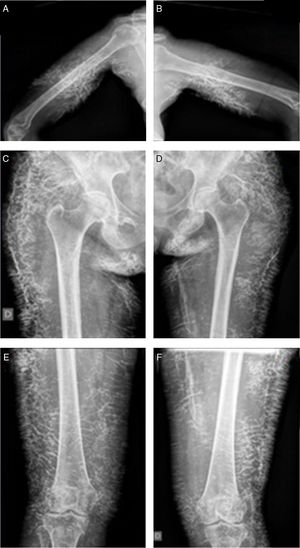
A female aged 48 who presented at the surgery with photosensitivity, heliotrope erythema and cervical and upper trunk level erythematous injuries, in addition to myalgias and proximal muscle weakness, 3/5 in upper and lower limbs, and weakness of the flexor tendons of the neck. Laboratory tests revealed erythrocyte sedimentation of 54mm/h, CPK 9.870U/l, significant elevation of transaminase levels and lactate deshydrogenase levels, and ANA 1:1.280 mottled pattern. Magnetic resonance of the thighs showed exaggerated inflammatory changes. Electromyography had potentials of polyphasic motor units of short duration and low amplitude, mainly at gluteus level. Muscular biopsy was compatible with dermatomyositis. Treatment was initiated with 40mg/day prednisone, 20mg/week methotrexate, 5mg/week folic acid, 200mg/12h hydroxychloroquine and muscular physiotherapy. Twenty days later, the patient presented with progression of weakness of 2/5 in lower limbs and 1/5 in upper limbs and was incapacitated and prostrate. Three pulsatile administrations of methylprednisone, cyclophosphamide and gammaglobulins were given. Treatment continued with pulsatile administrations of cyclophosphamide and she received infusions of 1g/kg/2 days in three consecutive stays every 30 days. Improvement occurred with intensive treatment and rehabilitation, with the patient being able to stand up and to walk after 3 months of treatment. There was an improvement in her extensively compromised cutaneous barrier after initiating treatment with 1g rituximab. Cutaneous calcifications progressed in triceps, gluteus, thighs and legs despite treatment with gammaglobulins, rituximab, pamidronate and colchincine (Fig. 1).
Calcinosis is a common finding in inflammatory myopathies, especially in juvenile dermatomyositis (20%–70%), but it is infrequent when the disease presents in the adult (20%).1 It is associated with the disease activity and progression, a highly compromised cutaneous barrier and a delay or lack of response to treatment.2 It is more common in regions of persistent stress and trauma. Its pathogenesis is unclear.2 Several recent reports associate this complication with the presence of anti-NXP2 antibodies in disseminated form and with anti-PM/Scl1,3,4 forms.
This complication is difficult to treat. Several strategies which have demonstrated improvement in case reports are: warfarin (not currently recommended due to risk of bleeding), thalidomide, diltiazem or colchincine (with tolerance-dependence dose adjustment), biphosphonates (cyclical infusions of amidronate or alendronate with oral administration of maintenance treatment), inmunoglobulins, and biologic agents, including infliximab and abatacept.5–10 Some recent case reports suggest that rituximab could be a favourable therapeutic option in severe and refractory cases.5,6 Surgery is reserved for discrete lesions due to the risk of infection.6–10
Ethical LiabilitiesProtection of people and animalsThe authors declare that no experiments using human beings or animals have been carried out for this research study.
Data confidentialityThe authors declare they have followed the protocols of their centre of work on patient data publication.
Right to privacy and informed consentThe authors declare that no patient data appear in this article.
Conflicts of InterestThe authors have no conflicts of interest to declare.
Please cite this article as: Baenas DF, Pirola JP, Benzaquén NR, Caeiro F, Álvarez AC, Saurit V, et al. Calcinosis extensa en dermatomiositis del adulto. Reumatol Clin. 2019;15:121–123.