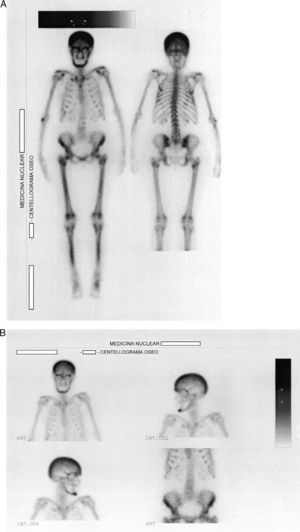
Endocrine disorders often have rheumatic manifestations, which can sometimes be the first characteristic of the disease. Among these disorders is hyperparathyroidism, which is classically manifested by the presence of kidney stones, fractures, pancreatitis and psychiatric disorders.1 A woman aged 57 was admitted due to widespread pain, sleep disturbances, headache, fatigue and loss of function of upper and lower limbs. Nine months earlier she had been diagnosed with fibromyalgia, having been treated with fluoxetine 20mg/day and clonazepam 1mg/day without improvement. Laboratories prior to admission showed an erythrocyte sedimentation rate (ERS) 31mm/h, hematocrit 35%, hemoglobin 11mg/dl, CPK 62U/l (VN to 165), C reactive protein (−). At the time of admission, the physical examination of the patient showed no peripheral arthritis, muscle strength was normal in the neck and pelvic girdle, and she presented positive trigger points for fibromyalgia (18/18). Analysis showed ESR 49mm/h, serum calcium 13.5mg/l (VN 8.5–10.5), phosphate 1.9mg/l (VN 2.4–4.1), alkaline phosphatase 900U/l (230–460V). Radiographs showed radiolucent lesions in the clavicle and salt and pepper lesions of the skull. The abdominal ultrasound showed a 6mm kidney stone at the middle calyx of right kidney. The chest CT observed lytic sack lesions, and a neck tumor formation that could be from the thyroid or parathyroid. The patient underwent a bone scan with 99mTc, which showed an increased uptake in the skull, the maxillofacial region, posterior rib areas and long bones of the lower limbs (Fig. 1A and B). The levels of parathyroid hormone (PTH) were 1900pg/ml (VN 42–72). Diagnosed with primary hyperparathyroidism, she underwent a resection of the tumor, with a pathology report parathyroid follicular adenoma. Musculoskeletal symptoms, as well as fatigue and sleep disorders, showed marked improvement after surgical treatment. Primary hyperparathyroidism is the third most frequent endocrine disorder in women between 50 and 60 years and the most common from is the single adenoma (80%–85%), followed in frequency by 4-gland parathyroid hyperplasia (10%–15%) and to a much lesser degree by parathyroid carcinomas (less than 1%); sometimes, this disorder may be part of a hereditary syndrome such as multiple endocrine neoplasia type 1 or 2.2,3 Current diagnostic methods rely on elevated serum calcium levels, found in 70%–80% of patients who are asymptomatic at the time of diagnosis and have the disease detected by the incidental presence of hipercalcemia.1,2 Patients may complain of nonspecific disorders, such as fatigue, depression, weakness, memory loss, sleep disturbances and altered concentration.4 The presence of arthralgia and myalgia, particularly affecting the proximal muscles of the shoulder and pelvic girdles, mimicking polymyalgia rheumatica, is frequent, and arthritis can also mimic gout or pseudogout.5,6 Our patient reported sleep disturbances, fatigue, strength loss of arms and legs and generalized musculoskeletal pain; symptoms did not improve with drug therapy. Other clinical manifestations are at the neuromuscular level,7 paresthesias and cramps. The improvement of symptoms after excision of the adenoma suggests the causal relationship with hyperparathyroidism. Thomas and Podduturu reported a patient with a previous diagnosis of fibromyalgia who received multiple treatments with no improvement, in whom high levels of PTH were found, receiving treatment for hyperparathyroidism, which led to the resolution of pain.8 In conclusion, we believe that routine determination of serum calcium and phosphorus should be performed in patients with generalized pain syndromes in which fibromyalgia or polymyalgia rheumatica is suspected.
Please cite this article as: Borgia AR, et al. Hiperparatiroidismo, una causa olvidada de dolor músculo-esquelético difuso. Reumatol Clin. 2012. http://dx.doi.org/10.1016/j.reuma.2012.02.008.