To determine whether there is an association between serum vitamin D levels and the Disease Activity Index in patients with rheumatoid arthritis (RA).
MethodAn analytical, retrospective, cross-sectional study was performed at the Hospital Luis Vernaza (HLV) and Center for Rheumatology and Rehabilitation (CERER). We included 18 to 75-year-old patients with a diagnosis of RA according to the 2010 classification criteria, and with a 25-hydroxyvitamin D (25 [OH] D) test within the last 3 months. The activity of the disease was assessed with the 28-joint Disease Activity Score (DAS 28) and C-reactive protein (CRP) as an acute-phase reactant. Spearman's rank correlation coefficient was used to establish association between the variables.
ResultsA total of 100 RA patients were studied. The mean vitamin D levels were 32.9 ± 11.5 ng/mL. In all, 45% showed insufficient 25 (OH) D and 55% had normal levels; no deficient vitamin D values were found. According to the DAS28-CRP, patients with low, moderate and high activity had an average vitamin D level of 30.4 ± 10.7, 31.9 ± 10.7, and 31.8 ± 12.1 ng/mL, respectively. There were no significant correlations between the disease activity and the serum vitamin D level (P = .60).
ConclusionIn our group of RA patients, there was no statistically significant correlation between the levels of vitamin D and the activity of the disease, nor were other determining variables associated with vitamin D levels
Determinar si existe asociación entre los niveles séricos de vitamina D y el índice de actividad de la enfermedad en pacientes con artritis reumatoide (AR).
MetodologíaEstudio transversal, analítico, retrospectivo realizado en el Hospital Luis Vernaza (HLV) y Centro de Reumatología y Rehabilitación (CERER). Se incluyeron pacientes entre 18 a 75 años con diagnóstico de AR según los criterios de clasificación 2010, y examen 25-hidroxivitamina D en los últimos 3 meses. La actividad de la enfermedad se evaluó con el DAS 28 (28-joint Desease Activity Score) y el PCR (proteína C reactiva) como reactante de fase aguda. Para establecer asociación entre las variables se realizó por el coeficiente de correlación de Spearman.
ResultadosSe estudiaron un total de 100 pacientes con AR. La media de vitamina D fue de 32,9 ± 11,5 ng/ml, el 45% presentó insuficiencia de 25(OH)D y el 55% niveles normales; no se hallaron valores deficientes de vitamina D. De acuerdo al DAS28-PCR, los pacientes en baja, moderada, y alta actividad tuvieron una media de vitamina D de 30,4 ± 10,7, 31,9 ± 10,7, y 31,8 ± 12,1 ng/ml respectivamente. La actividad de la enfermedad y el nivel sérico de vitamina D no se correlacionaron significativamente (ρ 0,60).
ConclusionesEn nuestro grupo de pacientes con artritis reumatoide, no hubo correlación estadísticamente significativa entre los niveles de vitamina D y la actividad de la enfermedad, tampoco se asociaron otras variables determinantes a los niveles de vitamina D.
Vitamin D is an essential steroid prohormone that chiefly participates in physiological processes that regulate phosphorus and calcium metabolism.1 A deficiency in this vitamin has now been linked to several diseases, such as cardiovascular diseases, inflammatory diseases and mortality rates in the general population.2–4
Vitamin D is measured by determining 25-hydroxyvitamin D (25[OH]D) in the blood.2 The concentration of the same in serum depends on several factors: exposure to sunlight, age, ethnic group, body mass index (BMI), the use of medication (steroids and immunosuppressant drugs), as well as dietary supplements.3
Vitamin D has recently been described as having non-classical actions, indicating that it not only regulates calcium and phosphorus metabolism, but that it is also plays immunological and anti-inflammatory roles by adjusting the growth and differentiation of macrophages, dendrite cells and T- and B-lymphocytes. In turn, it also promotes the inhibition of tumour necrosis factor α and the generation of anti-inflammatory factors (IL-4 and IL-10).5,6
This anti-inflammatory activity has led to research into its role in the regulation of the inflammatory disease progression. It has been shown that the direct and indirect immunomodulating actions of the molecule affect innate and adaptive immune responses. It may also have anti-inflammatory effects through regulation of the biosynthesis of pro-inflammatory molecules in the prostaglandin cascade through the active cells nuclear kappa factor light chain amplifier.6
Rheumatoid arthritis (RA) is a systemic chronic inflammatory autoimmune disease that is characterised by synovitis. Although its aetiology and pathogenesis have yet to be clearly described, many associated factors are known to intervene.7 It has been said that reduced levels of 25(OH)D may be associated with a higher risk of developing RA.8 Its role in the physiopathology of RA and the relationship between vitamin D deficiency and disease activity has been discussed by medical professionals and researchers.9 Nevertheless, some studies have not shown any significant relationship between serum levels of 25(OH)D and RA activity or the development of the disease.10,11
In Ecuador, only one study has been published recently on vitamin D levels in rheumatic patients. 58.8% of the patients in this study had insufficient levels of vitamin D, although these serum levels were not correlated with disease activity.12
The aim of this study is to determine whether there is an association between serum levels of vitamin D and the disease activity index in our patients with RA.
Materials and methodsThis transversal, analytical and retrospective study took place in the outpatient section of the rheumatology department of Hospital Luis Vernaza and the Centro de Reumatología y Rehabilitación. This study was approved by the teaching and medical research department and the Scientific Committees of both health centres; no informed consent was requested because of the nature of the study.
Individuals aged from 18 to 75 years old were included, diagnosed RA according to 2010 American College of Rheumatology/European League Against Rheumatism (EULAR) classification criteria, and patients who had been examined for 25(OH)D in the previous 3 months. Patients with a diagnosis of another inflammatory or connective tissue disease were excluded, as were those with kidney failure, poor intestinal absorption, hyperthyroidism, pregnancy, breast feeding or neoplasia.
Information was extracted directly from virtual clinical histories corresponding to 2016–2017. Demographic data of sex and age were recorded, together with years of evolution, laboratory tests and treatment. C reactive protein was standardised over the erythrocyte sedimentation volume as the acute phase reagent, as it has proven to be the most consistent. A value of ≥5 mg/l was considered positive. The analogue visual pain score was also recorded on a numerical scale from 0−100 mm for the overall evaluation of each patient.
Disease activity was calculated using the data obtained with an activity score index taken from a count of 28 joints (the Disease Activity Score (DAS28)). According to the results of this the patients were classified in 4 categories: high disease activity (DAS28: >5.1), moderate disease activity (DAS28: 3.21–5.1), low disease activity (DAS28: ≤3.2) and remission (DAS28: <2.6).13
To determine serum levels of 25(OH)D immunoanalysis was performed in both centres using electrochemiluminiscence (Cobas, Basel, Switzerland) in ng/ml units. The vitamin D level was considered normal at a serum level of o ≥30 ng/ml, insufficient at from ≤30−10 ng/ml and deficient at levels lower than 10 ng/ml.14
Version 21 of the IBM SPSS (2012) program was used for all of the statistical analysis. Qualitative variables were expressed as frequencies and percentages, and their distribution between groups was compared using the chi.-squared test or Fisher’s test, depending on which was appropriate. Quantitative variables were expressed as averages with their standard deviations, and they were compared between groups using the t-test for independent samples or the Mann-Whitney test, depending on which was appropriate according to the distribution of variables as a function of the dependent variable. Spearman’s ρ coefficient was used to establish correlations between disease activity (DAS28) and serum levels of vitamin D. A P value of <.05 was set as the limit of statistical significance for all of the analyses, with a confidence interval of 95%.
ResultsA total of 306 clinical histories were reviewed of patients with a diagnosis of RA, of which 135 were excluded due to a lack of 25(OH)D test results; there were insufficient data for 46 individuals and 25 fulfilled other exclusion criteria. A total of 100 clinical histories from both medical centres that fulfilled the inclusion criteria were therefore studied.
91% of the patients were women, and the average age of the group was 54.6 ± 13 years old. The average time over which the disease had evolved was 9.1 ± 9 years (Table 1).
Sociodemographic and clinical characteristics and analytical parameters.
| N = 100 | |
|---|---|
| Age (years), average ± SD | 54.6 ± 13 |
| Female sex, n (%) | 91 (91) |
| BMI, average ± SD | 26.4 ± 4.8 |
| Years of evolution, average ± SD | 9.1 ± 9 |
| Inflamed joints, average ± SD | 2.5 ± 3 |
| Painful joints, average ± SD | 2.3 ± 3 |
| DAS28-RCP, average ± SD | 3.1 ± 1.36 |
| DAS28-RCP, n (%) | |
| Remission | 42 (42) |
| Low | 10 (10) |
| Moderate | 32 (32) |
| High | 16 (16) |
| AVS pct 0−100 mm, average ± SD | 30.65 ± 20.8 |
| Rheumatoid factor > 14 U/ml, n (%) | 85 (85) |
| Antipeptide cyclical citrulinate ab > 25 U/ml, n (%) | 72 (72) |
| RCP (≥ 5 mg/l), (%) | 57 (57) |
| Vit. D (ng/ml), average ± SD | 32.9 ± 11.5 |
| Vit D levels (ng/ml), n (%) | |
| Deficiency (< 10 ng/ml) | 0 |
| Insufficiency (10−30 ng/ml) | 45 (45) |
| Normal (> 30 ng/ml) | 55 (55) |
| Calcium + vit. D supplements | 64% |
| Corticoids 5.1 mg (1.25–25) | 77% |
| DMAD | 80% |
| Methotrexate | 59% |
| Biological agents | 25% |
SD: standard deviation; BMI: body mass index; DAS28: Disease Activity Score; AVS: analogue visual scale; RCP: reactive C protein; Vit. D: vitamin D; DMAD: disease modifying anti-rheumatic drugs.
The average number of inflamed joints was 2.5 ± 3 and the average number of painful joints was 2.3 ± 3. The average score on the analogue patient pain scale was 30.65 ± 20.8. RF was positive in 86% of the patients and anti-CCP antibody was positive in 72%. Acute phase reactant CRP ≥ 5 mg/l was found in 57% of the population.
According to disease activity, the average score obtained in the basal DAS28-RCP was 3.1 ± 1.36. Respecting the EULAR disease activity classification, 42% of patients were in remission, 10% had low level activity, 32% had a moderate level of activity and 16% had a high level of activity.
The average concentration of 25(OH)D in the basal determination was 32.9 ± 11.5 ng/ml. In terms of the cut-off points of vitamin D serum levels in the basal determination, 55% of patients had optimum levels, 45% had insufficient levels and no deficient values were found.
64% of the 100 patients in the study were taking oral calcium supplements with vitamin D3; the average dose of calcium in its elemental calcium equivalent was 250.43 ± 58.25 mg (1.1 g citrate, 0.6 g carbonate), while the average dose of vitamin D3 was 505.40 ± 469.00 UI. 77% of the study participants were being treated with corticoids at an average dose of 5.1 mg (1.25–25) of prednisone. All of the patients had been treated with disease-modifying drugs during an average of 9.1 ± 9 years.
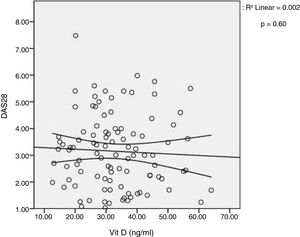
When the levels of 25(OH)D were evaluated according to disease activity as measured by DAS28-CRP, an average of 30.4 ± 10.7 ng/ml was found for low activity, 31.9 ± 10.7 ng/ml for moderate activity and 31.8 ± 12.1 ng/ml for a high level of activity, although no statistically significant differences were found between them (P = .28) (Table 2). Spearman’s ρ coefficient showed no relationship at all between both variables (ρ 0.60) (Fig. 1). Insufficient levels of 25(OH)D were not significantly associated with a high level of disease activity.
Serum vitamin D levels in the different groups according to disease activity measured by DAS28-RCP.
| DAS28 activity | P Value | ||||
|---|---|---|---|---|---|
| Remission, n = 43 | Low, n = 10 | Moderate, n = 32 | High, n = 16 | ||
| Vit. D (ng/ml), average ± SD | 34.8 ± 12.2 | 30.4 ± 10.7 | 31.9 ± 10.7 | 31.8 ± 12.1 | .28 |
DAS28: Disease Activity Score; Vit. D: vitamin D.
The relationships between 25(OH)D and sociodemographic, clinical, analytical and treatment variables were also examined (Table 3). Univariate analysis showed no significant relationship between serum vitamin D levels and the characteristics of these patients.
Univariate analysis con serum vitamin D levels and RA patient characteristics.
| Total series, N = 100 | Serum levels of vitamin D | P Value | |
|---|---|---|---|
| Normal (n = 55) | Insufficient (n = 45) | ||
| Age (years), average ± SD | 56 ± 12 | 53 ± 14 | .18 |
| Female sex, n (%) | 50 (90) | 41 (91) | 1.00 |
| BMI, average ± SD | 25.6 ± 4.7 | 27.3 ± 4.9 | .12 |
| Years of evolution, average ± SD | 10 ± 8 | 9 ± 10 | .20 |
| Inflamed joints, average ± SD | 2 ± 3 | 3 ± 3 | .16 |
| Painful joints, average ± SD | 2 ± 3 | 3 ± 3 | .27 |
| DAS28-RCP activity, average ± SD | 3 ± 1.3 | 3.3 ± 1.4 | .35 |
| DAS28-RCP activity, n (%) | |||
| Remission | 26 (48) | 14 (32) | .44 |
| Low | 5 (9) | 5 (11) | |
| Moderate | 15 (28) | 17 (39) | |
| High | 8 (15) | 8 (18) | |
| AVS 0−100 mm, average ± SD | 30 ± 30 | 40 ± 30 | .29 |
| RCP (≥5 mg/L), average ± SD | 11. 5 ± 15.8 | 13.8 ± 22.4 | .78 |
| Calcium + vitamin D supplements, n (%) | 30 (66.7) | 34 (61.8) | .62 |
| Corticoids, n (%) | 40 (73) | 37 (82.2) | .26 |
| DMAD, n (%) | 38 (84.4) | 42 (76.4) | .32 |
| Methotrexate, n (%) | 26 (57.8) | 33 (60.0) | .82 |
| Biological agents, n (%) | 12 (26.7) | 13 (23.6) | .73 |
DAS28: Disease Activity Score; SD: standard deviation; AVS: analogue visual scale; DMAD: disease modifying anti-rheumatic drugs; BMI: body mass index; RCP: reactive C protein.
When 25(OH)D levels were compared according to whether or not patients were taking a supplement of the same, there was no statistically significant difference between the patients taking supplements and those who were not (32.75 ng/ml vs. 33.19 ng/ml; P = .96). Likewise, there was no significant difference between the DAS28-RCP scores of the patients who were taking vitamin D3 supplements and those who were not (3.25 vs. 3.08; P = .54) (Table 4).
DiscussionThis study did not prove that there is a significant relationship between disease activity measured by DAS28-RCP and serum levels of 25(OH)D. The average level of vitamin D was 32.9 ± 11.5 ng/ml, and almost half of the patients (45%) had 25(OH)D insufficiency in spite of taking vitamin D3 supplements. However, the other half (55%) had normal levels and no vitamin D deficiency was detected.
Ecuador is located on the equator, at a latitude of −0.95, with solar radiation of 10–11 UV,15 so that the skin synthesises vitamin D during the whole year. In spite of this, the Ecuadorian population in general has been show to have a high prevalence of sub-optimum vitamin D levels. A study of the prevalence of vitamin D insufficiency and deficiency in adults over the age of 60 years old on the coast and in the mountains of Ecuador, with 2,375 participants, found that incidences of 67.8% and 21.6%, respectively. Low levels were particularly more common in older women, natives and those living in the Andes Mountains. Nevertheless, when only those living on the coast of the country are analysed, the region where our study took place, significantly lower incidences of 25(OH)D insufficiency (44%–50%) and deficiency (10%–14%) were found.16 These findings may be largely due to the latitude, greater exposure to sunlight and the type of clothing worn in the region.
A recent retrospective study in the city of Guayaquil, Ecuador, of 269 patients with joint pain in their first appointment with the rheumatology department, found an average vitamin D level of 27.29 ± 10.12 ng/dl. 30% of these patients had normal levels, 69% had insufficient levels (29−10 ng/dl) and only 1% had deficient levels (<10 ng/dl).15 Another study by the same author on the prevalence of vitamin D in patients with rheumatic diseases in Ecuador, showed that 41.2% had levels above 30 ng/ml, while levels in the remaining 58.8% were below this range. More particularly, patients with RA had an average of 30.2 ± 18.2 ng/ml of vitamin D in serum.12
Our population of patients reflects characteristics that are typical of a group with RA. The majority are women (91%), with an average age of 54.6 years old and an average duration of the disease of 9.1 years. All of them are receiving treatment and are in follow-up by the rheumatology department. This study did not reveal any significant relationship between disease activity and 25(OH)D serum levels. Even so, it is important to consider that a large proportion of the population studied are in remission or with low disease activity, so it is possible that this lack of correlation could not be extrapolated to a population with a high level of RA activity.
The findings of this study are similar to those described by several authors. A study of 116 patients with RA, 93 women and 23 men, concluded that serum levels of 25(OH)D did not correlate significantly.1 A transversal study with 239 patients in Thailand with RA did not show any relationship between serum levels of 25(OH)D and the number of painful and inflamed joints, the DAS28 score, HAQ and seropositivity for RF and anti-CCP.17 The TOMORROW study in Japan, with 186 patients with RA, who were not treated with vitamin D supplements, did not show any significant correlation between disease activity and the level of 25(OH)D in serum.18 A Latin American study in Argentina found an average of 20.4 ± 0,9 ng/ml vitamin D in 34 women with RA. Although there was no lineal correlation with DAS28, patients with moderate to high levels of activity had lower levels of vitamin D than those patients with low levels of disease activity.19
Nevertheless, other reports do correlate lower vitamin D levels with more severe clinical manifestations of RA, the disease activity index and other rheumatic diseases.20–22 An exhaustive meta-analysis published in 2016 with a total of 24 reports with 3,489 patients showed an inverse relationship between disease activity and serum levels of vitamin D.8 Additionally, they remark that this correlation was more significant in developing countries. The COMORA study, with 1,412 patients with RA in 15 countries, found an average vitamin D level of 27.3 ± 15.1 ng/ml, insufficiency in 54.6% of cases and deficiency in 8.5%. Low levels of vitamin D are associated with age, BMI, educational level, disease activity, corticoid dose and comorbidities.23
The association between vitamin D levels and disease activity is still controversial, and this may be because 25(OH)D levels are easily modified by factors such as geographical region, age, the use of sunblock, dress, glucocorticoids, antimaleria drugs and the immunosuppressant drugs used to treat RA.
On the other hand, this study analysed possible risk factors associated with vitamin D levels in patients with RA, although no association was found in univariate analysis. Although it is true that no association with any variable was found here, other studies have associated reduced levels of vitamin D with sex, BMI and chronic pain.24–26
Although the recommendation to take vitamin D3 supplements for chronic users of glucocorticoids has been widely accepted, the contribution of the latter to the deficiency and its possible association with the disease is controversial.22 It has been suggested that as vitamin D is a secosteroid, it may reduce the immune response in a similar way to steroids.3 Some studies have shown that taking vitamin D supplements modulates the production of proinflammatory cytokines, so that it may even have a cardioprotector effect. It also improves the regulation of vitamin D receptors8 and reduces the development of RA as well as other autoimmune diseases9 and cancer. Vitamin D has also been described as effective in the prevention of falls. The dose and duration of vitamin D3 supplements are not very clear, and cholecalciferol supplements are indicated at doses from 400 UI to 2,000 UI.4,13 The risk of systemic toxicity due to calcium/phosphorus metabolism is rare, and it occurs at doses above 50,000 UI/day, causing hypercalcaemia and hyperphosphatemia.5
As this study compared serum levels of 25(OH)D in patients who were and were not taking vitamin D3 supplements, no statistically significant difference was found. A placebo controlled randomised and double blind study with high doses of vitamin D found no benefit in terms of disease activity or the general health of patients with RA; however, it concludes that the sample size was very small.27 On the other hand, Varenna et al. in their study concluded that vitamin D deficiency is common in patients with RA, even when they receive a suitable dose in supplements.28
On the other hand, the use of calcium supplements has been shown to have cardiovascular side effects, although this finding is still controversial. A correct evaluation of the risk-benefit of adding calcium to the diet is required.
This study has certain limitations. Chiefly, as it is retrospective, the presence of incomplete clinical histories and, moreover, the lack of vitamin D evaluation in all of the patients made it impossible to include them in the analysis, reducing the sample size and making the study deficient in comparison with previous ones. Secondly, the study participants were patients during check-ups and treatment, so that a large proportion of them had disease activity that was classified as low level or in remission, so that it is impossible to compare the results with those of patients with a high level of RA activity.
Our findings are highly relevant for the field under study, as no biological measure has been proven to be sufficient to measure disease activity, so that new biomarkers are needed to function as reliable and objective indicators. This study was performed in patients with RA in everyday clinical practice. The association between vitamin D and disease activity was made using a widely used index that is simple to apply, the DAS28-RCP. Additionally, this study covered the greatest number of patients with these characteristics of all the studies carried out in this country. This paper may therefore have implications for subsequent studies to be used in decision-making regarding the treatment of patients with RA.
Vitamin D, due to its link with autoimmunity and its immunoregulating effects, may be one of the environmental factors that, among others, participate in the pathogenesis of RA. However, it is hard to establish a strong association between vitamin D deficiency and disease activity. Multiple factors such as age, geography, medication, the use of sunblock products and photosensitivity are associated with variations in serum levels of vitamin D; these factors may be linked to the inconsistent findings of previous studies. Even so, the future of vitamin D in autoimmune diseases continues to evolve due to increasing interest in its possible influence on the activity, severity and development of immune diseases.
To conclude, this study showed no significant correlation between disease activity measured by DAS28-RCP and the serum level of vitamin D. Additionally, there was no significant difference between serum level of 25(OH)D in patients who were taking vitamin D supplements and those who were not. Nor was it possible to associate other variables which determine vitamin D levels.
More studies are needed to explain how vitamin D influences RA. This will require larger scale evaluation and even the follow-up of these patients, to determine how any possible association behaves.
Conflict of interestsThe authors have no conflict of interests to declare.
Please cite this article as: de la Torre Lossa P, Moreno Álvarez M, González Guzmán MC, López Martínez R, Ríos Acosta C. La vitamina D no es útil como biomarcador para la actividad de laenfermedad en artritis reumatoide. Reumatol Clin. 2020;16:110–115.