Pilomatrixoma (PM), pilomatricoma or calcifying Malherbe's epithelioma are benign skin tumors derived from the hair follicles. They usually occur in children and adolescents as a single tumor in the upper body and their etiology is unknown. In this regard, it has been described in association with multiple trauma and disease, with no clear causal relationship.1 We report the first case of a child diagnosed with juvenile idiopathic arthritis (JIA) who developed a PM in the puncture site of subcutaneous methotrexate administration and we review the literature in this regard.
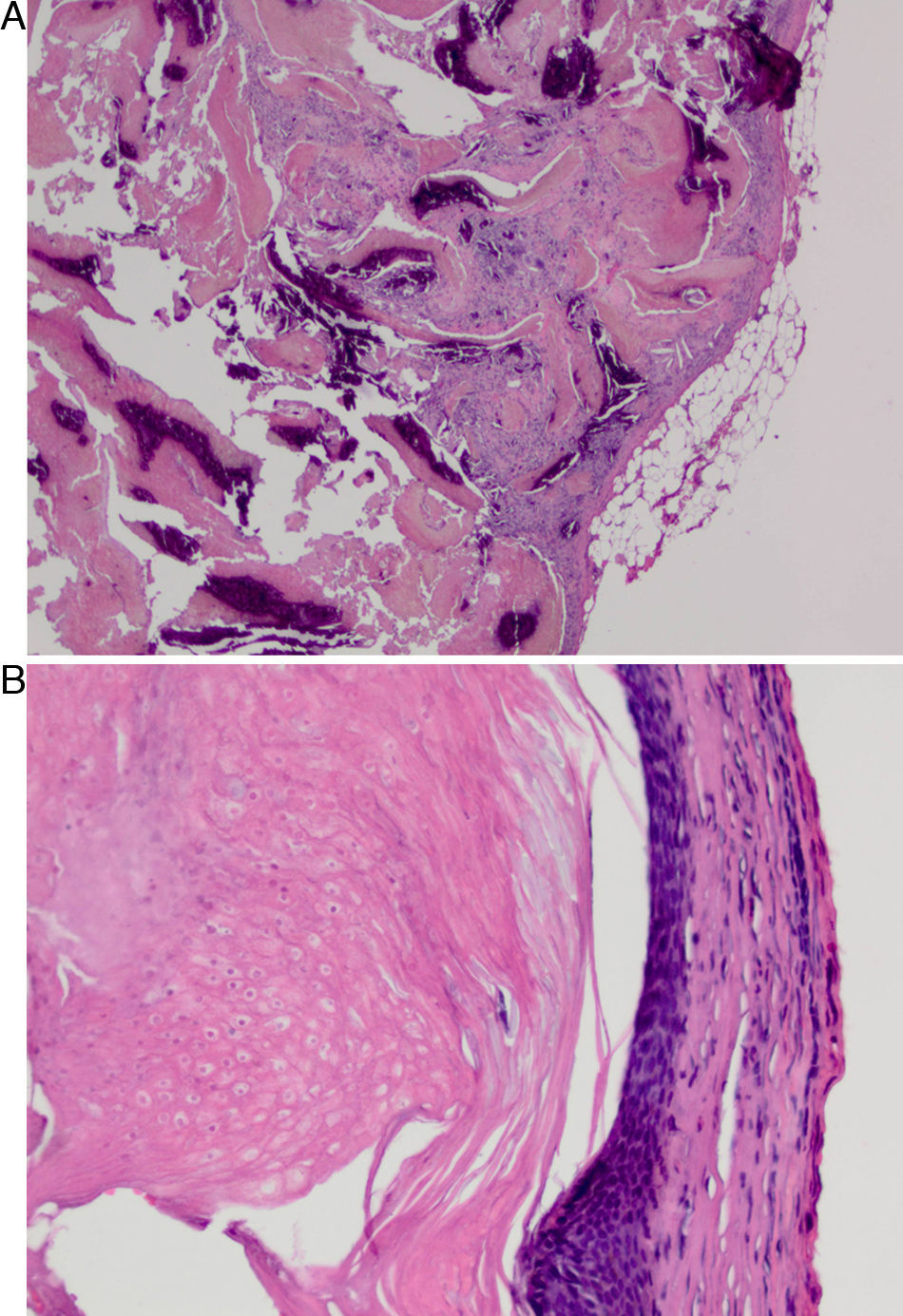
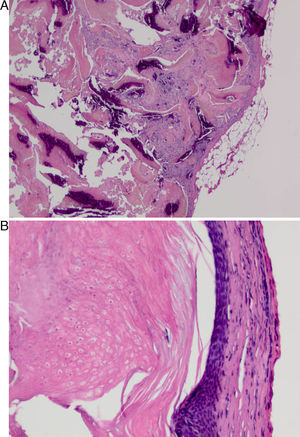
The patient, a girl, was diagnosed in 2007 with JIA at 3 years of age due to the presence of idiopathic chronic monoarthritis and with her father presenting Psoriasis. She had been treated with local infiltration of corticosteroids on 2 occasions and then, due to the persistence of disease activity, was prescribed weekly subcutaneous methotrexate in 2008. Currently, the patient is 7 years old and is on weekly subcutaneous methotrexate (15mg/0.3ml), being clinically asymptomatic and performing a normal life. After the last administration of subcutaneous methotrexate she presented a nodular cystic lesion. The lesion was treated with local cold, without improvement. Subsequently, it increased in size and consistency, becoming harder and painful upon palpation. On examination she had a hard, subcutaneous injury and uneven surface on the lateral aspect of the left arm, about 2cm in diameter, painful on palpation, not adhered to deep planes and covered with purplish skin. We conducted a consultation with Dermatology upon the suspicion of a foreign body reaction versus PM, who decided to excise the tumor and send it for pathologic examination. Pathology confirmed the diagnosis of PM (Fig. 1A and B).
(A) A well-defined, non-encapsulated tumor of the hair matrix. Cell proliferation in the lobes distinguished aspect formed by basaloid cells, keratinization and dystrophic calcifications (hematoxylin–eosin). (B) Under more detail we observed basophilic epithelioid cell proliferation suffering abrupt keratinization and presence of eosinophilic bodies called ghost cells (hematoxylin–eosin).
The PM is a well-circumscribed benign tumor located in the lower dermis and which extends into the subcutaneous tissue. It consists of irregular islands of epithelial cells, a basophilic stain located in the periphery with scant cytoplasm and hyperchromatic nuclei and other eosinophilic bodies called “ghost or shadow cells” whose nucleus does not stain. The stroma shows a foreign body reaction with giant cells, foci of calcification and ossification.2 In 2005 there was one case of PM in relation to BCG vaccination.3 Subsequently, Malpathak et al. described the formation of a giant PM after intramuscular injection. In this case, the authors postulated that local trauma and hematoma development could lead to suppression of apoptosis and thus the formation of the PM.4 Our case shows a clear temporal relationship with the subcutaneous injection of methotrexate, a fact not mentioned in the literature. The trauma caused by puncturing the skin or injecting fluid could act as a trigger factor favoring the development of PM. The increased use of different subcutaneous therapies in JIA should alert physicians treating these patients for the development of PM.
Please cite this article as: Afonso Pérez E, et al. Desarrollo de pilomatrixoma tras la inyección subcutánea de metotrexato en el tratamiento de la artritis idiopática juvenil. Reumatol Clin. 2012. http://dx.doi.org/10.1016/j.reuma.2012.05.009