TNF-α plays a role in the induction and maintenance of inflammation in autoimmune disease, hence the TNF-α inhibitors are used successfully in the control of certain systemic diseases or autoinmunitarias.1
Uveitis is an intraocular inflammation-associated to autoimmune systemic diseases, in which effectively blocking TNF-α2 constitutes one of the most important advances in recent years in the treatment of non-infectious uveitis.
The different anti-TNF-α agents do not have the same efficacy on ocular2 inflammation and 3 major questions remain to be resolved (when to initiate therapy with an agent, at what dose, duration, etc.).2 Changing biologic therapy works in some cases.4
We report the case of a patient with idiopathic uveitis, papillitis, and EMQ, who after 1 year of treatment with prednisone, cyclosporine, azathioprine, and infliximab had no improvement and underwent a change in anti-TNF-α treatment to adalimumab, achieving a major clinical response within 2 months.
In July 2009, a 58-year-old male came to the office complaining of pain in the right eye. Ophthalmologic examination showed Tyndall sign (+), vitritis (++), papillitis with periphlebitis around the papilla, and cystoid emerging macular edema (CME) with visual acuity (VA) of 0.5. The anamnesis for connective tissue disease and spondyloarthritis was negative and the analytical studies had not relevant findings, with negative HLA-B27. The first treatment was transeptal infiltration with triamcinolone acetonide, cyclosporine (5mg/kg/day), and prednisone (60mg/day). In August the patient presented a respiratory infection that required hospitalization, so we discontinued cyclosporine and prednisone was reduced (30mg/day).
In January 2010 the treatment was changed to azathioprine (100mg/day), prednisone (40mg/day), and infliximab (5mg/kg/day, weeks 0, 2, 6, and then every 8 weeks). No improvement was seen and by April 2010 treatment with infliximab was reduced to a dose every 4 weeks, and azathioprine was increased to 150mg/day.
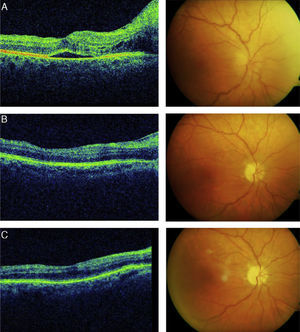
In August 2010, the patient still had pain, papillitis, and EMQ (Fig. 1A) and 0.2 of VA, so we switched the anti-TNF-α to adalimumab (40mg/s every 2 weeks) maintaining azathioprine. After a month with this treatment the VA improved to 0.4 and the pain disappeared. At 2 months, papillitis decreased (Fig. 1B), and AV reached 0.5. In December 2010 the patient remained stable (Fig. 1C) with adalimumab treatment and azathioprine (100mg/day).
There is some evidence that not all anti-TNF-α have the same efficacy in the treatment of uveítis.2 Etanercept (a p75 TNF-α receptor and human IgG Fc fusion protein) has demonstrated efficacy in treating uveítis2,3,5; however, infliximab (chimeric monoclonal antibody) and adalimumab (monoclonal human antibody) may be effective in the treatment of refractary2–9 uveitis. There is no comparative data to support the superiority of one antibody over the other, and influencing this choice we find, among others, the route of administration and patient10 preference. In case of an absence of response to anti-TNF, which can be seen, among others, with infliximab due to antichimeric antibodies, switching to a second anti-TNF antibody may be effective as has been observed in other inflammatory diseases.
This case shows that adalimumab is an effective drug in the treatment of uveitis refractory to conventional treatment, even in cases that did not respond to other anti-TNF-α. Therefore, the first choice of anti-TNF-α did not produce satisfactory effects after a few months, and the best option was to change the anti-TNF-α.
Please cite this article as: González-Suárez S, et al. Resolución de uveítis refractaria, cambiando el tratamiento anti-TNF. Reumatol Clin. 2012. http://dx.doi.org/10.1016/j.reuma.2012.02.005.