Categorization of patients diagnosed with ocular sarcoidosis during the period 2009–2014.
MethodsThe medical records of patients with ocular sarcoidosis were reviewed and variables were collected to categorize the patients according to the criteria of the FIWOS.
ResultsWe found 11 patients, 7 women and 4 men, with sarcoid uveitis; the median age was 58 years. Bilateral panuveitis was the most common pattern (54.5%), followed by chronic anterior uveitis (27.2%). The diagnosis of sarcoidosis was definitive in 4 patients (36.3%), presumed in 5 (45.4%), probable in 1 (9%) and possible in 1 (9%).
ConclusionsOcular sarcoidosis was diagnosed in more than half of the patients who had no confirmatory biopsy. Bilateral panuveitis and chronic anterior uveitis were the patterns most frequently observed.
Categorizar a los pacientes con diagnóstico de sarcoidosis ocular en el período comprendido entre 2009 y 2014.
MétodosSe revisaron las historias clínicas de los pacientes con sarcoidosis ocular y se recopilaron las variables para categorizar a los pacientes según los criterios del FIWOS.
ResultadosSe encontró a un total de 11 pacientes con uveítis sarcoidea, 7 mujeres y 4 hombres, con una mediana de edad de 58 años. El patrón de panuveítis bilateral crónica fue el más frecuente en un 54,5%, seguido de la uveítis anterior crónica unilateral, con 27,2%. El diagnóstico de sarcoidosis fue definitivo en 4 pacientes (36,3%), presunto en 5 pacientes (45,4%), probable en un paciente (9%) y posible en un paciente (9%).
ConclusionesMás de la mitad de los pacientes sin biopsia confirmatoria fueron diagnosticados de sarcoidosis ocular. La panuveítis bilateral crónica y la uveítis anterior crónica fueron los patrones predominantes.
Sarcoidosis is a multisystem disorder of unknown cause, characterized by noncaseating granulomatous inflammation.1 It affects the parenchyma of almost any organ, and thoracic symptoms are those most frequently observed. Overall, 30%–60% of the patients have eye involvement. It is usually bilateral uveitis, although, uveitis can occasionally develop in the absence of systemic disease, or could be the predominant manifestation with no significant extraocular impact.2–4 In clinical practice, the diagnosis of systemic sarcoidosis is based on the combination of clinical, radiographic and histopathological findings. The diagnostic criteria proposed by the First International Workshop on Ocular Sarcoidosis (FIWOS) were recently validated.5 These criteria classify ocular sarcoidosis as definite (uveitis and positive biopsy), presumed (bilateral hilar lymphadenopathy and uveitis without biopsy), probable (3 ocular signs and 2 laboratory findings without biopsy or bilateral hilar lymphadenopathy) and possible (4 ocular signs and 2 laboratory findings with a negative biopsy), in accordance with specific ophthalmological and laboratory findings.6 The latter are especially useful when there is no biopsy or the biopsy is negative.
ObjectivesThe purpose was to categorize those patients with a diagnosis of ocular sarcoidosis from 2009 to 2014 in Hospital Universitario Donostia, in the province of Guipúzcoa in northern Spain, using the diagnostic and validated criteria of the FIWOS.
Material and MethodsWe retrospectively reviewed the case reports of the patients diagnosed with ocular sarcoidosis. The diagnosis of sarcoidosis was based on a combination of the clinical, radiographic and histological criteria of the FIWOS, as well as the exclusion of other granulomatous diseases like tuberculosis.
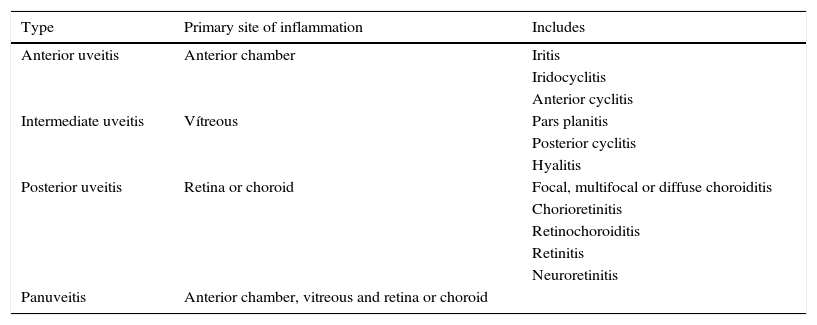
The variables recorded were patient age and sex, presence of systemic manifestations, anatomical location of the inflammation, tuberculosis screening, positive test for angiotensin-converting enzyme, lymph node biopsy, chest radiographic findings and treatment. To classify uveitis we used the anatomical classification of the Standardization of Uveitis Nomenclature (SUN) Working Group7 (Table 1). We excluded patients who had a positive result on the Quantiferon® test. Using these findings, we categorized the patients according to the FIWOS.
Anatomical Classification of Uveitis (Sun Working Group, 2005).
| Type | Primary site of inflammation | Includes |
|---|---|---|
| Anterior uveitis | Anterior chamber | Iritis |
| Iridocyclitis | ||
| Anterior cyclitis | ||
| Intermediate uveitis | Vítreous | Pars planitis |
| Posterior cyclitis | ||
| Hyalitis | ||
| Posterior uveitis | Retina or choroid | Focal, multifocal or diffuse choroiditis |
| Chorioretinitis | ||
| Retinochoroiditis | ||
| Retinitis | ||
| Neuroretinitis | ||
| Panuveitis | Anterior chamber, vitreous and retina or choroid |
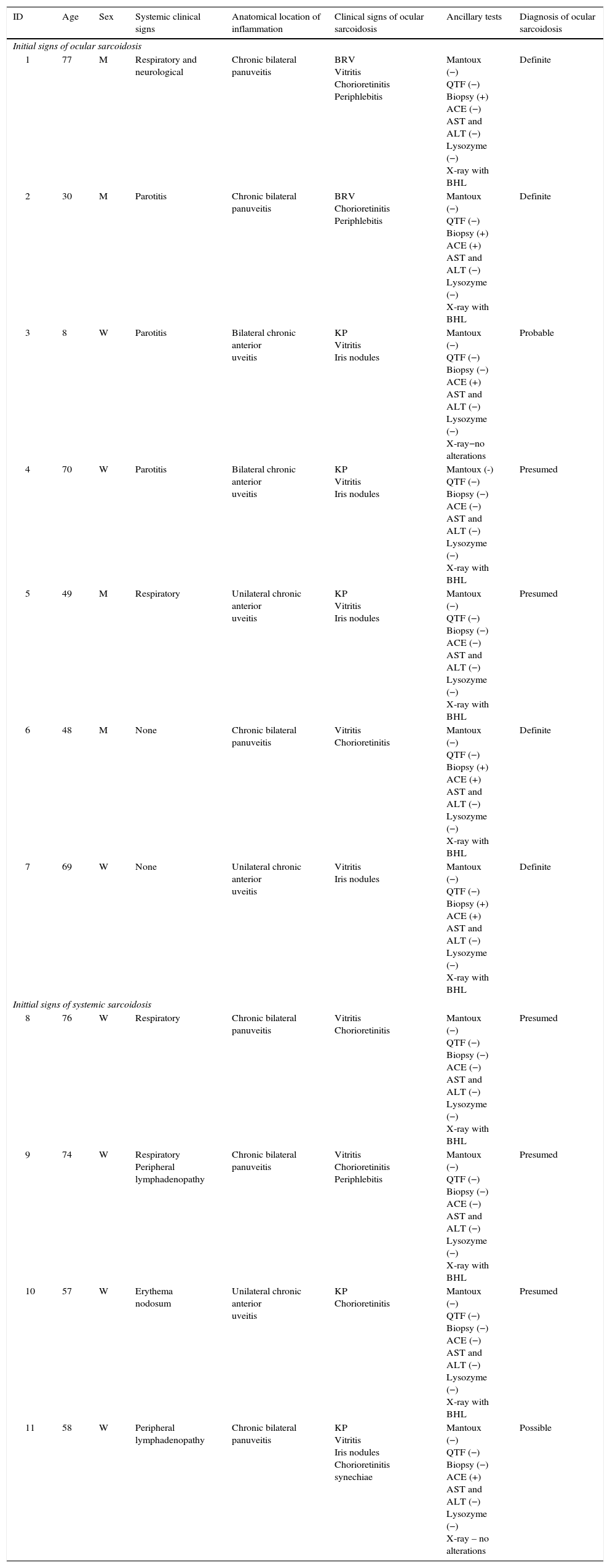
We found a total of 11 patients with a diagnosis of sarcoid uveitis, 7 women (63.6%) and 4 men (36.3%). The median age±standard deviation was 58±20.5 years. In 7 patients (63.6%), the eye was the first organ to be affected: 5 of them later developed the systemic clinical signs and 2 had only ocular clinical features. Four patients (36.3%) began with extraocular systemic manifestations, which, in order of frequency, were: bilateral hilar lymphadenopathy in 81.8%, respiratory manifestations in 36.3%, peripheral lymphadenopathy in 18.1%, parotitis in 27.2% and erythema nodosum in 9%. The locations of inflammation most frequently observed were chronic bilateral panuveitis in 54.5%, unilateral chronic anterior uveitis in 27.2% and bilateral chronic anterior uveitis in 18.1%. When the patients were categorized, 4 (36.3%) had a definite diagnosis of sarcoidosis, 5 patients (45.4%) had a presumed diagnosis, 1 patient (9%) had a probable diagnosis and 1 patient (9%) had a possible diagnosis of sarcoidosis.
Table 2 shows the above-mentioned variables in the patients diagnosed with ocular sarcoidosis.
Demographic and Clinical Characteristics, Anatomical Location of Uveitis, Signs of Ocular Sarcoidosis, Ancillary Tests, Diagnosis and Treatment of the Series Presented.
| ID | Age | Sex | Systemic clinical signs | Anatomical location of inflammation | Clinical signs of ocular sarcoidosis | Ancillary tests | Diagnosis of ocular sarcoidosis |
|---|---|---|---|---|---|---|---|
| Initial signs of ocular sarcoidosis | |||||||
| 1 | 77 | M | Respiratory and neurological | Chronic bilateral panuveitis | BRV Vitritis Chorioretinitis Periphlebitis | Mantoux (−) QTF (−) Biopsy (+) ACE (−) AST and ALT (−) Lysozyme (−) X-ray with BHL | Definite |
| 2 | 30 | M | Parotitis | Chronic bilateral panuveitis | BRV Chorioretinitis Periphlebitis | Mantoux (−) QTF (−) Biopsy (+) ACE (+) AST and ALT (−) Lysozyme (−) X-ray with BHL | Definite |
| 3 | 8 | W | Parotitis | Bilateral chronic anterior uveitis | KP Vitritis Iris nodules | Mantoux (−) QTF (−) Biopsy (−) ACE (+) AST and ALT (−) Lysozyme (−) X-ray−no alterations | Probable |
| 4 | 70 | W | Parotitis | Bilateral chronic anterior uveitis | KP Vitritis Iris nodules | Mantoux (-) QTF (−) Biopsy (−) ACE (−) AST and ALT (−) Lysozyme (−) X-ray with BHL | Presumed |
| 5 | 49 | M | Respiratory | Unilateral chronic anterior uveitis | KP Vitritis Iris nodules | Mantoux (−) QTF (−) Biopsy (−) ACE (−) AST and ALT (−) Lysozyme (−) X-ray with BHL | Presumed |
| 6 | 48 | M | None | Chronic bilateral panuveitis | Vitritis Chorioretinitis | Mantoux (−) QTF (−) Biopsy (+) ACE (+) AST and ALT (−) Lysozyme (−) X-ray with BHL | Definite |
| 7 | 69 | W | None | Unilateral chronic anterior uveitis | Vitritis Iris nodules | Mantoux (−) QTF (−) Biopsy (+) ACE (+) AST and ALT (−) Lysozyme (−) X-ray with BHL | Definite |
| Inittial signs of systemic sarcoidosis | |||||||
| 8 | 76 | W | Respiratory | Chronic bilateral panuveitis | Vitritis Chorioretinitis | Mantoux (−) QTF (−) Biopsy (−) ACE (−) AST and ALT (−) Lysozyme (−) X-ray with BHL | Presumed |
| 9 | 74 | W | Respiratory Peripheral lymphadenopathy | Chronic bilateral panuveitis | Vitritis Chorioretinitis Periphlebitis | Mantoux (−) QTF (−) Biopsy (−) ACE (−) AST and ALT (−) Lysozyme (−) X-ray with BHL | Presumed |
| 10 | 57 | W | Erythema nodosum | Unilateral chronic anterior uveitis | KP Chorioretinitis | Mantoux (−) QTF (−) Biopsy (−) ACE (−) AST and ALT (−) Lysozyme (−) X-ray with BHL | Presumed |
| 11 | 58 | W | Peripheral lymphadenopathy | Chronic bilateral panuveitis | KP Vitritis Iris nodules Chorioretinitis synechiae | Mantoux (−) QTF (−) Biopsy (−) ACE (+) AST and ALT (−) Lysozyme (−) X-ray – no alterations | Possible |
ACE, angiotensin-converting enzymes; ALT, alanine aminotransferase; AST, aspartate aminotransferase; BHL, bilateral hilar lymphadenopathy; BRV, bilateral retinal vasculitis; ID, identification; KP, mutton fat keratic precipitates; M, man; QTF, Quantiferon®; X-ray, radiography; W, woman.
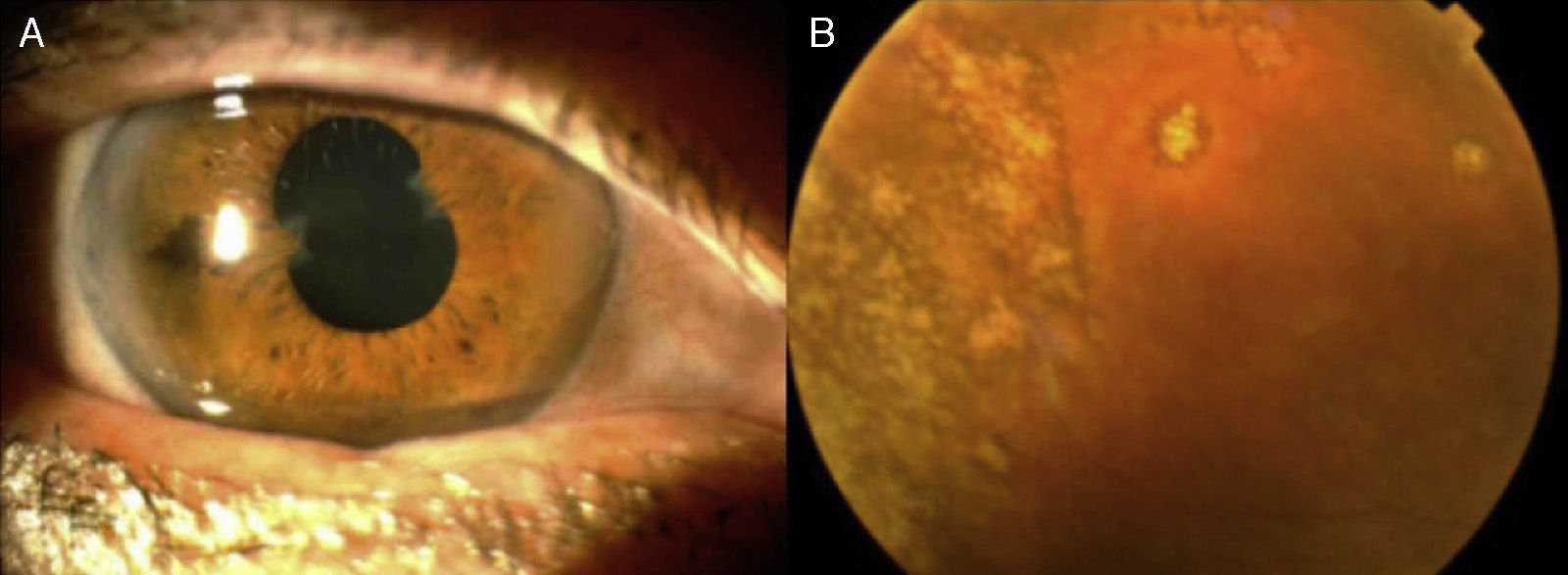
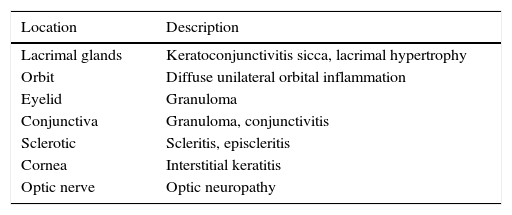
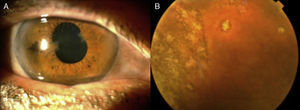
The diagnosis of systemic sarcoidosis is presently based on a combination of clinical and radiographic findings, together with the histological confirmation and the exclusion of other granulomatous diseases, such as tuberculosis.8 In clinical practice, the determination of the angiotensin-converting enzyme level, serum calcium, plain chest X-ray, scintigraphy and screening tests, like Mantoux or Quantiferon®, initially indicate involvement of systemic sarcoid. Ocular involvement in sarcoidosis is presented by up to half of the patients and may even be the initial manifestation of the disease. Sarcoidosis can affect the lacrimal glands and cause keratoconjunctivitis sicca, involving the iris, as well, causing different forms of uveitis and even the development of optic neuritis when it affects the posterior pole. The anatomical location of inflammation in sarcoid uveitis mainly, and chronically, involves the posterior segment. It frequently consists of recurrent bilateral uveitis, and can even cause generalized involvement in the form of bilateral panuveitis associated with retinal vasculitis.9,10 The findings most frequently observed in uveitis associated with sarcoidosis include mutton fat keratic precipitates, iris nodules, tent-shaped peripheral anterior synechiae, vitreous opacities like “snowballs”, multiple peripheral chorioretinal lesions and nodular periphlebitis (Fig. 1). Moreover, there were other ocular signs that could indicate sarcoid involvement, especially if evaluated in the presence of ancillary tests that are positive for sarcoidosis11–14 (Table 3). The diagnostic criteria proposed by the FIWOS were validated in 2010. They include several ophthalmological signs indicative of sarcoidosis and comprise ancillary tests5 (Table 4). These criteria do not include invasive procedures and are useful, in clinical practice, when there is no confirmatory biopsy or when the biopsy is negative.
Involvement of the Eye and Its Neighboring Structures, Except for the Iris.
| Location | Description |
|---|---|
| Lacrimal glands | Keratoconjunctivitis sicca, lacrimal hypertrophy |
| Orbit | Diffuse unilateral orbital inflammation |
| Eyelid | Granuloma |
| Conjunctiva | Granuloma, conjunctivitis |
| Sclerotic | Scleritis, episcleritis |
| Cornea | Interstitial keratitis |
| Optic nerve | Optic neuropathy |
Diagnostic Criteria of the First International Workshop on Ocular Sarcoidosis (FIWOS).
| Intraocular signs indicative of ocular sarcoidosis |
| 1. Mutton fat keratic precipitates and/or iris nodules (Koeppe/Bussaca) |
| 2. Trabecular meshwork nodules and/or tent-shaped peripheral anterior synechiae |
| 3. Vitreous opacities with “snowballs” or a string of pearls |
| 4. Multiple peripheral chorioretinal lesions (active and/or atrophic) |
| 5. Segmental and/or nodular periphlebitis and/or macroaneurysms in an inflamed eye |
| 6. Nodules or granulomas in the optic disc and/or solitary choroidal nodule |
| 7. Bilateral inflammation |
| Ancillary tests suggestive of ocular sarcoidosis |
| 1. Negative tuberculin test in a BCG-vaccinated patient or in one who had a positive result on a previous Mantoux test |
| 2. Elevated angiotensin-converting enzyme and/or elevated lysozyme level |
| 3. Chest X-ray showing bilateral hilar lymphadenopathy |
| 4. Unexpected findings in liver enzyme tests |
| 5. Chest tomography in patients with a negative X-ray |
BCG, Bacillus Calmette-Guérin.
Ocular and systemic manifestations of sarcoidosis, as well as the ancillary tests, show a great variability, a fact that complicates the diagnosis. With our work, we have put into practice the FIWOS criteria, which enabled us to categorize the patients with systemic clinical signs indicative of sarcoidosis together with other ocular manifestations and positive ancillary tests. Because of the heterogeneity of this disease, not all the patients fulfilled the diagnostic criteria for sarcoidosis; for this reason, after the diagnostic categorization, we see that, after satisfying the clinical and ophthalmological criteria and that of the ancillary tests, the patients’ disorder was classified as sarcoidosis. Most of our patients, coinciding with the literature, were women (63.6%). Ocular problems were the initial symptom in 7 of the overall group and most of them had ocular manifestations indicative of sarcoid disease. Tuberculin tests were negative in all of the patients and only 3 patients had a compatible lymph node biopsy. Those who had not undergone a biopsy for the classification criteria, after categorization, had a “presumed” diagnosis of sarcoidosis. The ophthalmological data showed that the most common anatomical location was chronic bilateral panuveitis, affecting 54.5% of the patients. In second place, unilateral chronic anterior uveitis, with 27.2%, was the most frequent form. Most of the patients began with clinical manifestations of uveitis, developing the systemic clinical disease later on. After the categorization of the patients, the diagnosis of sarcoidosis was definite in 4 patients, presumed in 5, probable in 1 and possible in 1 other patient.
The present study is especially interesting for rheumatologists who work in collaboration with ophthalmologists in uveitis clinics, as sarcoidosis is an uncommon disease, it is best to standardize criteria for the correct diagnosis of this disorder. We should also point out that the use of these criteria enables the diagnosis without the need for a biopsy, which could be iatrogenic or difficult in certain patients.
These criteria categorize patients with data indicative of sarcoidosis and who, because of the variability in the clinical course and organic involvement, have not been categorized as patients with sarcoid disease. The sarcoid ocular involvement plays a very significant role for categorization and, for this reason, it is important to stress a detailed ophthalmological examination in search of ocular signs indicative of a granulomatous inflammatory disease.
Ethical DisclosuresProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of dataThe authors declare that they have followed the protocols of their work center on the publication of patient data.
Right to privacy and informed consentThe authors declare that no patient data appear in this article.
FundingNone.
Conflicts of InterestThe authors declare they have no conflicts of interest.
Please cite this article as: Meneses CF, Egües CA, Uriarte M, Errazquin N, Valero Jaimes A, Maíz O, et al. Categorización diagnóstica según los criterios del First International Workshop on Ocular Sarcoidosis (FIWOS) en una serie de 11 pacientes. Reumatol Clin. 2017;13:25–29.