Minimizing disability and enhancing physical function to its optimal levels is still a challenge in management of rheumatoid arthritis (RA). The aim is to identify factors leading to disability in RA.
MethodsThis is a cross-sectional Egyptian multicenter study carried out on 215 RA patients attending to our inpatient and outpatient rheumatology clinics during 4 months starting from April to July 2017 who agreed to participate in the study; 170 patients were from Cairo University hospitals and 45 from Zagazig University hospitals. We recorded a number of possible risk factors including demographic, clinical, serological and therapeutic factors. The assessment of patients’ disability was done using Modified HAQ (MHAQ).
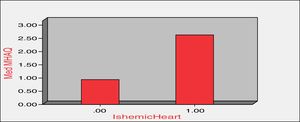
ResultsA significant positive correlation was found between MHAQ and different markers of activity in addition to age and depression score (P<0.001). Illiteracy accounted for higher MHAQ scores (P=0.001). A higher MHAQ was found in patients with ischemic heart disease (P<0.05). Patients with erosions on X-rays had significantly higher MHAQ scores. Subluxations also accounted for higher MHAQ scores (P=0.000).
ConclusionAging, illiteracy, disease activity, erosions, subluxations, depression and ischemic heart disease were all related to higher disability. Good control of disease activity which in turn reduces erosions and subluxations is mandatory. Screening for depression and proper use of anti-depressants is of great value. Proper screening and prophylaxis is recommended against ischemic heart disease by controlling modifiable risk factors like obesity, dyslipidaemia, hypertension, smoking and sedentary lifestyle.
Minimizar la discapacidad y mejorar la función física hasta sus niveles óptimos sigue siendo un desafío en el tratamiento de la artritis reumatoide (AR). El objetivo es identificar los factores que conducen a la discapacidad en la AR.
MétodosSe trata de un estudio multicéntrico egipcio de corte transversal llevado a cabo en 215 pacientes con AR que asisten a nuestras clínicas de reumatología para pacientes internados y ambulatorios durante 4 meses, desde abril a julio de 2017, que aceptaron participar en el estudio; 170 pacientes eran de hospitales de la Universidad de El Cairo y 45 de hospitales de la Universidad de Zagazig. Registramos una serie de posibles factores de riesgo que incluyen factores demográficos, clínicos, serológicos y terapéuticos. La evaluación de la discapacidad de los pacientes se realizó utilizando HAQ modificado (MHAQ).
ResultadosSe encontró una correlación positiva significativa entre MHAQ y diferentes marcadores de actividad además de la puntuación de edad y depresión (p<0,001). El analfabetismo representó un puntaje MHAQ más alto (p=0,001). Se encontró un MHAQ más alto en pacientes con cardiopatía isquémica (p<0,05). Los pacientes con erosiones en los rayos X tuvieron puntajes de MHAQ significativamente más altos. Las subluxaciones también representaron puntuaciones más altas de MHAQ (p=0,000).
ConclusiónEl envejecimiento, el analfabetismo, la actividad de la enfermedad, las erosiones, las subluxaciones, la depresión y la cardiopatía isquémica se relacionaron con una mayor discapacidad. El buen control de la actividad de la enfermedad que a su vez reduce las erosiones y las subluxaciones es obligatorio. La detección de la depresión y el uso adecuado de antidepresivos es de gran valor. Se recomienda la detección y profilaxis adecuada de la cardiopatía isquémica controlando los factores de riesgo modificables como la obesidad, la dislipidemia, la hipertensión, el tabaquismo y el estilo de vida sedentario.
Rheumatoid arthritis is an autoimmune disorder characterized mainly by targeting the joints leading to arthritis, limitation, deformities and even joint destruction. Joint affection may interfere with patients’ occupational, vocational and recreational activities leading to a very miserable life in some cases.
Early diagnosis and treatment of rheumatoid arthritis aimed mainly to limit attacks of arthritis to protect the joint from losing its function and integrity. Various medications have been and still are being introduced to the market aiming to prevent the burden of disability on patients, caregivers and communities.
Disease-modifying anti-rheumatic drugs have been found to reduce functional disability for at least 1 or 2 years1–6 while delay in the use of these drugs proved to result in worse outcomes.7–10 Moreover, many reports suggested that there have been major modifications in DMARDS’ treatment strategies throughout many years that were found to improve long-term outcomes.11–13 A recent article by Gwinnutt et al. published in 2017 stated that according to a 20-year follow-up of patients included in the Norfolk Arthritis Register, early treatment of RA leads to improved long-term functional outcomes compared with later treatment (>6 months after symptom onset).14
In 2008, Oken et al. studied factors associated with functional disability and found that between all studied factors only disease activity had an impact on physical function as every small improvement in disease activity scores resulted in a large gain in activities of daily living and that treatment should mainly target disease activity.15
In 2015, the concept of disability determinants began to change again. Even in the era of biologic therapy, the effect of other possible factors not related to therapeutic strategies was studied. Female sex, corticosteroids, and antidepressants were described as profound determinants of disability.16
Later in June 2016, a group of researchers developed a clinical prediction tool for estimation of disability at 1 year with scores ranging from 0 to 26. Higher scores corresponded with higher probabilities of reporting higher HAQ scores at 1 year. The tool contained anxiety and depression scores, employment, absenteeism and BMI.17 In 2017, Ji et al. studied disability and quality of life in 101 Chinese RA patients, they found that long disease duration, high disease activity, a larger number of tender and swollen joints, and high C-reactive protein (CRP) level were all associated with functional disability and added that participants with functional disability tended to have more severe depressive symptoms and a lower quality of life.18
Despite the introduction of more advanced technologies in drug manufacturing and the great improvement in disease outcome; minimizing disability and enhancing physical function to its optimal levels is still a challenge. The control of inflammation does not seem to be the only approach anymore; a more comprehensive approach may be needed to optimize physical function based on understanding the role of all underlying mechanisms and factors.
As is the case for any disease, factors influencing its outcome differ from one population to the other. Researchers in different parts of the world work hard to study different populations to determine the determinants of disease outcome in each. From this point of view our aim was to study an Egyptian population with RA detecting different determinants and contributing factors of functional disability and higher MHAQ scores seeking to target these factors in the future to improve patients overall physical activity and functional outcomes.
Patients and methodsAll procedures performed in this study were in accordance with the ethical standards of the institutional and national research committee and with the 1964 Helsinki declaration and its later amendments. Informed consent was obtained from all individual participants included in the study.
Study designThis is an observational cross-sectional Egyptian multicenter study. Two hundred and fifteen RA patients attending to our inpatient and outpatient rheumatology clinics who agreed to participate in the study were recruited during 4 months starting from April to July 2017; 170 patients were from Cairo University hospitals and 45 patients from Zagazig University hospitals. Inclusion criteria included patients’ who fulfilled the 2010 American College of Rheumatology (ACR)/European League Against Rheumatism Classification (EULAR) criteria for rheumatoid arthritis19 who accepted to join the study (a consent was taken from all participants for ethical considerations) and were above 16 years. Exclusion criteria included other causes of disability such as previous traumatic conditions like fractures, cut tendons, burn contractures, and previous neurologic deficits not related to the disease like hemiplegia, nerve injuries, etc. Also other autoimmune conditions other than RA were excluded like overlapping autoimmune syndromes, scleroderma, dermatomyositis and others were excluded, etc.
The information about risk factors was based on history taking and clinical assessment at time of examination in addition to clinical, laboratory and imaging data that were previously recorded in the patients’ files. We recorded a number of possible risk factors including demographic, clinical, serological and therapeutic factors. The assessment of patients’ disability was done by Modified HAQ20 at the time of examination.
Demographic factorsThe demographic factors included age, gender, weight, height, BMI, education and employment. The patients’ educational level was classified as illiterate or educated. Regarding occupation patients were classified as being unemployed, or having a blue collar (workers who perform manual labor) or white collar (workers who perform professional jobs) employment.
Clinical factorsWe recorded disease duration, morning stiffness, general health, physician's global visual analogue scale VAS (1–10), current disease activity using Disease Activity Score 28-ESR (DAS 28-ESR) was also calculated.21 Presence of fibromyalgia was assessed according to the American College of Rheumatology's (ACR's) 1990 criteria for classifying fibromyalgia.22 Anxiety and depression were assessed according to Hospital Anxiety and Depression scale HADS23 were also recorded in some patients.
Laboratory factorsMost recent laboratory investigations were recorded including erythrocyte sedimentation rate (ESR), high sensitivity C-reactive protein (hs-CRP), serum albumin, hemoglobin, rheumatoid factor and antibodies to cyclic citrullinated peptide (anti-CCP).
Imaging factorsMost recent X-ray findings were recorded regarding erosions, subluxations and deformities. Also history of previous arthrodesis or arthroplasty was also recorded.
Therapeutic factorsWe recorded the drugs used by each patient, including corticosteroids and disease modifying anti-rheumatic drugs (DMARDS) like anti-malarials, methotrexate, sulfasalazine, leflunomide, and biological therapy.
ComorbiditiesPresence of comorbidities like hypertension, diabetes, ischemic heart disease, dyslipidemia, bronchial asthma, chronic kidney disease, hypo/hyperthyroidism, HCV and osteoporosis was also recorded regardless patient developed them on top of RA or as a complication of the disease or its treatment.
Disability assessmentThe Modified Health Assessment Questionnaire (MHAQ) is a questionnaire for the assessment of rheumatoid arthritis. The questionnaire is a patient reported outcome (PRO) which is usually self-administered by the patient. The MHAQ is a modification of the HAQ. It was developed to include questions concerning perceived patient satisfaction regarding the same activities of daily living, along with perceived change in degree of difficulty. The number of activities of daily living was reduced from 20 (HAQ) to 8 (MHAQ). The eight activities measured by the MHAQ are: dressing and grooming, arising, eating, walking, hygiene, reach, grip and common daily activities. Patients are asked to rate these daily activities on a scale ranging from 1 to 4 with: without difficulty, with some difficulty, with much difficulty and unable to do.20
Statistical analysisThe data were analyzed using the SPSS software package version 18.0 (SPSS, Chicago, IL, USA). The quantitative data were expressed using the mean and standard deviation, while the qualitative data were expressed as median, range, frequency and percent. Most of our data were non-parametric and so were analyzed mainly using the Mann–Whitney test, Kruskal–Wallis test and the Spearman correlation. Multiple linear regression analysis was also performed. We assumed that the P value was significant at 0.05 and highly significant at 0.001.
ResultsDemographics and patient characteristicsThere were 215 RA patients in this multicenter study. Demographic data and patient characteristics are represented in Table 1.
Characteristics of RA patients.
| RA patients’ characteristics (n=215) | |
|---|---|
| Demographic Data | |
| Age in years (mean +SD) | 47.3 + 12.66 |
| Height(mean +SD) | 161.2 + 6.96 |
| Weight(mean +SD) | 81.67 + 15.25 |
| BMI (mean +SD) | 31.56 + 6.32 |
| Gender(no & %) | |
| Males | 21(9.8) |
| Females | 194 (90.2) |
| Race (Caucasians) (no & %) | 215(100) |
| Disease duration in months(median & range) | 48 (0.5- 408) |
| Clinical features | |
| Morning stiffness with treatment(median & range) | 30 (0-360) |
| Physician Global(median & range) | 6 (0-10) |
| Patient Global (General Health)(median & range) | 6 (0-10) |
| TJC(median & range) | 10 (0-28) |
| SJC(median & range) | 5 (0-24) |
| MHAQ(median & range) | 1 (0-20) |
| DAS 28(mean +SD) | 5.1 (+1.6) |
| Laboratory investigations | |
| ESR (mm/hr)(median & range) | 39 (5-144) |
| CRP (mg/L)(median & range) | 9.1 (0.7-124.5) |
| Hemoglobin (g/dl)(median & range) | 12 (3.2-113) |
| Serum Albumin (mg/dl)(mean +SD) | 4.03 (+ 0.46) |
| Positive RF (no & %) | 153 (71.2) |
| Positive Anti-CCP (n=161)(no & %) | 105 (48.8) |
| RF titre(median & range) | 58.8 (1.6- 1280) |
| Anti-CCP titre(median & range) | 161 (0.7- 1620) |
| Radiography | |
| Erosions in plain X-ray (no & %) | 175 (73) |
| Medications | |
| NSAIDS(no & %) | 108 (50.2) |
| Corticosteroids(no & %) | 124 (57.7) |
| Antimalarial(no & %) | 166 (77.2) |
| Methotrexate(no & %) | 151 (70.2) |
| Leflunamide(no & %) | 67 (31.2) |
| Sulfasalazine(no & %) | 26 (12.1) |
| Azathioprine(no & %) | 1 (0.5) |
| Cyclophosphamidea(no & %) | 1 (0.5) |
| Biologicalb(no & %) | 2 (0.9) |
No (%): number and percentage of cases. TJC: tender joint count, SJC: swollen joint count, DAS 28: 28 joint count Disease Activity Score by Prevooet al.1995, ESR: erythrocyte sedimentation rate, CRP: C-reactive protein, RF: Rheumatoid Factor, Anti-CCP: Anti-cyclic citrullinated peptide. MHAQ: Modified Stanford Health Assessment Questionnaire Pincus et al., 1983. NSAIDS: Non-steroidal anti-inflammatory drugs.
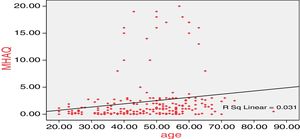
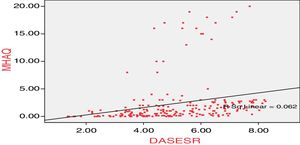
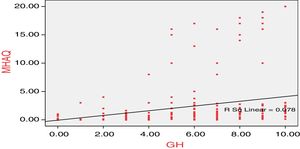
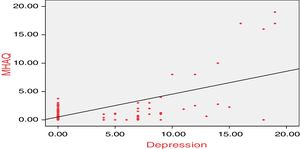
A significant positive correlation was found between MHAQ and many different markers of activity as shown in Table 2 in addition to age and depression score (P≤0.001). Other correlations with the MHAQ were not significant (P>0.05). Figs. 1–4 show correlations between MHAQ and age, General Health (GH), DAS-ESR, and Depression Score. Table 3 shows multiple linear regression analysis between different parameters that were correlated with MHAQ, the regression model was statistically significant (P=0.000), TJC was the most significant parameter in this model (P=0.000).
Correlations between different patient characteristics and MHAQ.
| Patient characteristics | R | P |
|---|---|---|
| Age | 0.276 | 0.000** |
| Bodyweight | −0.036 | 0.637 |
| Height | −0.036 | 0.642 |
| BMI | −0.017 | 0.824 |
| Disease duration | −0.094 | 0.180 |
| Morning stiffness | 0.303 | 0.000** |
| Physician's global | 0.409 | 0.000** |
| General health | 0.497 | 0.000** |
| TJC | 0.579 | 0.000** |
| SJC | 0.345 | 0.000** |
| ESR | 0.204 | 0.003* |
| DAS 28 | 0.504 | 0.000** |
| Hemoglobin | −0.120 | 0.082 |
| CRP | 0.271 | 0.121 |
| Albumin | −0.054 | 0.440 |
| Depression score | 0.763 | 0.001** |
Correlations were performed by Spearman correlation. r: correlation coefficient; DAS 28: 28 joint count Disease Activity Score by Prevoo et al., 1995; TJC: tender joint count; SJC: swollen joint count; ESR: erythrocyte sedimentation rate; CRP: C-reactive protein.
Multiple linear regression analysis: comparing determinants of higher MHAQ.
| Model | Unstandardized coefficients | Standardized coefficients | t | Sig. | Model summary | ||||
|---|---|---|---|---|---|---|---|---|---|
| B | Std. error | Beta | R2 | Adjusted R2 | F | P | |||
| (Constant) | 0.407 | 1.491 | 0.273 | 0.785 | |||||
| Age | 0.020 | 0.023 | 0.060 | 0.879 | 0.380 | ||||
| MS | 0.002 | 0.005 | 0.023 | 0.353 | 0.724 | 0.236 | 0.204 | 7.480 | 0.000** |
| Physician | 0.269 | 0.211 | 0.170 | 1.277 | 0.203 | ||||
| GH | −0.025 | 0.185 | −0.016 | −0.134 | 0.893 | ||||
| TJC | 0.299 | 0.051 | 0.557 | 5.877 | 0.000** | ||||
| SJC | −0.033 | 0.079 | −0.046 | −0.426 | 0.670 | ||||
| ESR | 0.008 | 0.012 | 0.051 | 0.680 | 0.497 | ||||
| DAS 28 | −0.732 | 0.402 | −0.270 | −1.823 | 0.070 | ||||
MS: morning stiffness; GH: general health; TJC: tender joint count; SJC: swollen joint count; ESR: erythrocyte sedimentation rate; DAS 28: 28 joint count disease activity score by Preevo et al., 1995.
Tables 4 and 5 show the comparison between different groups regarding MHAQ. Patients’ age influenced MHAQ greatly; patients between 40 and 60 years had significantly higher MHAQ scores than those between 20 and 40. Moreover, patients with disease duration greater than 10 years showed significantly higher MHAQ (P=0.01). Illiteracy accounted significantly for higher MHAQ scores (P=0.001). Among all co-morbidities, a higher MHAQ was found in patients with ischemic heart disease compared to those without and the difference was statistically significant (P<0.05) (Fig. 5). In addition, patients with erosions on X-rays had statistically significant higher MHAQ scores compared to non-erosive patients. Subluxations also accounted for significantly higher MHAQ scores (P=0.000). Depression also seemed to interfere with activities of daily living and contributed significantly to disability (P<0.05). No specific drug use was found to influence MHAQ.
The relation between MHAQ and different demographic and clinical factors.
| Characteristic | MHAQ | P value |
|---|---|---|
| Median (range) | ||
| Disease durationa | ||
| <10 years (n=140) | 0.75 (0–20) | 0.01* |
| >10 years (n=47) | 1.38 (0–19) | |
| Ageb | ||
| 16–19 (n=0) | 0 (0) | 0.002* |
| 20–29 (n=22) | 0.5 (0–2.75) | |
| 30–39 (n=38) | 0.25 (0–8) | |
| 40–49 (n=50) | 0.875 (0–19)d | |
| 50–59 (n=65) | 1.19 (0–20)c | |
| 60–69 (n=34) | 1.75 (0–17)c | |
| >70 (n=6) | 2.375 (0–3) | |
| Sexa | ||
| Females (n=194) | 1 (0–20) | 0.542 |
| Males (n=21) | 1 (0–10) | |
| Educationa | ||
| Illiterate (n=113) | 1 (0.13–8) | 0.001* |
| Educated (n=102) | 0.5 (0–3) | |
| Employmentb | ||
| Unemployed (n=184) | 1 (0–20) | 0.215 |
| Blue collar (n=14) | 1 (0–3) | |
| White collar (n=17) | 0.5 (0–3) | |
| Smokinga | ||
| Non-smoker (n=192) | 1 (0–20) | 0.521 |
| Smoker (n=23) | 1 (0–15) | |
| Hypertensiona | ||
| Absent (n=178) | 0.94 (0–20) | 0.518 |
| Present (n=37) | 1 (0–17) | |
| Ischemic heart diseasea | ||
| Absent (n=208) | 0.94 (0–20) | 0.003* |
| Present (n=7) | 2.63 (1–17) | |
| Diabetesa | ||
| Absent (n=185) | 1 (0–19) | 0.110 |
| Present (n=30) | 1.125 (0–20) | |
| Thyroid diseasea | ||
| Absent (n=204) | 1 (0–20) | 0.696 |
| Present (n=11) | 1.063 (0–2.5) | |
| Hepatitisa | ||
| Absent (n=158) | 1 (0–20) | 0.195 |
| Present (n=57) | 0.75 (0–2.88) | |
| Chronic kidney diseasea | ||
| Absent (n=214) | 1 (0–20) | 0.229 |
| Present (n=1) | 3 (3–3) | |
| Bronchial asthmaa | ||
| Absent (n=209) | 1 (0–20) | 0.299 |
| Present (n=6) | 2.19 (0.13–3) | |
| Osteoporosisa | ||
| Absent (n=191) | 0.88 (0–19) | 0.247 |
| Present (n=24) | 1063 (0–19) | |
| Fibromyalgia (n=205)a | ||
| Absent (n=184) | 0.88 (0–20) | 0.225 |
| Present (n=21) | 1.13 (0–10) | |
| Depression (n=185)b | ||
| Normal (n=149) | 0.75 (0–3.75) | 0.011* |
| Borderline (n=9) | 1 (0–8) | |
| Depressed (n=27) | 1.5 (0–19)c | |
| RFa | ||
| Negative (n=58) | 1 (0–19) | 0.628 |
| Positive (n=157) | 1 (0–20) | |
| Anti-CCP (n=161)a | ||
| Negative (n=56) | 1 (0–3.75) | 0.204 |
| Positive (n=105) | 0.69 (0–8) | |
| Erosions (n=204)a | ||
| Absent (n=47) | 0.75 (0–4) | 0.018* |
| Present (n=157) | 1 (0–19) | |
| Subluxationsa | ||
| Absent (n=185) | 0.75 (0–13) | 0.000** |
| Present (n=30) | 4 (0–20) | |
| Arthroplastya | ||
| Absent (n=205) | 1 (0–20) | 0.087 |
| Present (n=10) | 1.75 (0–16) | |
| Arthrodesisa | ||
| Absent (n=212) | 1 (0–20) | 0.776 |
| Present (n=3) | 1.75 (0.25–1.88) | |
RF: rheumatoid factor; anti-CCP: anti-cyclic citrullinated peptide; MHAQ: Modified Stanford Health Assessment Questionnaire Pincus et al., 1983.
The relation between MHAQ and the use of different medications.
| Characteristic | MHAQ Median (range) | P value |
|---|---|---|
| NSAIDS | ||
| Non-users (n=107) | 1.125 (0-20) | 0.088 |
| Users (n=108) | 0.875 (0-19) | |
| Corticosteroids | ||
| Non-users (n=91) | 0.75 (0-19) | 0.588 |
| Users (n=124) | 1 (0-20) | |
| Antimalarial | ||
| Non-users (n=49) | 1 (0-19) | 0.990 |
| Users (n=166) | 1 (0-20) | |
| Methotrexate | ||
| Non-users (n= 64) | 1.28 (0-19) | 0.488 |
| Users (n=151) | 0.88 (0-20) | |
| Leflunomide | ||
| Non-users (n=148) | 1 (0-20) | 0.580 |
| Users (n=67) | 0.75 (0-18) | |
| Salazopyrine | ||
| Non-users (n= 189) | 1 (0-19) | 0.510 |
| Users (n=26) | 1.25 (0-20) | |
| Azathioprinea | ||
| Non-users (n=214) | 1 (0-20) | 0.283 |
| Users (n=1) | 3 (3-3) | |
| Cyclophosphamidea | ||
| Non-users (n=214) | 1 (0-20) | 0.283 |
| Users (n=1) | 3 (3-3) | |
| Biologics | ||
| Non-users (n=213) | 1 (0-20) | 0.493 |
| Users (n=2) | 0.565 (0.13-1) | |
| Tramadol | ||
| Non-user (n=201) | 0.75 (0-3.75) | 0.740 |
| User (n=14) | 1 (0-3) | |
| Anxiolytics | ||
| Non-users (n=205) | 0.75 (0-3.75) | 0.268 |
| Users (n=10) | 1 (0-3) | |
| Antidepressant | ||
| Non-users (n=195) | 0.75 (0-3.75) | 0.111 |
| Users (n=20) | 1.065 (0-3) | |
| Hypnoticsa | ||
| Non-users (n=214) | 0.875 (0-3.75) | 0.247 |
| Users (n=1) | 0.125 (0.13-0.13) | |
NSAIDS: Non-steroidal anti-inflammatory drugs. Analysis was done by Mann Whitney U test (MW).
Rheumatoid arthritis outcome differs greatly between populations and individuals. Decreased physical function and disability are most problematic being a disease mainly targeting joints. Disease activity has been thought to be the main contributor to disability, but other factors are still being highlighted in more recent studies and in different populations. In this study we gathered patients from Rheumatology departments of two Egyptian university hospitals aiming to identify determinants of disability and high MHAQ scores in these patients.
Regarding patients’ demographics, in our study age correlated significantly with MHAQ scores while no significant difference was found between males and females. Aging is well related to disability as shown in other studies24–26 usually due to longer disease duration, longer exposure to medications, more co-morbidities, general debility, polypharmacy with more drug interactions and refusal of medications. Patients between 40 and 60 years of age had the highest MHAQs moreover those with disease duration greater than 10 years showed greater disability. In other populations, female sex was found to be associated with greater disability.16 Patients’ height, weight and BMI were not determinants of MHAQ scores in this studied group.
Not surprisingly nearly all parameters of disease activity including morning stiffness, Physician's Global VAS, General Health, TJC, SJC, ESR, and DAS 28 showed significant positive correlation with MHAQ scores. In multiple regression analysis tender joint count showed the highest influence on MHAQ denoting the importance of controlling activity in RA patients as a mainstay in improving patients’ wellbeing. Erosions in X-rays and subluxations detected either clinically or radiologically contributed to higher MHAQ as indicators of joint destruction and dysfunction. So in other words the actual presence of erosions and sublaxations was more associated with disability rather than just seropositivity. These findings were partly different from the results of Krause et al. who found that RF status, inflammatory markers, and joint erosions were not associated in univariate analysis to disability.16 While in many other previous cohort data multiple clinical factors were associated with disability including tender joint count, inflammatory markers including ESR and CRP, and joint damage.24–27
Among all co-morbidities a higher MHAQ was found in patients with ischemic heart disease compared to those without and the difference was statistically significant. RA increases the risk of ischemic heart disease as a chronic inflammatory disease with elevated CRP enhancing atherosclerosis in addition to the burden of corticosteroid use. Ischemic heart disease seemed to interfere with activities of daily livings raising MHAQ scores in such patients.
Psychosocial factors were found to further modify these clinical factors and contribute to the different disease outcomes.28,29 Depression seemed to interfere with activities of daily living and contributed significantly to disability as MHAQ scores were higher in depressed patients compared to those who were borderline and those who were normal. Moreover, MHAQ scores were correlated with depression scores. This was similar to the results of Ji et al. in 2017 who found that participants with disability had more depressive symptoms.18 Surprisingly, on the other hand no significant difference was found between those actually receiving antidepressants and those who were not, although antidepressants use was found to be one of the determinants of disability in other studies.16 This may be explained by the presence of a group of patients who were undiagnosed and not receiving medications. Interestingly, fibromyalgia was not associated with disability as previously demonstrated in other studies.30 Also patients using anxiolytics showed no higher MHAQS than those not. Some studies also demonstrated similar results showing no relation between fibromyalgia and disability in RA patients.16
Illiteracy is still a major problem in developing countries one of the factors that may not be a great concern in other populations. Illiteracy accounted significantly for higher MHAQ scores showing a highly significant difference between MHAQ scores in illiterate and educated patients with different levels of education. Illiteracy is usually associated with lower adherence to medical care and treatment, less understanding of the disease nature in addition to low socioeconomic level and poverty hindering the compliance with medications and the use of more recent and expensive therapies like biologics.
Although it is widely known that disability rates in the biologic era are declining due to better control of inflammation, this is not a rule in all populations and in fact disability still has an impact on many patients.31 The availability of biologics and its optimal use in clinical practice is still an issue. Limitations in our study were that although we are in the era of biologics only 2 patients in our studied sample received biological therapy which is due to financial causes, so we were limited to demonstrate the value of biological therapy in reducing disability in this studied sample. Conventional DMARDS still provide promising results in many RA patients reducing the urge to use expensive biologics.
Reducing disability and improving the quality of life in rheumatoid arthritis patients is still one of the main goals of therapy. It is necessary to determine the main determinants of disability in each population highlighting those that are modifiable or preventable. In our studied sample of Egyptian Caucasians; aging, illiteracy, disease activity, erosions, subluxations, depression and ischemic heart disease were all related to higher disability. It seems promising that many of these are modifiable if properly addressed by physicians. Disease activity being the main factor causing disability should be controlled which in turn reduces erosions and subluxations. Screening for depression and proper use of anti-depressants is of great value in enhancing patient's coping with RA disease. Proper screening and prophylaxis against ischemic heart disease is mandatory. Finally, rheumatologists should work in collaboration with psychologists, cardiologists and other specialties whenever needed.
Conflict of interestThe authors declare no conflict of interests