Diffuse idiopathic skeletal hyperostosis is a bone disease characterised by ossification of spinal ligaments and peripheral entheses. Currently, we still use the classic classification criteria that do not include extraspinal manifestations. A number of authors agree on the need to revise them. We present 3 patients in which a diagnosis of diffuse idiopathic skeletal hyperostosis could not be established if we apply those criteria, but they have fully compatible clinical and radiological manifestations of hyperostotic disease.
La hiperostosis esquelética difusa idiopática es una enfermedad caracterizada por la osificación de ligamentos vertebrales y de entesis periféricas. Actualmente, siguen utilizándose los criterios clasificatorios clásicos que se basan en hallazgos radiológicos vertebrales, pero que no incluyen otras manifestaciones clinicopatológicas que conforman el espectro de la enfermedad. Diversos autores abogan por la revisión y actualización de dichos criterios. A continuación describimos 3 casos clínicos en los que no se podría establecer un diagnóstico de hiperostosis esquelética difusa idiopática pero que presentan unas manifestaciones clínico-radiológicas totalmente compatibles con la enfermedad hiperostosante.
Diffuse idiopathic skeletal hyperostosis (DISH) was defined more than 60 years ago by Forrestier and Rotés.1 This disease is characterised by ossification of the anterior longitudinal ligament of the spine, and multiple areas of the entheses of the ligament, tendon, joint capsule or annulus fibrosus. The classification criteria of Resnick-Niwayama (1976) are still used to diagnose the condition, and are solely based on characteristic vertebral radiographic signs.2 This classification has been questioned by various authors, such as Utsinger (1985) who presented other criteria that included extraspinal involvement of the disease, and even enabled diagnosis of DISH without spinal involvement.3 This author already noted that the patients who did not meet the classical criteria of the disease could have early stages of it. For years other diagnostic proposals have been published that differ essentially in the number of bony bridges between affected vertebrae, with or without a description of preserved disc or sacroiliac space, and/or the presence of enthesis ossification.4–6 Given the need to standardise and update diagnosis of DISH, Mader et al. sought to revise the definition of the disease and design new criteria to include specific clinical manifestations, such as extraspinal involvement or the association with certain metabolic disorders, but reached no final consensus.7
We present 3 patients who could not be classified as having DISH using Resnick's criteria, but who without doubt had a clinical form with peripheral predominance that is widely described in hyperostotic disease.
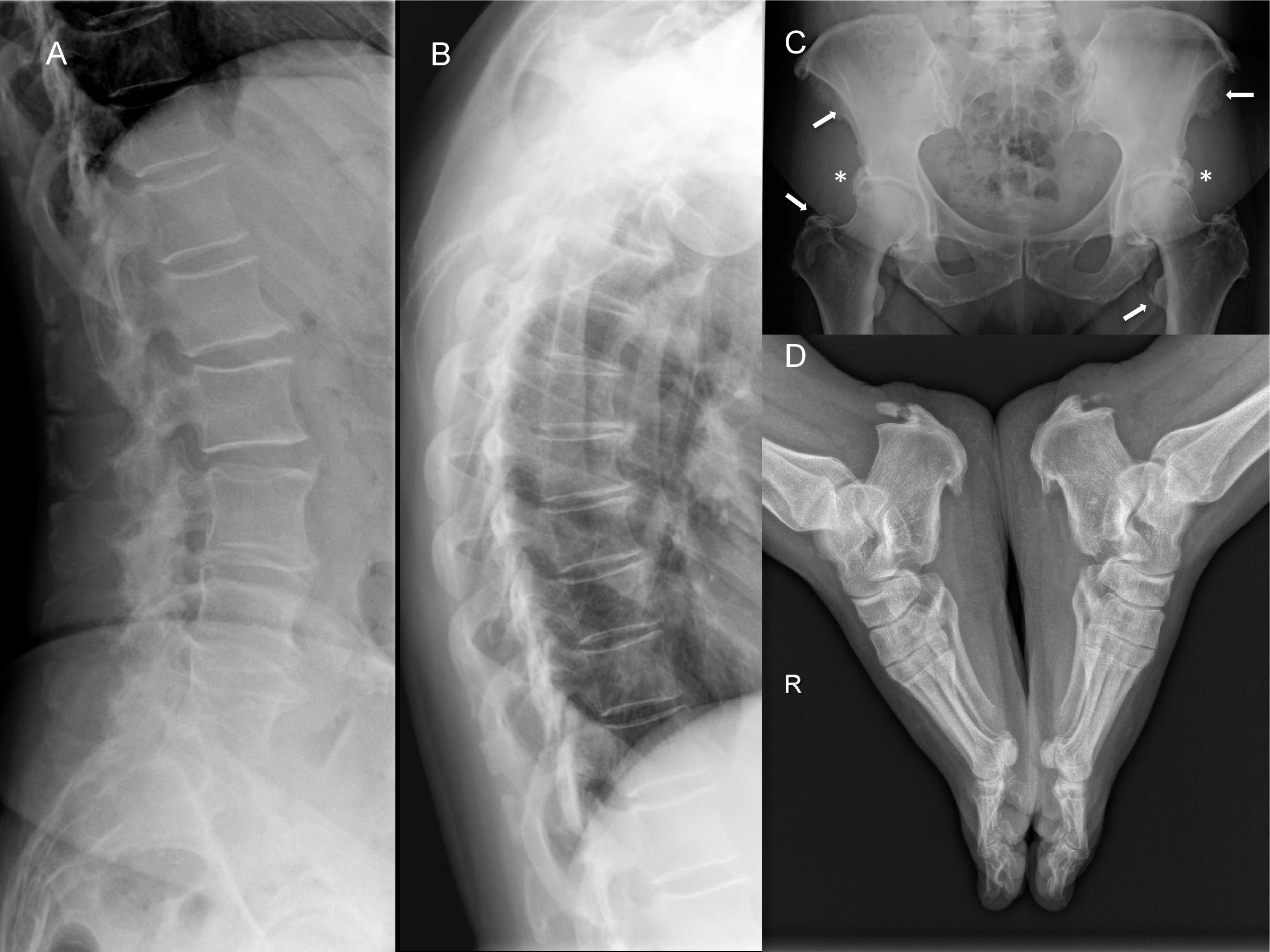
Case 1A 63-year-old woman, monitored by the rheumatology clinic over 47 years. The initial reason for consultation was pain and progressive restriction of bilateral coxofemoral mobility. She had no personal or family history of psoriasis, no other diseases related to spondyloarthritis, and no intake of retinoids or other vitamin A derivatives. Her blood tests showed no elevation of acute phase reactants or phosphocalcium metabolism disorders, and HLAB27 was negative. Of interest in her medical history were glucose intolerance and high blood pressure. She showed no sign of vertebral involvement in the initial study, but there was already exuberant bony proliferation on her iliac crests, ischial and trochanteric tuberosities, and lateral acetabular prominences with preserved joint space. Subsequently, there was the addition of other sites, such as insertions in the calcaneus, Achilles tendon, triceps, olecranons and patellae (Fig. 1). Various radiological studies of the spine were performed as the condition progressed that found no alterations suggestive of calcification of the anterior common vertebral ligament (ACVL) until the last radiographic check, when an incipient bony bridge was revealed in the cervical spine. The patient underwent various operations, such as resection of the ossification in the bilateral Achilles insertion, because it was impossible for her to put her shoes on, and hip arthroscopy to resect the acetabular ossification in order to improve her joint balance.
Radiological study of case 1. (A and B) Lateral projections of the dorsal and lumbar spine with signs of spondyloarthrosis of lumbar predominance with no ossification of the ACVL. (C) Prominent acetabular bony excrescences with preserved joint space (*), and multiple enthesis ossifications on the iliac spines and the trochanters (arrows). (D) Prominent bony excrescences on the plantar and Achilles tendon entheses.
A 47-year-old woman, with a four-year history of bilateral Achilles tendon pain and swelling. The patient was obese, but with no associated metabolic or cardiovascular disease. She had no family or personal history of psoriasis, spondyloarthritis or retinoid intake. Her blood tests were normal, but vertebral radiology revealed incipient radiographic signs of hyperostosis in the dorsal and lumbar spine that did not meet Resnick's criteria. A more extensive radiological study was requested that showed ossifications in the entheses of the pelvis, knees, feet and shoulders.
Case 3A 50-year-old woman, with a history of bilateral epicondylitis, who initially consulted with bilateral plantar fasciitis resistant to local corticosteroid-anaesthetic injections, orthesis and physiotherapy. The patient had no personal, family or drug history of interest, and blood tests were not significant. No vertebral radiological changes were detected, but prominent coxofemoral ossifications were found, with no loss of joint space, and extraspinal involvement in the Achilles tendon, plantar, patellar and olecranon entheses.
DiscussionWe consider that the 3 cases presented had a DISH (Utsinger's criteria), although they did not meet Resnick's classical criteria due to incipient or no vertebral involvement. We were struck by a series of particularities that differ from those traditionally described in the disease, such as the patients’ age and sex, the “non benign” nature of the disease course, and minimal or no spinal manifestations, even after a course of years.
DISH has been traditionally considered a disease that predominates in males, and whose prevalence increases with age. The most significant epidemiological studies achieve a diagnosis of the disease based exclusively on the findings of conventional radiology or computed tomography of the spine. The prevalence of DISH is estimated at between 3.6% and 28% in males and from 0.8% to 13.9% in women.8–11 In a recent study in an Asian population the prevalence was 10.8% (ratio 5:1), and although it has traditionally been described in people of advanced age, these authors already observed 1.8% males and .7% in women aged under 50 years of age. Given the diversity of classification criteria, the epidemiological data published are very variable, and do not include the forms where peripheral ossification predominates over vertebral ossification.
Resnick and Niwayama pointed out that DISH might not be a disease per se, but rather a state of extensive ossification. It is described in the literature that levels of vertebral pain are lower in hyperostotic disease than in spondyloarthrosis.12 However, Mata et al., although they corroborate the above in terms of pain and rigidity in the lumbar segment, they did not observe this in other sites studied such as the cervical or dorsal spine or the extremities.13 In reality, functional capacity evaluation has only been undertaken in one single study where the authors detected poor functional status, regardless of body mass index, measured through the abbreviated HAQ questionnaire compared to a healthy population.14 in our first case, the exuberant bony excrescences resulted in several operations due to their impact on the person's physical function and quality of life. In the other cases, the involvement of the Achilles tendon and calcaneus enthuses required various treatments, and resulted in long periods of functional incapacity and sick leave.
Since Forestier's definition, certain metabolic or constitutional factors are considered to be linked to the disease. Our 3 patients were overweight, and the first case also had hypertension and oral glucose intolerance that developed into type 2 diabetes mellitus. In recent years the physiopathogenic role of metabolic dysfunction in the ossification of ligaments and entheses has been researched. In this regard, Mader et al. performed a study where they found that the likelihood of developing a DISH in the fifth decade of life was 5 times greater in a patient of the same age and sex if they had 3 clinical parameters such as obesity, a first-degree relative with a history of hypertension or diabetes, and back or chest pain or enthesitis or tendinitis.15
Finally, in the cases we present we wanted to highlight the predominance of extraspinal manifestations over little or no axial involvement. Although according to Utsinger these would be early stages, our first patient was followed up over 15 years without presenting a single radiological sign in the vertebrae. Based on these observations it may well be that these were not different stages of the disease, but different phenotypes of it. We describe a pattern of peripheral predominance that would not meet the classical classification criteria of Resnick, that would be more prevalent in females, and which would start at younger ages. However, studies are required with larger numbers of patients, but that include forms with predominant extraspinal involvement in particular. We agree with the authors that uphold the need to create new more complete classification criteria that take into account all the manifestations of the disease, such as peripheral involvement in the form of enthesis ossification or the presence of comorbidities. These would provide us greater knowledge of the entire clinical spectrum of the disease, access to epidemiological data, to real data on disability and quality of life, as has been researched in other rheumatic diseases. In short, we would be able to identify patients in earlier stages in order to apply therapies that might change the course of the DISH.
ConclusionDISH is a relatively common rheumatic disease, with a broad spectrum of manifestations, which is currently diagnosed in advanced stages or with major complications of spinal involvement. Extraspinal manifestations often go unnoticed, but can be a sign of early disease. Finally, we stress the need to consider a diagnosis of DISH in a patient presenting with one or various enthesopathies in order to make an early diagnosis, and consider therapeutic measures in less advanced stages of the disease.
Ethical ResponsibilitiesProtection of people and animalsThe authors declare that neither human nor animal testing has been carried out under this research.
Data confidentialityThe authors declare that they have complied with their work centre protocols for the publication of patient data.
Privacy rights and informed consentThe authors declare that no patients’ data appear in this article.
Conflict of InterestsThe authors have no conflict of interests to declare.
Please cite this article as: Clavaguera T, Reyner P, Valls R, de Cendra E, Rodríguez-Jimeno MC. Hiperostosis esquelética difusa idiopática: ¿existe un patrón de predominio periférico? Reumatol Clin. 2019;15:301–304.