Fibromyalgia is characterized by musculoskeletal pain and asthenia of chronic course. Fibromyalgia patients are often a challenge for the health care community as a whole. Existing studies are often limited to the opinion of rheumatologists or family physicians. With this study we seek to know what are the actions, perceptions and knowledge of health professionals as a whole when caring for patients with this disease.
Materials and methodsDescriptive cross-sectional study, by means of a self-administered and anonymous survey. Distributed mainly in hospital wards and primary care centers. Statistical analysis of the variables collected was performed (p < 0.05).
Results200 surveys were collected, most of them physicians 63.5% (n = 127) or nurses 25.5% (n = 51). 71% of physicians reported using the WHO analgesic scale. 53% (n = 59) use NSAIDs or Paracetamol. Antidepressants are the third drug of choice. Most believe that the referral specialists should be rheumatologists or primary care physicians, a similar percentage, that management should be multidisciplinary. 52% feel discouraged or annoyed when dealing with these patients. Physicians have more negative connotations and believe that the care that the patient receives is mostly influenced by the diagnosis of fibromyalgia, compared to nurses and other professionals.
ConclusionsOur study shows that the lack of knowledge and therapeutic tools generates, to a large extent, frustration and discomfort in health personnel. It is important to develop new approaches to this entity.
La fibromialgia se caracteriza por dolor musculo-esquelético y astenia de curso crónico. Los pacientes con Fibromialgia suelen ser todo un desafío para los sanitarios en su conjunto. Los estudios existentes suelen estar limitados a la opinión de médicos reumatólogos o de familia. Con este estudio buscamos conocer cuáles son las actuaciones, percepciones y conocimientos del conjunto de los profesionales sanitarios al atender pacientes con esta enfermedad.
Materiales y métodosEstudio descriptivo de corte transversal, mediante una encuesta auto-administrada y anónima. Distribuida principalmente en plantas hospitalarias y centros de atención primaria. Se realizó análisis estadístico de las variables recogidas (p < 0,05).
ResultadosSe recogieron 200 encuestas, la mayoría médicos 63,5% (n = 127) o enfermeros 25,5% (n = 51). El 71% de los médicos refirieron utilizar la escala analgésica de la OMS. El 53% (n = 59) utilizan AINE o Paracetamol. Los antidepresivos son el tercer fármaco de elección. La mayoría cree que los especialistas de referencia deben ser los reumatólogos o los médicos de atención primaria, un porcentaje similar, que el manejo debe ser multidisciplinar. El 52% se siente desanimado o molesto al abordar estos pacientes. Los médicos tienen mayores connotaciones negativas y creen que la atención que el paciente recibe está mayormente influenciada por el diagnóstico de fibromialgia, frente a los enfermeros y otros profesionales.
ConclusionesNuestro estudio demuestra que la falta de conocimiento y herramientas terapéuticas, genera en gran medida frustración y malestar en el personal sanitario. Es importante desarrollar nuevos enfoques sobre esta entidad.
Fibromyalgia (FM), included within the central sensitivity syndromes (CSS), is the second most common "rheumatic" disorder, after osteoarthritis.1,2 Its prevalence ranges between 2% and 8% of the world's population,1,3 and in Spain, according to data from the EPISER 2000 study, the rate is 2.37%.3 FM can develop at any age, including childhood, although the average age is between 40 and 49 years.1,3 This disease affects the quality of life of patients, and can be potentially disabling due to its morbidity and because it represents a significant economic burden2,4,5: some studies estimate that between 25% and 50% of patients with FM may have to stop working due to their disease.6 And if we turn to healthcare expenditure, some Spanish multicentre studies show that the expenditure of a patient with CSS-FM may be around 10,000 euros per year, a total of 11bn euros per year in direct and indirect costs, if we consider the total population of the country potentially affected.4
Primary fibromyalgia syndrome is defined as a "rheumatic condition with recognisable clinical features”.7 Within its clinical spectrum, in addition to generalised musculoskeletal pain, we can encounter non-REM sleep disorders, stiffness, fatigue or gastrointestinal problems, such as irritable bowel syndrome, among other conditions.1,7,8 In addition, in many cases depression and anxiety can be associated with this, with no evidence of previous psychological trauma.8,9
The first diagnostic criteria published by the American College of Rheumatology (ACR) in 1990 were based on the perception of pain at certain points (tender points).10 When applying these criteria, the diagnosis of the disease was almost exclusive to women, since they were more sensitive to palpation of these points compared to men.1,3 The new criteria (ACR 2010/2011), which do not take into account the aforementioned points, give a female to male prevalence ratio of 2:1, similar to other conditions of chronic pain.5,9,11
Currently, patients with FM are a challenge for both healthcare professionals and for the healthcare system itself.12 We know that some professionals have an aversion to this condition as a disease category and that this rejection is due, in large part, to the lack of knowledge of its etiopathogenesis and the feeling of frustration derived from the constant treatment failures but also to the overwhelming demand for time on the part of patients, as a result of the need for medical visits, the time required to carry them out and the frequent request for clinical reports.13,14
There are very few studies that reflect the opinion and attitude of healthcare professionals towards FM, and those that do so tend exclusively to assess the perception of physicians, especially rheumatologists and family doctors.15 We believe that objective studies are needed to record the view of healthcare professionals, as a whole, on the approach to patients with this disease. The aim of this study was to describe the personal opinion, attitude and knowledge of the tools (analgesic rating scales, drugs) available to health professionals when visiting patients with CSS-FM at a university hospital and at their centres of reference (primary care centres and public hospitals).
MethodologyParticipants and methodsA descriptive cross-sectional study, carried out between July and October 2021, using a self-administered and anonymous ad hoc survey. The survey was conducted in print format, using Google®'s survey platform. In the first instance, a pilot test was carried out with 30 respondents from the rheumatology and rehabilitation services, to assess the duration and understanding of the questionnaire. During this period, the paper survey was distributed to the hospital’s in-patient floors, and handed out service by service (internal medicine, pulmonology, neurology, psychiatry, intensive care, rehabilitation, rheumatology, emergency, traumatology and anaesthesia-resuscitation) to all professionals who met the inclusion criteria (healthcare personnel involved in care at that time and mainly clinical departments). Similarly, surveys were sent out through a link, coupled with the collaboration of the teaching unit and the consultants (email and WhatsApp® groups) at the Vallparadís public hospital and the main primary care centres (CAP Rambla, CAP Sant Cugat, CAP Valldoreix, CAP Rubí and CAP Sud). A total of 90 printed surveys were sent out or distributed in hard copy (Fig. 1).
Production of the questionnaire and sociodemographic variablesThe questionnaire was prepared with the help of an expert in epidemiology and questionnaires (N.G.G.), who provided guidance on gathering information in the sociodemographic domain and the format in which the answers to the questions could be retrieved (Table 1). In addition to this, focus group meetings were held with the head of the rheumatology service (S.M.P.), who collaborated over drafting the questions and the variables that address issues of clinical practice such as: analgesic assessment scales, beliefs concerning the pathophysiology of the disease, pharmacological and non-pharmacological treatments prescribed, alternative therapies, preconceived ideas about patients, moods, and opinions concerning multidisciplinary patient management, etc. (Table 2). Questions were drafted with qualitative answers, the majority categorical in nature, plus others which were quantitative, ranging from 0% to 100%.
Sociodemographic variables included in the survey.
| Sociodemographic variables | n | % |
|---|---|---|
| Sex | ||
| Male | 60 | 30 |
| Female | 140 | 70 |
| Professional Category | ||
| Doctors | 127 | 63.5 |
| Nurses | 51 | 25.5 |
| Physiotherapists | 15 | 7.5 |
| Psychologists | 4 | 2 |
| Othersa | 3 | 1.5 |
| Service | ||
| FCM | 50 | 25 |
| Rehabilitation | 28 | 14 |
| Internal Medicine | 17 | 8.5 |
| OST | 16 | 8 |
| Rheumatology | 15 | 7.5 |
| Psychiatry | 14 | 7 |
| Emergencies | 10 | 5 |
| Neurology | 6 | 3 |
| Anaesthesia and Resuscitation | 1 | 0.5 |
| Other b | 43 | 21.5 |
| Area of development | ||
| Hospitality | 141 | 70.5 |
| PCC | 54 | 27 |
| Health and Social Centre | 3 | 1.5 |
| Other c | 2 | 1 |
| Median | CI Range (25%–75%) | |
| Age | 34.04 | 28.8−46.7 |
| Years of professional practice | 10 | 3−22 |
PCC: primary care centre; OST: orthopaedic surgery and traumatology; FCM: family and community medicine.
Summary of survey responses.
| Survey | n | % |
|---|---|---|
| 2-A: Have you seen patients with CSS-FM in the past 10 years? | ||
| Yes | 182 | 91 |
| No | 17 | 8.5 |
| No answer | 1 | 0.5 |
| 2-B: How often do you work with these patients? | ||
| At least once a month | 99 | 49.5 |
| At least once a week | 53 | 26.5 |
| No answer | 30 | 15 |
| Daily | 18 | 9 |
| 2-C: Respond only if you prescribe medication. Do you take into account the WHO analgesic scale to indicate treatment? | n | % (out of 200) |
| Yes | 86 | 43 |
| No answer | 79 | 39.5 |
| No | 24 | 12 |
| Don’t know | 11 | 5.5 |
| 2-D: In what proportion, from 0 to 100%, do you think the symptoms have an organic basis? | Mean (50%) | CI Range (25 %–75 %) |
| 40 | 20−60 | |
| 2-E: Do you think the WHO analgesic scale is applicable to these patients? | n | % |
| No | 80 | 40 |
| Don’t know | 73 | 36.5 |
| Yes | 47 | 23.5 |
| 2-F: What treatment(s) do you think is/are beneficial? | ||
| Physical exercise | 164 | 82 |
| Group Therapy | 142 | 71 |
| GABAergic | 71 | 35.5 |
| Antidepressants | 62 | 31 |
| NSAIDs | 52 | 26 |
| Morphic derivatives | 36 | 18 |
| Othera | 14 | 7 |
| Eating habits | 1 | 0.5 |
| 2-G: Respond only if you prescribe medication. What is your first therapeutic option? | n | % (out of 200) |
| No answer | 89 | 44.5 |
| Antidepressants | 38 | 19 |
| Other b | 35 | 17.5 |
| NSAIDs | 26 | 13 |
| GABAergic | 7 | 3.5 |
| Morphic derivatives | 5 | 2.5 |
| 2-H: What percentage of influence do you think the diagnosis of FM has on the care provided? | Average (50%) | CI Range (25%–75%) |
| From emergency professionals | 60 | 30−80 |
| From PC professionals | 50 | 30−70 |
| From the nurse | 50 | 20−70 |
| From colleagues in your unit | 45 | 20−70 |
| From you | 40 | 20−70 |
| 2-I: How do you think the background of FM influences this? | n | % |
| Negatively | 170 | 85 |
| Has no influence | 12 | 6 |
| Positively | 12 | 6 |
| No answer | 6 | 3 |
| 2-J: What do you think should be the specialty(s) of reference? | ||
| FCM | 47 | 23.5 |
| Rheumatology | 46 | 23 |
| Otherc | 46 | 23 |
| Psychiatry | 21 | 10.5 |
| Rehabilitation | 20 | 10 |
| Internal Medicine | 9 | 4.5 |
| Neurology | 6 | 3 |
| Anaesthesia | 3 | 1.5 |
| No answer | 2 | 1 |
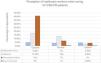
| 2-K: How do you feel about the challenge of caring for FM patients? (Fig. 2) | ||
| Discouraged | 76 | 38 |
| Indifferent | 66 | 33 |
| Irritated | 28 | 14 |
| Good | 23 | 11.5 |
| Enthusiastic | 4 | 2 |
| No answer | 3 | 1.5 |
| 2-L: Do you consider specialised units as treatment? | ||
| Yes | 97 | 48.5 |
| No | 60 | 30 |
| Don’t know | 41 | 20.5 |
| No answer | 2 | 1 |
| 2-M: Do you think the units improve care? | ||
| Yes | 129 | 64.5 |
| Don’t know | 62 | 31 |
| No | 8 | 4 |
| No answer | 1 | 0.5 |
PC: primary care; NSAIDs: nonsteroidal anti-inflammatory drugs; PCC: primary care centre; OST: orthopaedic surgery and traumatology; FM: fibromyalgia; FCM: family and community medicine; CSS: central sensitivity syndrome.
The information was collated on a Microsoft Excel® database. Statistical analysis was run using the Stata SE v. 13.0. Qualitative variables were expressed as percentages and confidence intervals (CIs). Quantitative variables were expressed using medians and interquartile ranges of 25%–75%. Descriptive and bivariate analyses were run by comparing qualitative variables using the chi-square test (χ2) or Fisher's test, and the comparison of quantitative variables using Student's t or Mann–Whitney's U, as appropriate. A p < 0.05 was considered as significant.
ResultsA total of 200 surveys were collected from healthcare providers (88 responses in paper format and 112 in digital format), mostly from doctors and nurses in hospital and primary care, with a response rate of 93.02% (Fig. 1). Sociodemographic, professional and management data is shown in Tables 1 and 2.
Of the 200 professionals who responded to the survey, 70% (n = 140) were women. The mean age was 34 years (interquartile range 25%–75%: 29–47) and the majority were physicians (63.5%; n = 127) or nurses (25.5%; n = 51).
A total of 91% (n = 182) of respondents had seen patients with FM in the last 10 years; 71% of physicians who responded to the prescription question (n = 86/121) reported using the WHO analgesic scale to indicate treatment. The remaining 29% (n = 35) had not used it or were unaware of its usefulness. Of the total respondents, 76.5% (n = 153) believed that the scale was not applicable or doubted its usefulness in patients with CSS-FM. Again, those who prescribed medication had been asked what the first pharmacological treatment indication was, with111 responses obtained from doctors. A total of 53% (n = 59) used NSAIDs or paracetamol. Outside this group, the family of drugs most commonly prescribed as a first treatment option were antidepressants (34%; n = 38).
Turning to non-pharmacological treatment, 82% (n = 164) of the total of respondents believed that physical exercise benefitted patients with EFS-FM while 71% (n = 142) considered that group therapy would help these patients.
On the 0%–100% quantitative scale, respondents were asked to suggest what percentage of symptoms reported by patients had a pathophysiological basis, in their opinion. A median of 40% was obtained (interquartile range 25%–75%: 20−60%).
Regarding specialised units, 50.5% (n = 101) of respondents were unaware of their existence or did not consider them as an option for the treatment of their patients with FM, although 64.5% (n = 129) considered that these units could improve the care of patients with CSS. When asked what the specialty of reference for these patients should be, 23.5% (n = 47) believed that it should be the family doctor, 23% (n = 46) thought the rheumatologist, and another 23% (n = 46) considered that management should be multidisciplinary. The remaining 30.5% (n = 61) opted for rehabilitation specialists (10%; n = 20), internal medicine (4.5%; n = 9), psychiatry (10.5%; n = 21), anaesthesia (1.5%; n = 3), neurology (3%; n = 6), or did not respond (1%; n = 2). Regarding the interest aroused by the subject of patients diagnosed with FM in the professionals whose role it was to treat them, 52% (n = 104) of the respondents stated that they felt discouraged or irritated when having to do so (Fig. 2).
The bivariate analysis showed that physicians referred more negative connotations (despondency or irritation) when visiting these patients, compared to nurses and other healthcare professionals (64.6% vs 29.17% vs 36.36%; p < .001). If these results are analysed by service, it can be observed that, although there is no statistical significance, there is a greater tendency towards negative perception on the part of rheumatology professionals in comparison with primary care professionals and the rest of the services (80.0% vs 42.8% vs 54.1%; p < .06). A total of 85% (n = 170) of the respondents believed that having a history of CSS-FM negatively influenced the care the patient received. This influence was not perceived as much by nurses, compared to physicians (4.76% vs 12.77%; p < .05). No statistical significance was found in the analysis of the treatments indicated for each service (percentages ranged from 4.5% to 34%; p = .1), probably due to a limited sample size.
DiscussionThe present study provides specific information on the attitude of healthcare professionals in our environment regarding the care of patients with CSS-FM, and is, as far as we know, the first to do so by means of a questionnaire structured in two different domains.
As a point to highlight, doubts about the pathophysiological basis of FM as a disease category were evident. This perception that the disease has low organicity and a major psychosomatic component was equivalent to that observed in other studies.14,15 Despite this, only 10% of those interviewed believed that the specialty of reference should be psychiatry.
In terms of treatment approaches, a large number of healthcare professionals believed that the WHO scale is not the best tool to direct analgesic treatment, although, in the absence of other better ones, it is the most widely used. The belief that the origin of pain is not somatic but central justified the choice of antidepressants as the third most prescribed treatment option by our physicians, after NSAIDs and paracetamol, as is also referred to in other series.12,16 The idea that physical exercise and group therapies play a beneficial role in these patients is also evident in the opinion of the respondents, a consideration that is conclusive as a result of the current available evidence.17,18
The poor response to existing therapies, the continuous demands for care, and the high frequency of this type of patient in health centres produce a state of unease that directly harms the patients themselves but also the professionals who attend to them, wearing them out and thus impoverishing the relationship between them.5,14 This state of overload and exhaustion of treatment resources was perceived negatively by professionals and was reflected in our results.19 A high percentage of respondents, especially doctors, felt discouraged or even irritated when caring for their patients with CSS-FM.
The appearance of prejudices towards the patient as a consequence of all of the above considerations can lead to errors of under- and/or overdiagnosis, which may lead to the use of inappropriate treatments that prejudice the patient.8,20 It should be noted that this perception was not shared by nursing staff, and this was not the first time that there have been different approaches and points of view between different disciplines of health professionals.21
Patients with FM constantly consult various different specialties and wander through multiple services in search of alternatives to relieve their symptoms.19 As we have seen, a large number of respondents believe that the care provider of reference for patients with FM should be the primary care provider, although some studies indicate that family physicians manifest some uncertainty over the diagnosis and supervision of these patients.5 The opposite occurs with rheumatologists, who are confident in their diagnosis and management, despite the fact that they do not believe that they should be the service of reference.5 In our study, these facts translate into the existence of a more marked negative perception by rheumatology professionals when caring for patients with CSS-FM, compared to those in family medicine and other services.22
Finally, the present study reflects the real perception of health professionals as a whole when it comes to treating patients with CSS-FM. It is important to further deepen the scientific knowledge of this disease in order to offer those who treat it the necessary tools to reach a correct diagnosis and ensure adequate management of patients, so that effective treatment options can also be provided to improve their quality of life. In this regard, the Spanish Society of Rheumatology has prepared a recent in-depth article and it deserves to be cited for the benefit of the readers’ knowledge (Rivera Redondo et al.).23 It should also not be forgotten that people affected by CSS-FM deal with symptoms that disable and depress them on a daily basis, upsetting their daily life and their home and work environment.
Limitations of the studyThe methodology in the form of a survey does not enable us to work out the cause behind the data obtained. Although the results depended on the subjectivity of the respondent, we believe that the fact that it was anonymous and free of any subsequent judgments could lead to reliable answers. On the other hand, although the sample size was small, a high response rate was obtained, so the conclusions were representative of our population of professionals who care for these patients, although we cannot ensure external validity for other healthcare centres.
ConclusionsOur study provides novel and relevant data on the interaction of various health care providers, both in primary care and hospital specialties, with patients diagnosed with FM. An example of this was the disparity of opinions between medical practitioners and other healthcare professionals. The high proportion of despondency among those who deal with this disease and among patients who suffer from it was also directly objectified through opinion. We conclude that the lack of pathophysiological knowledge, as well as the absence of truly effective treatment tools, create frustration and irritation among healthcare personnel. By shedding light on this situation, the need for new perspectives on the approach to these patients becomes evident.
Ethical responsibilitiesConsent was required to participate in the survey. This was obtained by a note of reference located at the top of the survey page, just below the title. No personal data was collected from the participants, with the exception of their date of birth. The study went before the ethics committee (CEIM) of our institution and was accepted by that committee on June 17th, 2021 under the following sponsor code: 2021-075-1.
FundingThis work was not the beneficiary of any funding.
Conflict of interestThe authors declare that they do not have any conflict of interest.
To Dr Nuria Giménez Gómez, Associate Lecturer, Autonomous University of Barcelona (UAB).