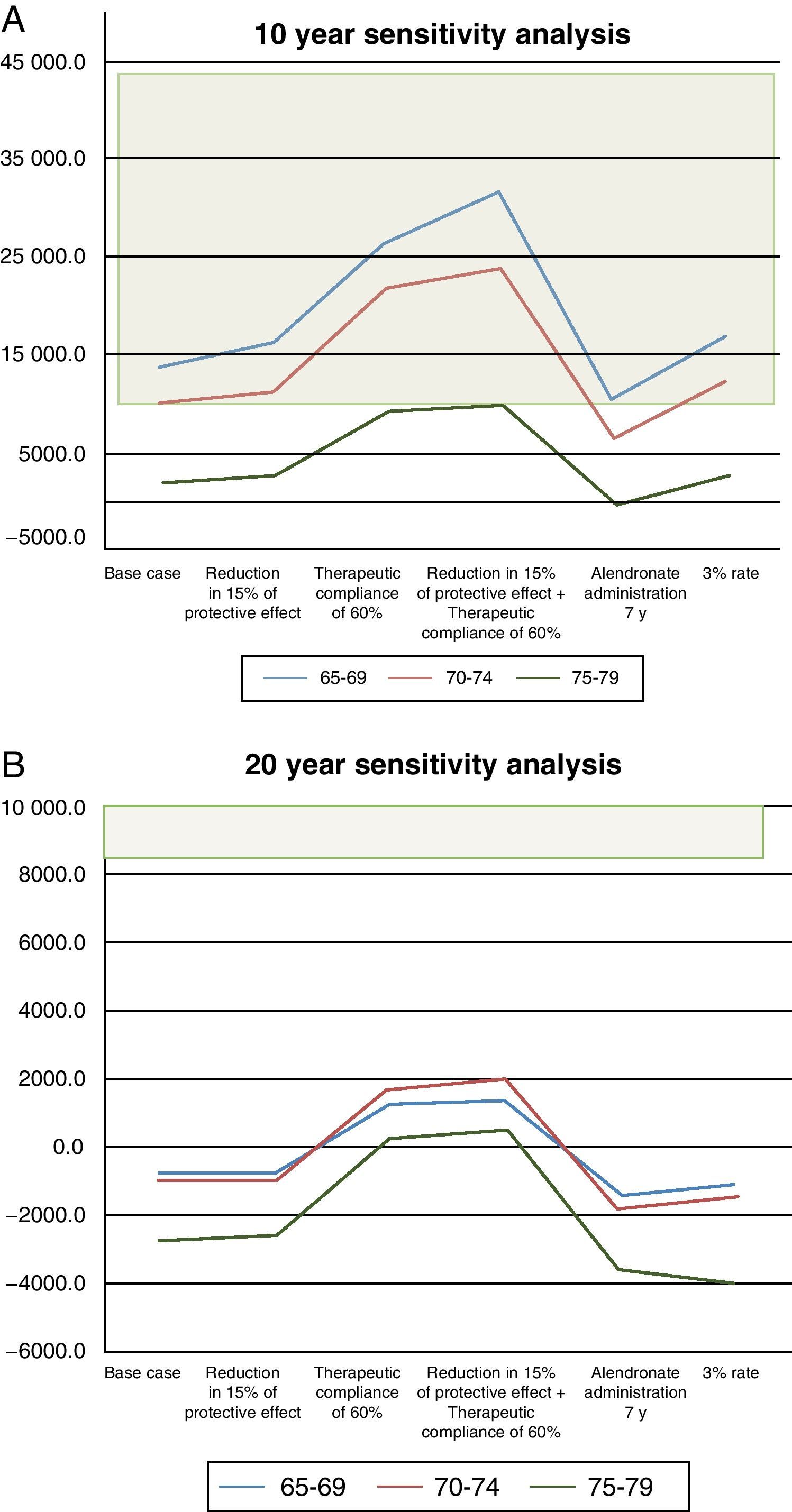
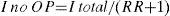
Base Case and Uncertainty AnalysisThe analysis was conducted in the following age groups: 65–69 years, 70–74 years and 75–79 years of age. For the base case we calculated a 100% compliance and a fracture risk reduction of 40% for the first year, with persistence of the effect during the 10 years of treatment. An example of a decision tree is presented in Fig. 1. In the uncertainty analysis we have considered the following scenarios:
- -
A decrease in compliance to 60%.
- -
A 15% reduction of the protective effect of alendronate at 10 years.
- -
Both effects.
- -
The administration of alendronate for 7 years with a fracture risk reduction of 15% in 10 and 20 years.
- -
A reduction rate of 3%.
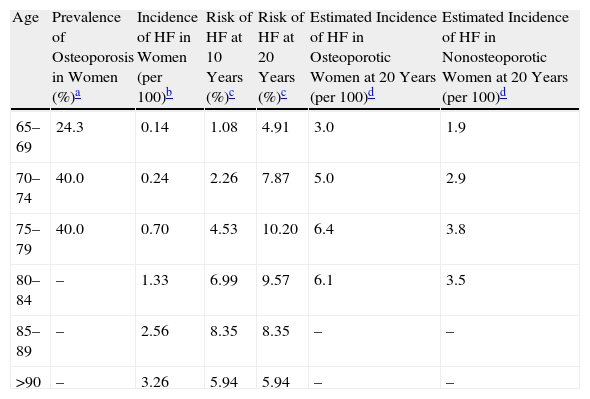
The prevalence of osteoporosis in the Spanish female population, measured by axial densitometry,6 and the incidence of HF are shown in Table 2. Among women over 64 years of age with osteoporosis, the fracture RR is 1.7 (95% CI, 1.4–2.2).7 The distribution of HF between osteoporotic and non-osteoporotic women (Table 2) was calculated using the following formulas:
Prevalence of Osteoporosis by Axial Densitometry as Determined in Spanish Women; Incidence of HF in Women (2009) Based on Hospital Admission Records; Risk of HF in Women ≥65 Years at 10 and 20 Years and Estimated HF Distribution in Osteoporotic and Nonosteoporotic Women (Adopting an RR of 1.7).
| Age | Prevalence of Osteoporosis in Women (%)a | Incidence of HF in Women (per 100)b | Risk of HF at 10 Years (%)c | Risk of HF at 20 Years (%)c | Estimated Incidence of HF in Osteoporotic Women at 20 Years (per 100)d | Estimated Incidence of HF in Nonosteoporotic Women at 20 Years (per 100)d |
| 65–69 | 24.3 | 0.14 | 1.08 | 4.91 | 3.0 | 1.9 |
| 70–74 | 40.0 | 0.24 | 2.26 | 7.87 | 5.0 | 2.9 |
| 75–79 | 40.0 | 0.70 | 4.53 | 10.20 | 6.4 | 3.8 |
| 80–84 | – | 1.33 | 6.99 | 9.57 | 6.1 | 3.5 |
| 85–89 | – | 2.56 | 8.35 | 8.35 | – | – |
| >90 | – | 3.26 | 5.94 | 5.94 | – | – |
As I OP the incidence in women with osteoporosis and I no incidence of OP in osteoporotic women.
Risk of Hip FractureThe likelihood of having a HF in the next 10–20 years (Table 2) was calculated with the Cutler–Ederer8 formula:
As the incidence Ia and In are the period of the incidence in the period n.Indication of DensitometryAccording to Roig-Vilaseca et al.,9 densitometry was indicated in 63.6% of women aged 65 years or older who attended primary health care centers if the criteria proposed by the AIEHQC were adopted.
MortalityIn addition to in-hospital mortality, in the first year after the fracture the mortality rate increased to 30%.10 However, in our model it is assumed that after the first year, the mortality rate is the same as the corresponding age group according to the Register of Deaths in Cataluña.11
Loss of Personal Autonomy (State Dependence)About 50% of patients with HF have important disability.12 We adopted the figure of 45% found in one Barcelona13 study and 30% for a long-term3 situation.
UtilityTo calculate the adjusted quality of life years (QALYs), the values used were taken from a recent review,14 i.e. 0.797 for the first year after the fracture and 0.899 for the following years. The usefulness in those that have failed to present a fracture is considered to be 1, regardless of age group, to compare changes in QALYs due only to the intervention. We used a reduction rate of 5%.
Cost VariablesDirect Costs of the Current SituationDirect costs include visit to the emergency room, admissions to hospital, the stay of some patients in a geriatric hospital, outpatient visits and 4 control visits without added tests (or densitometry).15 The costs are calculated on the basis of the rates (hospital discharge or stay), paid by the public insurer.16 In cases where rates vary by type of hospital, we used the average of the rates. The estimated cost per stay has been multiplied by the average stay and the number of patients in order to obtain the total cost.
Indirect Costs of the Current SituationWe did not consider the costs associated with lost work productivity because we dealt with a retirement age population. In the study of the costs associated with a situation of dependency we considered severe dependency status in 30% of patients.17 Montserrat18 calculated the costs of the status of severe dependency, including the cost of health and social assistance, at € 9805.94 (value 2003). Without the direct health costs, such costs to date (3% per year) are € 8429.1. It was considered that the life expectancy of people in a situation of dependency is 7.7 years,19 regardless of age group.
Direct Costs of the Proposed InterventionDirect costs include densitometry for women with risk factors, an annual visit to primary care and drug treatment. The cost (list price of generic alendronate in 2010), updated drug treatment and annual monitoring is € 1460.4 per person treated (in 20 years and with a reduction rate of 5%).
Cost per Year of Quality-adjusted LifeSince there is no consensus on the cost per QALY in our country, we adopted the range of values per QALY proposed by Abellán et al.,20 which for 2010 is between € 9200 and € 44 000. Differences in costs and QALYs were calculated for 1000 women, with 1000 women interventions versus no intervention.
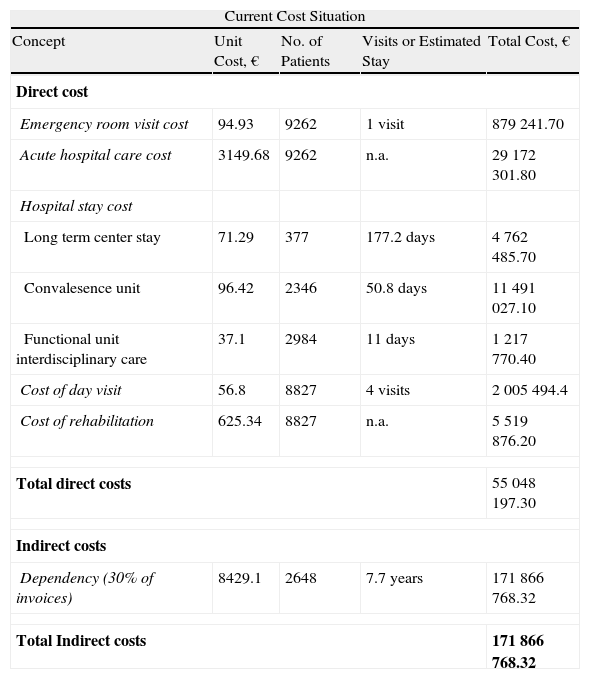
ResultsTotal Direct CostsThe total direct costs of hospitalized patients in 2009 was € 55 048 197.3 (Table 3), representing € 5943.4 per patient. With a time horizon of 20 years and a reduction rate of 5%, the current value per patient was approximately € 2240.0. Total costs (direct and indirect) over a period of 10 years was € 226 914 965.53, which account for € 9233.63 per person over 20 years with a 5% reduction (Table 3).
Direct and Indirect Current Costs of HF in Cataluña (2009) and Direct Costs of the Proposed Intervention.
| Current Cost Situation | ||||
| Concept | Unit Cost, € | No. of Patients | Visits or Estimated Stay | Total Cost, € |
| Direct cost | ||||
| Emergency room visit cost | 94.93 | 9262 | 1 visit | 879 241.70 |
| Acute hospital care cost | 3149.68 | 9262 | n.a. | 29 172 301.80 |
| Hospital stay cost | ||||
| Long term center stay | 71.29 | 377 | 177.2 days | 4 762 485.70 |
| Convalesence unit | 96.42 | 2346 | 50.8 days | 11 491 027.10 |
| Functional unit interdisciplinary care | 37.1 | 2984 | 11 days | 1 217 770.40 |
| Cost of day visit | 56.8 | 8827 | 4 visits | 2 005 494.4 |
| Cost of rehabilitation | 625.34 | 8827 | n.a. | 5 519 876.20 |
| Total direct costs | 55 048 197.30 | |||
| Indirect costs | ||||
| Dependency (30% of invoices) | 8429.1 | 2648 | 7.7 years | 171 866 768.32 |
| Total Indirect costs | 171 866 768.32 | |||
| Direct Costs of Intervention | ||||
| Concept | Unit Cost, € | No. | Total, € | Value per Patient Treated*, € |
| Densitometry cost | 40 | 1 | 40 | 15.4 |
| Monthly generic alendronate (70mg/week) for 10 years | 15.42 | 120 months | 1850.40 | 697.40 |
| Monthly cost Ca+ vitamin D (daily administration) | 10.55 | 120 months | 1266.00 | 477.10 |
| Cost of annual visits to primary care | 37.9 | 20 visits | 758.40 | 285.80 |
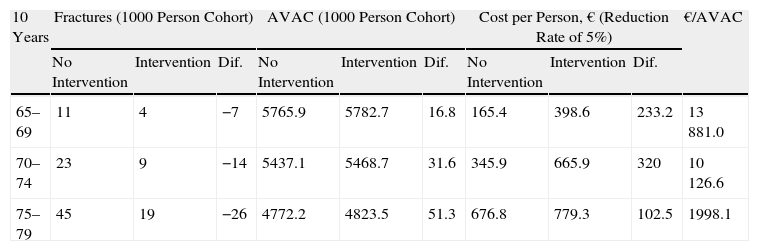
Table 4 shows the differences in the number of fractures and in costs, QALYs and costs per QALY in the different age groups considering a 40% reduction in fracture risk. In a time horizon of 20 years, the intervention is dominant in all age groups and cheaper than non-intervention.
Number of Fractures, AVAC, Cost Per Person and Per AVAC in a Cohort of 1000 Women With and Without Intervention and a 10 and 2 Year Time Horizon.
| 10 Years | Fractures (1000 Person Cohort) | AVAC (1000 Person Cohort) | Cost per Person, € (Reduction Rate of 5%) | €/AVAC | ||||||
| No Intervention | Intervention | Dif. | No Intervention | Intervention | Dif. | No Intervention | Intervention | Dif. | ||
| 65–69 | 11 | 4 | −7 | 5765.9 | 5782.7 | 16.8 | 165.4 | 398.6 | 233.2 | 13 881.0 |
| 70–74 | 23 | 9 | −14 | 5437.1 | 5468.7 | 31.6 | 345.9 | 665.9 | 320 | 10 126.6 |
| 75–79 | 45 | 19 | −26 | 4772.2 | 4823.5 | 51.3 | 676.8 | 779.3 | 102.5 | 1998.1 |
| 20 Years | No Intervention | Intervention | Dif. | No Intervention | Intervention | Dif. | No Intervention | Intervention | Dif. | €/AVAC |
| 65–69 | 49 | 20 | −29 | 6118.1 | 6192.6 | 74.5 | 452.4 | 395.3 | −57.1 | −766.4 |
| 70–74 | 79 | 35 | −44 | 5020.1 | 5113.5 | 93.4 | 726.7 | 635.7 | −91 | −974.3 |
| 75–79 | 102 | 45 | −57 | 3526.5 | 3611.3 | 84.8 | 941.8 | 711.9 | −229.9 | −2711.1 |
The results of this analysis are shown in Fig. 2. In the 10-year time horizon, all scenarios would be acceptable, since the values are below the 44 000 €/QALY proposed for Spain. In the 75–79 year group, values fall below € 9200, which is the lowest limit suggested. With a 20-year perspective, the intervention is dominant in the 75–79 years of age group if the reduced risk of fracture is at least 15%. All other scenarios are acceptable in all age groups, as the QALY values do not exceed € 3000.
Budget Impact AnalysisWe estimated the cost of implementing preventive intervention in 2 age groups: ≥65 and 75–79 years (Table 5). In the next 10 years the population of women over 64 years will be approximately about 750,000 with an average annual income, if no intervention is performed, of 6911 a year, which will provide direct costs of about 41.1 and total costs of 165.5 million euros. The average annual direct cost of intervention in the ≥65 year age group and in the 75–79 year group would be about 63.4 and 38.2 million euros, respectively, for the next 10 years. The balance between the direct costs of the intervention and the costs of non-intervention, if prevention is performed in women over 65 for 10 years, would increase 34.2 million a year on average. Considering the total costs, the increase is 10.9 million. The balance of direct costs, for prevention in women 75–79 years for 10 years, showed an increase of 8.9 million per year on average. When considering the total costs, the balance is more favorable, since the intervention represents an annual saving of about 7.4 million. Considering only the perspective of the insurer, the above figure of 8.9 million represents an increase of 31% per annum of the actual cost of the HF, although the overall public drug budget21 does not reach a 0.5% increase.
Budget Impact of the Intervention in a Cohort of Women ≥65 and 75–79 Years of Age Comparing It With No Intervention.
| ≥65 Years | 75–79 Years | |
| No intervention | ||
| Number of women≥65 | 751 243 | |
| HF hospitalizations expected in women≥65 | 6757 | |
| Direct hospitalization costs (millions of €) | 29.2 | |
| Total costs (direct+indirect) (millions of €) | 165.5 | |
| Intervention | ||
| Persons under treatment | 140 000 | 53 000 |
| Costs of care and densitometry (millions of €) | 41.6 | 14.2 |
| Expected avoided hospitalizations | 1839 | 1268 |
| Direct costs (hospitalizations+treatment) (millions of €) | 63.4 | 38.2 |
| Total costs (millones €) | 160.9 | 113.1 |
| Balance (intervention-no intervention) | ||
| Balance of direct costs (millions of €)* | 34.2 | 8.9 |
| Balance of total costs (millions of €)* | 10.9 | −7.4 |
Drug prevention of HF is more efficient and cheaper than the option of doing nothing in the female population over 64 years, from a social and long-term perspective (20 years). Adopting the social22,23 perspective is based on the need to ensure that the use and distribution of public resources is done efficiently and with reasoned and transparent criteria. This justifies the use of QALYs as the unit of measure. The incorporation of the costs associated with a state of dependence due to FC can multiply the cost of HF 4, while a preventive policy proposal allows a saving of between 766.7 and € 2711.1 per QALY gained, depending on the age group. The incorporation of these costs has previously justified the application of some health policies in Catalonia for the acute care of stroke.24,25 In the 10-year time horizon, the intervention is effective but more expensive in the three age groups, although the costs obtained per QALY (13,881 for the 65–69 year group, 10,126 for the 70–74 group and 1988 the 75–79 year group) are within the recommended range of values. Moreover, the cost per QALY, especially in those aged 75–79, is not far from the values of other procedures prioritized in Catalonia, such as knee replacement surgery (€ 1353.5/QALY) or the hip replacement surgery (€ 8419.4/QALY values of 2010).26 The results are similar to those of other studies of cost-effectiveness. The cost per QALY gained in Germany from the strategy of screening and treatment of osteoporosis with alendronate27 was highest in women 60–70 years of age (€ 16589/QALY), reaching up to € 2337/QALY in the group of 80–89 years. The study by Kanis et al.28 demonstrated that primary prevention is cost-effective in women aged 50 years, lowering the cost of QALY progressively from age 60 and remaining dominant in the ≥80 years of age group. The proposed intervention involves nearly a 31% increase in current spending, but would not involve more than 0.5% of the total drug budget of the public insurer. Both the low cost per QALY as well as its small budgetary impact could justify the introduction of this preventive intervention in the 75–79 years of age group of women. The introduction of this measure, to be feasible, should be managed from primary care, as would be the appropriateness of prescribing bisphosphonates to the target population, avoiding unwarranted treatments. One limitation of the study is the criterion for the selection of persons at risk of osteoporosis. Shortly after the completion of our study, a publication appeared, which predicted that the positive predictive value of AIEHQC criteria for low bone density is 58.97% for women over 65 years of age, while the negative predictive value is high.29 The likelihood of osteoporosis that we have adopted is the same in the group with densitometry than in the group without; therefore overestimating fractures in the group without making densitometry analysis results are more robust. The upcoming availability of screening tools based on the absolute risk of osteoporotic fracture, and validated in our population, will improve the efficiency of the preventive strategy. In this sense, the FRAX® index (available in http://www.shef.ac.uk/FRAX/) which helps calculate the risk of fracture, may be an easily performed and useful tool.30 Another methodological limitation is the simplicity of the analysis employed, mainly based on point estimates of five-year age groups, the assumption of a linear increase (not exponential) of HF risk and uncertainty management through univariate sensitivity. However, it is assumed that the introduction of an exponential risk, the risk of a HF and transitional probabilities associated with age, would result in a greater number of fractures and greater cost-utility of preventive policy than has been analyzed. In summary, primary prevention of HF with alendronate plus Ca+ and vitamin D in women ≥65 years of age with osteoporosis is an intervention that has a long-term cost-utility (time horizon of 20 years). Within 10 years, the intervention in the group of women 75–79 years shows annual savings that reach 7.4 million euros on average, taking into account the total costs. The measure in that age group would have a budgetary impact on the public insurer.
Ethical disclosuresProtection of human and animal subjects. The authors declare that no experiments were performed on humans or animals for this investigation.
Confidentiality of Data. The authors declare that no patient data appears in this article.
Right to privacy and informed consent. The authors declare that no patient data appears in this article.
AuthorshipMary J. Antonio Pueyo and J. Garcia-Ruiz developed the study design, analyzed the data and drafted the manuscript. Marta Larrosa Xavier Surís contributed to the idea of the project and the manuscript.
Conflict of InterestThe authors declare no conflict of interest.
We thank Dr. M. de la and Elena for their support for the realization of the International Master's Degree in Health Economics and Pharmacoeconomics (on line), 11th edition, from which the thesis that underlies this manuscript emerged.
Please cite this article as: Pueyo MJ, et al. Análisis de coste-utilidad e impacto presupuestario de la prevención primaria con alendronato de la fractura osteoporótica de cadera en Cataluña. Reumatol Clin. 2012;8:128–34.