Joint hypermobility is the largest amplitude of the normal range of motion of joints, due to increased compliance of the ligaments and joint capsules.1 When joint hypermobility is associated with clinical and/or extra-articular manifestations, the joint hypermobility syndrome (JHMS) or benign joint hypermobility syndrome occurs, defined by the revised Brighton2,3 (Table 1) criteria. Moreover, according to the classification criteria of the Ehlers-Danlos syndrome (EDS) currently employed,4 the former EDS type iii is now classified as hyperlax or hypermobile EDS, and would be virtually identical to the benign joint hypermobility syndrome.2 We report the case of a woman with a hyperlax EDS.
Brighton Criteria for the Diagnosis of Benign Joint Hypermobility Syndrome (1998).
| Main criteria |
| Four or more points of the Beighton criteria |
| Joint pain for longer than 3 months in at least 4 joints |
| Minor criteria |
| One to 3-points of the Beighton criteria |
| Joint pain in one, 2 or 3 joints or back pain or dorsal root pain for more than 3 months |
| Dislocation or subluxation of more than one joint, or one joint more than once |
| Three or more periarticular lesions (tennis elbow, tenosynovitis, bursitis, etc.) |
| Marfanoid habitus (tall, thin, arachnodactyly, etc.) |
| Skin abnormalities: striations, hyperextensibility, thin skin, etc. |
| Ocular signs myopia or Antimongoloid type |
| Varicosities or hernias or uterine or rectal prolapse |
The benign joint hypermobility syndrome is diagnosed if 2 main criteria, or one major and 2 minor, or 4 minor criteria are met. Two minor criteria will suffice if a first degree relative is affected. Major criterion number 1 and minor criteria number 1 and 2 and major criterion 2 and the minor criterion 2 are exclusive.
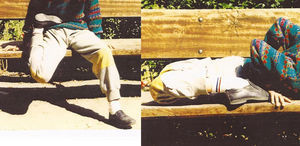
The patient is a 27 female graphic designer with a family history that highlights her father with joint hypermobility mainly of the hands, a sister aged 20 and a paternal cousin of the first degree with symptoms of hypermobility, but not studied. She has a history of two pregnancies, an abortion and a healthy 7-year-old daughter, who also has a joint hyperlaxity documented by a Beighton 9/9 hypermobility. From birth the patient showed “extreme” mobility of the joints, which delayed the start of gait and led to repeat sprains since childhood. She frequently performed joint hypermobility maneuvers (Fig. 1). She had bruises and frequent epistaxis. Study of coagulation and platelet function were performed before birth, being normal. Since 3 years prior presents repeating subluxations in the knees and shoulders, so has to travel in a wheelchair for long distances. She presents relapsing tendinopathy of the wrists after holding weight or maintaining positions for writing or drawing, so she cannot practice her profession. Systemic examination was normal. No skin elasticity or transparency was observed, nor was ecchymosis, atopic dermatitis on elbow flexure lesions; Beighton test was 9/9. Passive and active joint mobilities in all joints were explored, over the normal range (Fig. 2), leading to subluxation. The echocardiogram was normal.
DiscussionJoint hypermobility is less a skill than a problem; there is also a relative confusion in terminology as we stated in the introduction. The EDS includes a group of inherited, rather heterogeneous disorders of connective tissue regarding their clinical and genetic transmission, in which the main finding is, to a greater or lesser extent, vascular, cutaneous, ligamentous and internal organ fragility. The most common types are the classic EDS (by a defect of collagen type v, being a mutation in the COL5A1 and COL5A2 genes in half of the cases), vascular EDS (by a defect in type III collagen, with anomalies in the COL3A1 allele) and hypermobile or hyperlax EDS. But it is increasingly clear that the current classification is inadequate and many patients have overlapping forms of EDS, so they cannot be unambiguously classified into one of5 recognized subtypes 6.
Hypermobile EDS (equivalent to benign joint hypermobility syndrome) is characterized by skin changes (soft, elastic, abnormal scarring), joint pain, myalgia, tendonitis and recurrent subluxations. In children it often delays walking, leads to body contortions (“rubber children’) or ‘juggling acts” with hands.6 No inflammatory signs, laboratory tests or specific radiological signs are found. The precise biochemical alterations and the genetic defects are not well known; there is a family history and it was once considered of autosomal dominant inheritance, but some recent studies indicate that in less than 10% of cases there may be a defect in tensacin gene x, a glycoprotein in the extracellular matrix which is manifested recessively. Its controversial association with mitral valve prolapse, which does not seem to be more prevalent in hypermobile EDS, shows a higher prevalence in a study of patients with hypermobility.2 Its correlation has been demonstrated with chronic fatigue syndrome, fibromyalgia7 anxiety, depression, panic attacks, agoraphobia2,6,8 dysautonomia and osteoporosis in premenopausal women.9
The diagnosis of this syndrome is clinical and confirmed using Brighton criteria.3 Treatment includes preventive measures, rest, physiotherapy and analgesia in the acute phase and then a multidisciplinary rehabilitation approach to restore normal range of joint motion, correct movement dysfunction, improve joint stability, physical condition and mental impact by benign hypermobility. Again adjectives demonstrate how relative they can become.
Ethical ResponsibilitiesProtection of people and animalsThe authors declare that no experiments have been performed on humans or animals.
Data confidentialityThe authors declare that they have followed the protocols of their workplace regarding the publication of data from patients and that all patients included in the study have received sufficient information and have given their written informed consent to participate in the study.
Right to privacy and informed consentThe authors have obtained informed consent from patients and/or subjects referred to in the article. This document is in the possession of the corresponding author.
Conflict of InterestThe authors declare no conflicts of interest.
Please cite this article as: Pantoja Zarza L, Díez Morrondo C, Alexis D. Síndrome de Ehlers-Danlos hiperlaxo: ¿hipermovilidad benigna? Reumatol Clin. 2014;10:189–190.