Sarcoidosis is an inflammatory disease with unknown cause characterized by non-caseating granuloma formations. It may present with bilateral hilar lymphadenopathy, skin lesions, eye and musculoskeletal system involvement. Hypercalcemia and hypercalciuria are important electrolyte imbalances resulting from sarcoidosis and sometimes they may cause nephrolitiasis and kidney failure. Hyponatremia, although being quite rare, has been found in some patients with sarcoidosis. Herein, we have reported a patient with neurosarcoidosis who presented with hyponatremia and responded well to corticosteroid treatment.
La sarcoidosis es una enfermedad inflamatoria, de causa desconocida, que se caracteriza por la formación de granulomas no caseificantes. Se puede presentar con linfadenopatía hiliar bilateral, lesiones en la piel, en los ojos, y la implicación del sistema musculoesquelético. La hipercalcemia y la hipercalciuria son importantes desequilibrios electrolíticos resultantes de la sarcoidosis, y algunas veces pueden causar nefrolitiasis e insuficiencia renal. La hiponatremia, a pesar de ser bastante rara, se ha encontrado en algunos pacientes con sarcoidosis. Aquí, hemos informado de un paciente con neurosarcoidosis que se presentó con hiponatremia y respondió bien al tratamiento con glucocorticoides.
Sarcoidosis is an inflammatory disease with unknown cause characterized by non-caseating granuloma formations.1 Although the pathogenesis of disease is not clear yet it is thought that there is a Th1 cell-mediated immune response against unknown antigens. Environmental, genetic and infectious agents are discussed in the pathogenesis of sarcoidosis. Non-caseating granuloma formation in the biopsy specimen material may be used as diagnostic tool. It may present with bilateral hilar lymphadenopathy, skin lesions, the involvement of eye and symptoms on the locomotor system. Sarcoidosis is a heterogeneous disease which may be seen in different ethnic origins with different prevalances.2 The disease appears to begin at the fourth decade of life, and is more frequent in woman. Sarcoidosis is a chronic granulomatous disease that may present with different clinical findings. The pathognomonic histological finding of disease is the presence of non-caseating granulomas.3 These granulomas may form in almost any organ and system of the body. Neurological involvement may occur in 5–10% of patients. Sarcoidosis may affect brain, spinal cord, and any part of the central or peripheral nervous system. Neurosarcoidosis typically lead to cranial nerve involvement, basilar meningitis, myelopathy and diabetes insipidus as well as anterior hypothalamic disease symptoms.4 Facial nerve paralysis is the most common cranial neuropathy. Due to hypothalamic-pituitary involvement, diabetes insipidus related symptoms like polydipsia and polyuria can occur. Granulomatous inflammation and white matter abnormalities can also be seen in MRI.5 The relationship between hyponatremia and neurosarcoidosis was reported in some studies.6,7 However, the number of studies is very low. Herein, the relationship with hyponatremia in a patient with neurosarcoidosis was reported.
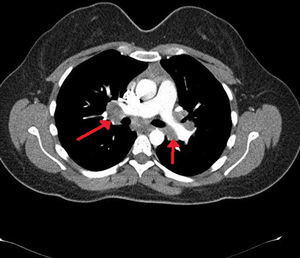
Case reportA 64-year-old female patient, is being followed with the diagnosis of neurosarcoidosis for nearly 30 years. Patient presented with the complaints of arthralgia, fatigue, drowsiness and forgetfulness and was admitted to our rheumatology department. She had hypertension in her medical history. The physical examination revealed tenderness in the knee and ankle joints. Other systemic examinations were found to be normal. In the laboratory investigation, serum Na: 119mg/dl (normal 135–140mg/dl), serum ACE: 102mg/dl (normal <45mg/dl), serum calcium and serum hydroxyvitamin D levels were normal. Liver, kidney function tests and the urine analysis were normal. Nephrology consultation and the research on etiology was conducted. On thorax CT, bilateral hilar lymphadenopathy was seen (Fig. 1). Due to the history of neurosarcoidosis, cranial and pituitary MRI were ordered for a possible pituitary involvement. In the brain MRI, millimeter-sized chronic microangiopathic ischemic signal changes were observed in the periventricular deep white matter; no mass image was seen in the pituitary MRI. EMG of lower extremities was performed and it was consistent with polyneuropathy. Endocrinology consultation was done; in tests performed: Cortisol: 7.74g/dL (normal 6.2–19.4g/dl), ACTH: 1.68pg/ml (normal 0–46pg/ml), prolactin: 14.30ng/ml (normal 4.79–23.3ng/ml), freeT4: 1.92ng/dI (normal 0.93–1.71ng/dl), freeT3: 2.57pg/dl (normal 2–4.4pg/dl), TSH: 1.71μIU/ml (normal 0.27–4.2μIU/n). A pathology that could explain the hyponatremia was not detected in any research and it was thought to be associated with the underlying neurosarcoidosis. Despite fluid and electrolyte therapy, the serum Na did not increased. Prednisone 40mg/day, was started. One month later, in control laboratory tests, patient was clinically stable, and had normal level of serum Na. The patient's general condition is good and she is followed-up in the outpatient clinic.
DiscussionSarcoidosis is a chronic inflammatory disease with unknown etiology, characterized by noncaseating granulomas and often shows multisystemic involvement. Five to ten percent of patients have neurological involvement.6 Neurosarcoidosis may present with various neurological symptoms, physical examination, brain MRI, laboratory and histological examination are required to reach a diagnosis.7 In neurosarcoidosis, severe hyponatremia may develop due to the hypopituitarism and secondary hypocorticolism. In the literature, neurosarcoidosis associated with hyponatremia has been rarely reported. In a study on headache and mental status changes, brain biopsy revealed the neurosarcoidosis, characterized by noncaseating granulomas in the subependymal zone, as the underlying cause of cerebral salt wasting syndrome and central nervous system (CNS) inflammation. Sarcoidal granulomas can be seen in the meninges, hypothalamus, brain stem, subependymal space, choroid plexus, peripheral nerves and also in the blood vessels that feed the nerves. Hyponatremia due to CNS damage can occur. The most common cause is syndrome of inappropriate anti-diuretic hormone(ADH) secretion. The cause of persistent CNS inflammation in these patients was found to be neurosarcoidosis. Neuropsychiatric symptoms have also occurred rarely.8 In another study, sarcoidosis has been shown to cause the syndrome of inappropriate ADH secretion, and hence the hyponatraemia. After 1 year with the corticosteroid treatment, decline in both the findings of syndrome of inappropriate ADH secretion and the systemic findings of sarcoidosis was observed.9 In a study investigating the relationship between sarcoidosis and pituitary mass, a patient diagnosed with pulmonary and ophthalmic sarcoidosis was presented with fatigue and vomiting complaints. Laboratory tests showed hyponatremia and the brain CT detected a suprasellar mass. Since MRI illustrates the intrasellar and suprasellar mass and also the pituitary stalk thickening, the clinical and radiological findings strongly support the hypothesis that the mass in the pituitary is due to the sarcoidosis.10 Unlike this case, in our patient although the pituitary mass was not detected, after other reasons of hyponatremia were excluded, a response to corticosteroid therapy suggests that it may be associated with neurosarcoidosis. The reason of hyponatremia in our case was thought to be neurosarcoidosis. Indeed, hyponatremia was improved after the corticosteroid therapy.
In conclusion, we report a case with neurosarcoidosis presenting with hyponatremia. Sarcoidosis is one of the diagnoses that should be kept in mind in patients presenting with electrolyte imbalance.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of dataThe authors declare that they have followed the protocols of their work center on the publication of patient data.
Right to privacy and informed consentThe authors must have obtained the informed consent of the patients and/or subjects mentioned in the article. The author for correspondence must be in possession of this document.
Conflicts of interestThe authors declare no conflicts of interest.