IgG4-related disease is characterised by mass lesions, a dense lymphoplasmacytic infiltrate with immunohistochemical positivity for IgG4, storiform fibrosis and, frequently, elevated serum IgG4 levels. It can be multisystemic; however, myocardial involvement, which is objectively determined by imaging tests, has not been described in the medical literature. We report the case of a man with IgG4-related disease with possible myocardial involvement, detected by cardiac magnetic resonance. This raises the question of a differential diagnosis with other diseases such as sarcoidosis and Fabry disease, the differential diagnosis of which is of great importance due to its therapeutic impact.
La enfermedad relacionada con el depósito de IgG4 es una entidad caracterizada por lesiones tumefactas, infiltrado denso linfoplasmocítico con positividad inmunohistoquímica para IgG4, fibrosis estoriforme y, frecuentemente, niveles séricos elevados de IgG4. Puede cursar con afectación multisistémica; sin embargo, la afectación miocárdica, objetivada mediante pruebas de imagen, no ha sido descrita en la literatura médica. Se presenta el caso clínico de un varón afecto de enfermedad relacionada con IgG4 con posible afectación miocárdica, detectada a través de cardiorresonancia magnética, que plantea el diagnóstico diferencial con otras enfermedades como la sarcoidosis y la enfermedad de Fabry, cuyo diagnóstico diferencial es de gran importancia por su repercusión terapéutica.
IgG4-related disease is characterised by swollen mass lesions, a dense lymphoplasmacytic infiltrate with immunohistochemical positivity for IgG4, storiform fibrosis and, frequently, but not always, elevated serum IgG4 levels.1 It can be multisystemic, but myocardial involvement, which is determined by imaging tests, has not been described in the medical literature to date.
Clinical ObservationA 48-year-old man, with no toxic habits and no background of interest was admitted to hospital with headaches, paresthesias in the upper right extremity and a hypertensive crisis. Brain CT showed no changes. Vasodilator, diuretic and anti-platelet treatment was initiated with good control over blood pressure rates and the disappearance of neurological focality. The chest X-ray revealed vascular redistribution and an enlarged right hilum. Chest and abdominal CT scan showed multiple lymph nodes of appreciable size, between 10 and 20mm at intrathoracic level (in the prevascular, subcarinal, right petratracheal, bilateral hilar spaces and those adjacent to the lower left bronchus), with no changes to the pulmonary parenchyma nor at abdomen level. A bronchoscopy was performed, which revealed no alterations, and 3 lymph node PAAF with abundant lymphoid cellularity with no atypical findings. The sputum smears and microbacteria cultures tested negative. A transthoracic echocardiogram showed: left ventricle with moderate dilation of its cavity, slight concentric hypertrophy and moderate reduction of overall globe contractability from inferior akinesia and hypokinesia in the remaining segments. Estimated EF of 37%. A restrictive type of diastolic dysfunction suggestive of an increase in capillary pressure. Moderate dilation of the left atrium. The cardiac magnetic resonance (CMR) showed:
- 1.
Situs solitus, levocardia, left apex, AV-VA normal concordance.
- 2.
Left ventricle with moderate concentric, dilated and remodelled hypertrophy, with diffuse hypokinesia and moderately depressed systolic function (EF 44%).
- 3.
Moderately dilated left auricle with septal aneurysm.
- 4.
Right cavities not dilated with normal systolic function.
- 5.
Pericardium not enlarged and with no effusion.
- 6.
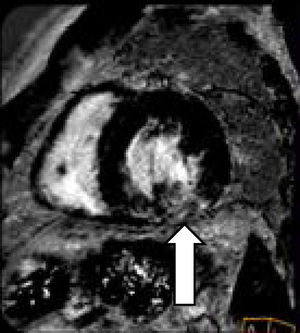
Intramyocardial-idio basal inferolateral and lower basal and lateral patchy pattern of the left ventricle with no necrosis, suggestive of sarcoidosis as opposed to Fabry disease (Fig. 1).
A dried blood spot was studied which ruled out Fabry disease and new lymph node PAAF was performed by echobronchial ultrasound which showed blood material and lymphocytes with no atypical factors or granulomas. The sputum samples and microbacteria culture tested negative. A coronarography did not show any significant angiographic lesion. A gallum scan showed uptake in the upper anterior right and left mediastinal region, which suggested an inflammatory origin, but a lymphoproliferative process was not ruled out. General analysis which included the determination of total immunoglobulins, angio-tensin converting enzyme, autoantibodies and viral serologies all tested negative or normal.
The patient continued with vasodilator treatment and in the medical check-up after 2 months was found to have normal blood pressure and was asymptomatic. A further transthoracic echocardiogram showed no changes to the previous one, except an improvement of systolic function. The transesophageal echocardiogram confirmed the data and permeable oval foramen was ruled out. The CMR was repeated which showed: left ventricle with moderate concentric hypertrophy, no dilation, no change in segmentary contractility and normal systolic function (EF 70%) and persistence of the patchy intramyocardial pattern in the mid interferolateral segment and lower segment of the left ventricle with no necrosis, suggestive of sarcoidosis as opposed to Fabry disease.
Further thoracic CT and gallum scans continued showing mediastinal and hilar lymph node enlargement in the retro sterna prevasular space, with gallum uptake suggestive of inflammatory activity. Due to the suspected diagnosis of an inflammatory process with mediastinal and hilar lymph node involvement and patchy myocardial involvement suggestive of sarcoidosis we decided to perform a diagnostic mediastinoscopy which showed a hard, highly attached tissue in the retrosternal region, which was resected for AP study and biopsy of mediastinal lymph nodes. The AP of the mediastinal lymph nodes. Showed: lymph nodes with sinusal histiocytosis and an increase in eosinophils. The AP of the anterior mediastinal lesion showed: a fibroinflammatory lesion made up of abundant storiform sclerosis surrounding lymphoid follicles with hyperplasia germinal centres, together with abundant plasmocytary infiltrate. Several of the follicles presented with Castlemanoid type appearance with plasmatic cells which surrounded the germinal centre concentrically and with the presence of a thick-wall blood vessel crossing over the germinal centre. An inflammatory infiltrate was also observed with lymphocytes, histiocytes and eosinophils. Small blood vessels were identified with sclerosed wall and no light, associated with inflammatory infiltrate. The histochemical study with elastic fibres showed the presence of sclerosed venous vessels. The immunohistochemical study expressed positivity for IgG and for IgG4 in over 40 plasmatic cells, with an IgG4/IgG ratio of approximately 40%. CD30, CD15, Pax5, EMA, ALK, CD10 and CyclinD1 tested negative. The stains for CD20, CD79a, CD3, CD5 and BCL-2 also revealed B and T lymphocytes. CD23 showed the dentritic cells of the germinal centres. The stains for CK AE1/AE3, CK5/6 y CK34Be12 showed epithelial cell nests trapped within the fibrosis. Calretinin and mesothelin tested negative. The in situ hybridisation study for immunoglobin heavy chains Kappa and Lambda showed polyclonal population of plasma cells. The Epstein–Barr virus tested negative with the EBER in situ hybridisation.
Morphological and immunophenotypic findings were compatible with fibroinflammatory mediastinal lesion related to IgG4. Serum IgG4 was 130mg/dl. Sputum smears and cell cultures for microbacteria from the samples tested negative, and the presence of a lymphoproliferative process was completely ruled out. With the diagnosis of the disease related to IgG4 with mediastinal involvement and probably cardiac involvement, treatment with the immunosuppressant prednisone was initiated (1mg/kg/day) and also azathioprine (dose increases up to 2mg/kg/day). The patient presented with a good clinical response, with reduction of the images of lymph nodes detected by CT and the control CMR performed after 4 months of immunosuppressant treatment showed a reduction in the previously described intramyocardial pattern in the mid inferolateral and lower segments of the left ventricle with no necrosis (Fig. 2).
DiscussionIgG4-related disease, which was described in 2003, has been reported as affecting multiple organs or tissues, such as the biliary tree, salivary glands, periorbitarian tissue, kidneys, lungs, lymph nodes, meninges, aorta, breast, prostate gland, thyroid glands, pericardium and skin.1,2 However, we did not find any myocardial involvement mentioned in the medical literature. Our patient presented which what appeared to be an extensive involvement of intrathoracic lymph nodes, where surgical findings demonstrated fibrosing mediastinitis, described in IgG4-related disease and as was demonstrated by the 2 CMR performed, one myocardial involvement suggested sarcoidosis or Fabry disease but the latter was ruled out by an enzymatic study. Sarcoidosis is a granulomatous disease of immunoinflammatory ethiopathogenesis which is similar in its presentation to IgG4-related disease, and differential diagnosis is therefore often required.3,4 Myocardial involvement of sarcoidosis has been broadly reported and may be detected through imaging studies such CMR or PET-CT with glucose 18.5,6 Although patchy changes are not described in IgG4-related disease, cardiac involvement has been described in the form of coronary periarteritis, luminal stenosis, pericarditis or aortitis.7 In our case, both lymph node involvement and the data from CMR was suggestive of a diagnosis of sarcoidosis. However, the AP showed IgG4-related disease with extensive mediastinal involvement and patchy myocardial involvement, both of which improved with immunosuppressant treatment. Ours is the first description of myocardial involvement within the context of IgG4-related disease.8 We therefore believe that this entity should be considered in the differential diagnosis of those entities which may lead to patchy intramyocardial involvement, such as sarcoidosis or Fabry disease.
Conflict of InterestsThe authors have no conflict of interests to declare.
Please cite this article as: López Vivancos J, Sanchez Sitges L, Herranz Perez X, Leal Bohorquez N, Simonetti S, García Cors M. Enfermedad relacionada con inmunoglobulina IgG4 con posible afectación miocárdica. Reumatol Clin. 2019;15:e116–e118.