Cherubism is a rare disorder with autosomal dominant inheritance. It is classified as a benign fibro-osseous lesions and may involve either facial bone. Its typical dentofacial deformities are caused by mutations in the SH3BP2 gene. The protein encoded by SH3BP2 had a significant role in the regulation of osteoblasts and osteoclasts. Accordingly with the radiological findings, differential diagnoses includes fibrous dysplasia, giant cell granuloma, osteosarcoma, juvenile ossifying fibroma, fibrous osteoma, odontogenic cyst and hyperparathyroidism. The aim of the present report is twofold. First, we examine the importance of the proper management of these cases. Second, we describe this rare syndrome with the goal of proposing suitable treatments.
El querubismo es una enfermedad rara. Presenta herencia autosómica dominante y es clasificada como una enfermedad fibroósea benigna. Las deformidades típicas de esta dolencia se deben a la alteración del gen SH3BP2 y pueden afectar a cualquier hueso del macizo facial. La proteína codificada por este gen es fundamental para el correcto funcionamiento de osteoblastos y osteoclastos. El diagnóstico diferencial debe incluir: displasia fibrosa, granuloma de células gigantes, osteosarcoma, fibroma osificante juvenil, fibroma osteoide e hiperparatiroidismo.
Cherubism is an uncommon disease classified as a benign fibro-osseous pathology. It presents an autosomal dominant inheritance and normally appears during childhood.1 Typical dentofacial deformities of this disorder are caused by mutations in SH3BP2 gene on chromosome 4 (SH3-domain binding protein 2).2 The protein encoded by SH3BP2 is essential for bone metabolism. This results in formation of numerous cysts that affect facial bones. Specifically, lower jaw is often the most afflicted by pathology.3
Cherubism is self-limiting with regression after puberty. After age 30 lesions are often replaced with bone and radiologically not visible.4 However, despite the relatively benign behavior, it might provoke major problems. Ocular complications are among the most serious and feared in these patients. In this light, orbital involvement does not occur after puberty but may still be present. Thus, patients with cherubism should be frequently examined by an ophthalmologist in order to perform a routine screening of the visual acuity.5
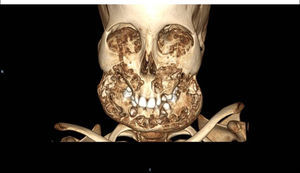
Case reportA 7 year old male visited the outpatient department of oral and maxillofacial surgery of our Hospital. Parents referred bilateral progressive swelling of jaw bones. Physical examination shows asymmetry of the face with gross chubby appearance. Deformities were more pronounced on jaw bone and on left size. In addition, patients presented upward gaze and bilateral submandibular lymphadenopathy. In view of these findings, we decided to perform a panoramic radiograph and a head CT scan in order to guide the diagnosis. This tests showed several multilocular cysts in all four quadrants of jaws (Fig. 1). No significant alteration was observed with biochemical analysis of calcium metabolism. Finally, an incisional biopsy of cystic tissue was carried out. Histopathological examination evidenced many multinucleated giant cells. By correlating clinical, radiographic and histopathological features a final diagnosis of cherubism was made. After diagnosis, patient was referred to an ophthalmologist with the aim of beginning a routine screening of the visual acuity. No alteration was evidenced by eye examination. Against this backdrop, we decided to keep a conservative attitudes.
DiscussionCherubism results from replacement of bone with multilocular cysts due to osteoblasts and osteoclasts malfunctioning (Figs. 2 and 3, Supplementary Material). As already mentioned it represent a benign fibro-osseous pathology and it should be distinguished from central giant cell granuloma (CGCG), multiple giant-cell lesion syndrome, fibrous dysplasia, brown tumors and Ramon syndrome and hyperparathyroidism.6 Differential diagnosis is based on specific clinical, radiological and anatomo-pathological features.
Although the severity of pathology, no effective treatment exists. Therapy strategies include: (a) surgical treatment; (b) medical treatment.
In relation to surgery, the strategy of wait and see is the most commonly used in these patients (Table 1, Supplementary Material). Surgery before puberty is only recommended in case of serious deformity or severe psychological impact.7
In relation to medical treatment, there is no evidence for an effective medical treatment. Recently, Tacrolimus demonstrated great results in one case.8 Calcitonin might also be useful.9 These positive effects seem to be related with the inhibition of bone reabsorption. On the other hand, radiotherapy and adalimumab (TNF-α antagonist) have not proven utility.
ConclusionThis report contains three central point. First, a conservative attitudes are recommended until after puberty. Second, the diagnosis of cherubism is based on the presence of specific clinical, radiological and histological characteristics. Notwithstanding, a genetic study might be useful to achieve a safe diagnosis in borderline cases. Indeed, treatment substantially differs across benign fibro-osseous tumors. Third, further study should be undertaken regarding the effect of medical treatment in this disorder.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of dataThe authors declare that no patient data appear in this article.
Right to privacy and informed consentThe authors declare that no patient data appear in this article.
Financial assistanceAuthors not received financial assistance.
Authors’ contributionsAll authors participated in the creation of manuscript.
Conflict of interestThe authors declare that they have no competing interests.