Hematogenous vertebral osteomyelitis (HVO) is a rare entity (in Spain, 9 new cases per million inhabitants/year),1 yet its incidence is increasing in relation to population aging, immunosuppressive use, increasing nosocomial bacteremia and other predisposing factors, especially diabetes mellitus.1–3 Although there are many possible causal agents1–5 pyogenic Gram-positive bacteria, specifically Staphylococcus aureus, is the most common etiology (up to 51% in some series).1,2,6 Although mortality is rare,it is associated with high comorbidity, often related to the occurrence of complications secondary to delayed diagnosis.1,3 We present a case of extensive HVO due to Parvimonas micron (P. micron) with large epidural involvement, prevertebral abscess, myelopathy and bilateral pleural effusion.
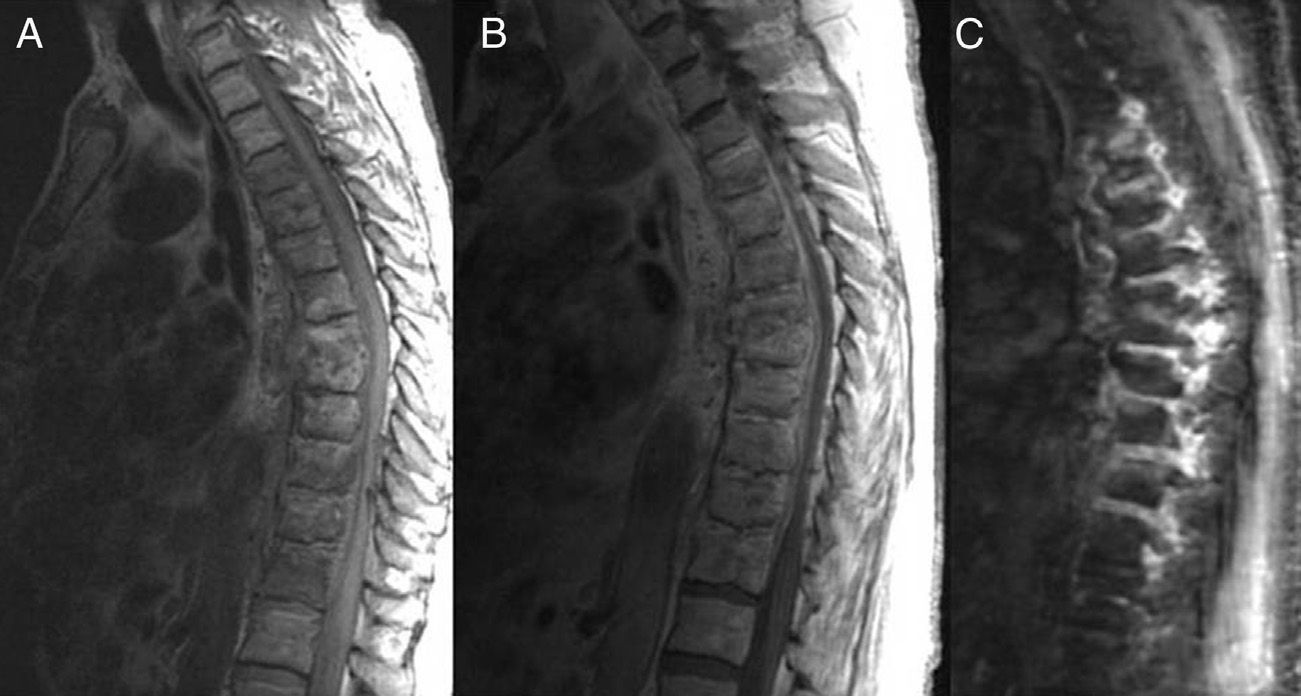
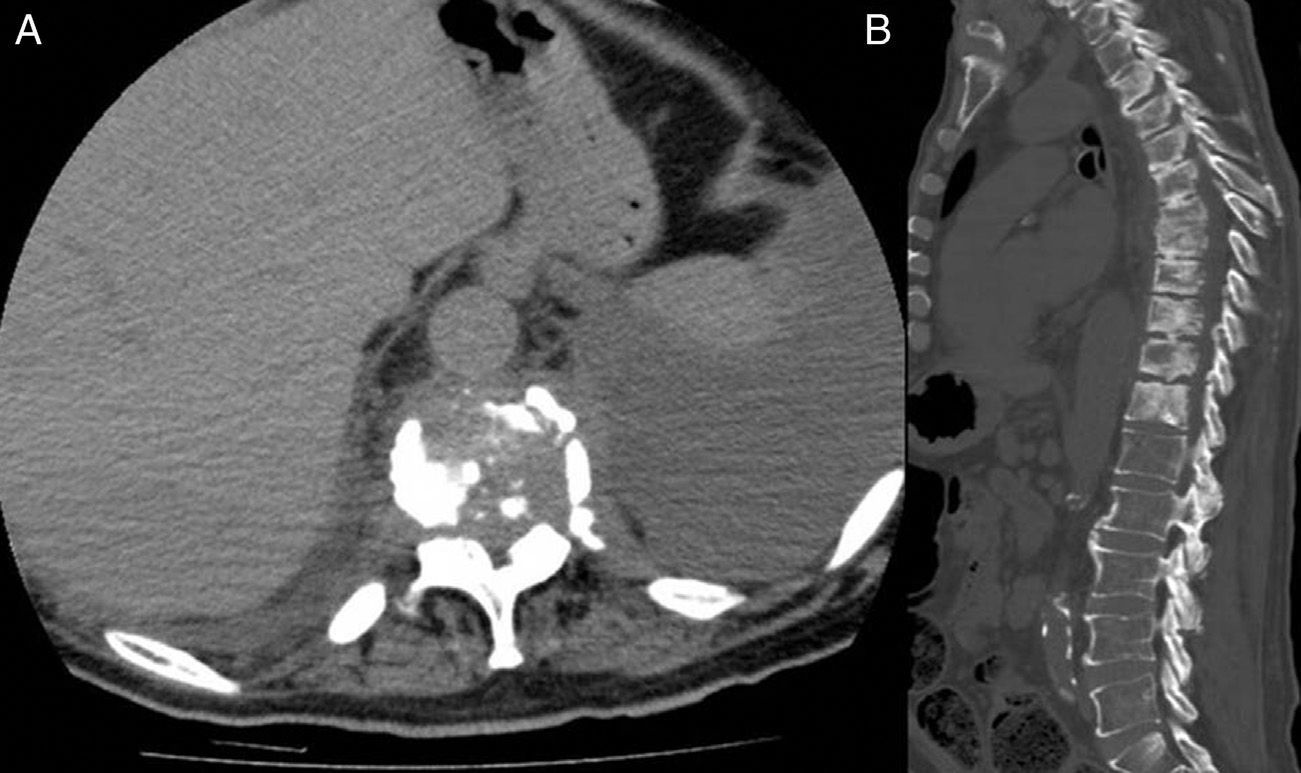
The patient was a 62-year-old male, former smoker, hypertensive, longstanding diabetic, hemiparetic and aphasic after a left frontoparietal hemorrhagic stroke which occurred a year earlier. The family consulted us due to progressive deterioration with back pain, unstable sitting and left lower limb weakness lasting for the previous 6 months.Physical exam: no fever, blood pressure 120/70 mmHg, heart rate 80 bpm.Heartbeat rhythm had no murmurs, vesicular murmur was decreased in both lung bases.The patient had generalized amyotrophy. The patient had paresis, Achilles clonus and Babinski on the left leg. There was residual right hemiparesis and aphasia. Other exploratory findings were unremarkable. Laboratory data: hemoglobin 11.7g/dl, leukocytes 11500mm−3 neutrophils 8900mm−3 platelets 447000mm−3; ESR 61mm/h and CRP86.10mg/l. Hepatic and renal biochemistry, electrolytes, total protein and glucose were within normal limits. Cranial CT showed no new lesions. The electromyogram showed sensorimotor axonal and symmetrical polyneuropathy and the MRI of the lumbar spine showed a correction of lordosis and unobtrusive spondylosis without radiculopathy.Spine x rays revealed disorganization of the D7–D8 intervertebral space, with effacement of the discs and decreased height of both vertebral bodies. MRI of the thoracic spine showed significant signal alteration of vertebral bodies from D3 to D12 and paraspinal soft tissue and adjacent epidural tissue being the most affected at the D7–D8 level, with a prevertebral abscess at this level and increased signal by epidural spinal cord compression (Fig. 1). CT with multiplanar reconstructions confirmed the findings of spinal osteomyelitis with epidural and paraprevertebral extension and spondylodiscitis of D7–D8, and also revealed bilateral, predominantly left, pleural effusion (Fig. 2). Diagnostic thoracentesis objectified features of chronic inflammatory process in the cytology. Blood cultures were negative. Percutaneous biopsy of the intervertebral D7–D8 space was conducted with negative microbiological tests for mycobacteria and positive for P. micron, and a histology indicative of nonspecific chronic inflammation. Given the patient comorbidity and the rejection of the family to receive intravenous antibiotic therapy, we chose a conservative approach based on clindamycin 600mg orally every 8h. After 4 months and improved overall strength of the left leg, the backache disappeared and acute phase reactants decreased (ESR 12mm, 12.9CRPmg/l). On control MRI no significant changes were seen.
MRI of thoracic spine, sagittal spin echo T1 sequences, with (A) and without contrast (B), and STIR (fat suppression) (C) sequence, where extensive epidural and paravertebral soft tissue involvement is observed reducing the diameter of the spinal canal, with a small D7–D8 prevertebral abscess.
P. micra (formerly Peptostreptococcus micros) is a type of strict anaerobic gram-positive cocci, unsporulated and an oropharyngeal commensal.7 Although it has been associated with polymicrobial infections (intracranial abscesses, sinus infections and periodontitis)8 involvement in vertebral osteomyelitis is rare, with only 2 cases reported in the literature.1,5
In the last decade, an increase in anaerobic bacteremias germs has been described, which seems to be related to the increasingly frequent health care to patients with complex comorbid processes underlying changes in susceptibility patterns of these pathogens and better techniques for detecting microbial presence.9 In our case, we should consider a spontaneous hematogenous spread from the oropharynx or promoted by bronchial aspiration in the context of coma accompanying acute stroke months earlier; other possible sources were quite unlikely, given the quality of the commensal germ, the clinical course and the lack of examination signs and/or microbiological data to support endocarditis or other satellite infectious process. The diagnostic delay due to the lack of suspicion when faced with insidious and atypical symptoms in a patient already weakened and with difficulty communicating and intercurrent processes that delayed imaging tests, justify the extent of involvement and the chronic nature of the process. The concomitant presence of inflammatory pleural effusion is a very rare finding,10 which was interpreted in the context of chronic pleural irritation secondary to paravertebral involvement. The left pyramidal monoparesis was consistent with the finding of compressive myelopathy. Although treatment improved clinical and laboratory parameters, the chronic nature of the injury, the absence of debridement and drainage of the abscessed tissue, and lack of parenteral antibiotic therapy justify the absence of radiological improvement.
Please cite this article as: García González M, Muñiz Montes JR, García Rosado D, Bustabad Reyes S. Osteomielitis vertebral hematógena multisegmentaria por Parvimonas micra y derrame pleural secundario en un paciente diabético. Reumatol Clin. 2014;10:191–192.