Chikungunya virus infection (CHIKV) is associated with joint involvement in half of the cases. This can lead to erosive arthritis which, given the high intervariability of clinical and serological presentations, and the probable role of genetic conditioning in the severity and chronification of the condition, represents a great diagnostic and therapeutic challenge. There is an important lack of scientific evidence that would enable us to characterize the variability of the patient and choose the most appropriate approach.
La infección por virus Chikungunya (CHIKV) presenta afectación articular en la mitad de las ocasiones. Esta afectación puede derivar en una artritis erosiva que, dada la elevada intervariabilidad en la presentación tanto clínica como serológica y el probable papel del condicionamiento genético en la gravedad y cronificación del cuadro, supone un gran reto diagnóstico y terapéutico. Existe una importante falta de evidencia científica que nos permita caracterizar la variabilidad del paciente y decidir el abordaje más adecuado.
Alphaviruses are associated with inflammatory forms of clinically severe arthritis which may be self-limiting or persist over time, mimicking persistent forms of noninfectious arthritis.
The Chikungunya (CHIK) virus is an arbovirus of the Togaviridae family of the alphavirus species, as are also the O’nyong-nyong virus, the Sindbis virus, the Ross river virus, the Mayaro virus, the Semliki virus and the Barmah virus. Discovered in Tanzania in 1952, the CHIK has widely extended, causing massive explosive outbreaks in the region of the Indian Ocean islands. It was traditionally perceived as a tropical disease until an outbreak occurred in Italy in 2007. Vector distribution is extensive (Aedes aegypti and Aedes albopictus) and since the end of 2013 infections by CHIK have spread from the Southern states of the United States to the north of Argentina. These are the same mosquitoes responsible for the transmission of dengue fever, yellow fever, Zika fever, West Nile fever, Japanese encephalitis and Eastern equine encephalitis virus.
The standard initial disease symptoms are high fever from 3 to 10 days, with half of patients also suffering from joint pain and/or effusion1 which starts 2–5 days after the fever and usually includes the involvement of over 10 joints symmetrically, with hands, followed by wrists, and ankles being the most commonly affected.2,3 Participation of the axial skeleton is observed in less than half of the patients depending on the series. The anti-CCP antibodies and the rheumatoid factor (RF) typically test negative.
Due to its low prevalence in Europe and North America up until now this disease has not been a regular pathology in the everyday clinical practice of rheumatologists in these areas. However, the increase in its incidence in our environment due to greater international travel and global warming suggests that cases should now be reviewed in greater detail.
Clinical CaseA 40 year-old woman presented at our centre in mid-December 2014. She had been on a trip to Cartagena de Indias at the beginning of December that same year. On the third day after her arrival in Colombia she suffered from low mucosa secretion and gingivitis, and right carpal monoarthralgia on the fifth day which one day later developed into symmetrical and distal bilateral polyarthralgias affecting both wrists and ankles. Later proximal and distal interphalangeal arthalgias were added to the first and fourth finger. She did not suffer from myalgias. On the eighth day, on her return to Spain she had a fever of 37.1°C with a nonconfluent maculopapular rash which respected palms of hands and feet. Analysis highlighted a reactive C protein of 1.9mg/dl, lymphopenia and monocytosis. Treatment with nonsteroid anti-inflammatory drugs (NSAIDS) and paracetamol were prescribed. On the twelfth day she presented with synovitis and effusion in both wrists and ankles which were confirmed by the rheumatology department. The patient stated she no longer had a fever but did have night diaphoresis. On the eighteenth day the patient suffered from carpal tunnel syndrome, mostly in her right hand. A positive IgM antibody for CHIK was then confirmed serologically and treatment with 30mg of prednisone was initiated.
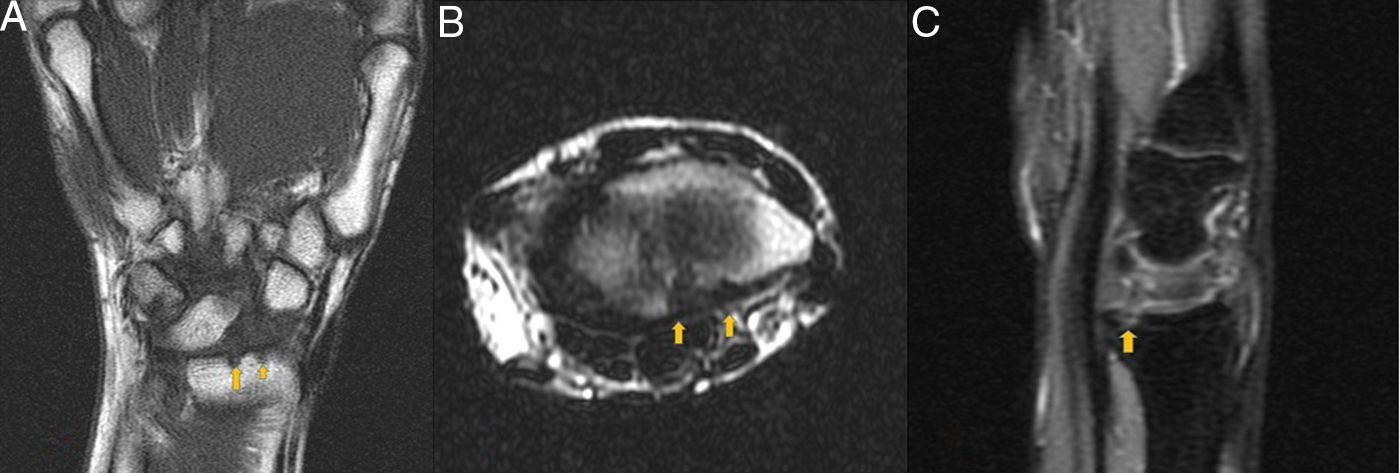
In May 2015, functional limitation persisted, with no synovitis, but with serious pain in right wrists. Nuclear magnetic resonance (NMR) imaging of the right wrist in October 2015, 11 months after initiation of symptoms, showed two erosions on the articular side of the right radial epiphysis (Fig. 1). In our case, the patient continued to suffer for 18 months with arthritis controlled with corticosteroids, initially at a fixed dose and later with a progressively lower dose until it was resolved. Due to the patient's express desire to conceive, we ruled out initiation of standard synthetic disease-modifying anti-rheumatic drugs (DMARDs). After one and a half years of clinical symptoms with the presence of articular effusion, the corticoid treatment was withdrawn. The patient currently has no clinical or ultrasound signs of arthritis in any joint although she continues to have pain on extreme flexion of the right wrist.
DiscussionThe possibility of erosive polyarthritis of wrists, hands and ankles has been described in the literature,1,4,5 with participation from uncommon joints on occasions, such as the sternoclavicular or temporomandibular joints. The severity of symptoms in the initial stages of the infection by CHIK could determine time of resolution and risk of development of a long-term arthritis.1 Chronic progression of arthritis should be taken into consideration for a differential diagnosis to prevent persistence over time of an arthritis which could result in joint destruction.6
The mechanisms that may lead to chronification of arthritis have not been well established. At the moment, the presence of CHIK RNA in synovial fluid in the acute phase has only been demonstrated in animal models. Furthermore it has been demonstrated that macrophage activation in synovial fluid plays a central role in persistent joint inflammation. A study sponsored by the George Washington University is currently trying to show the presence of the virus in human synovial fluid and to assess its role in arthritis chronification, in addition to the presence or nonpresence of the virus in serum.7 The prolonged persistence of IgM in serum could indicate the presence of the virus in tissues. However, there is no evidence that the persistence of the virus would be necessary for the development of a chronic inflammation or that there is a clear relationship between with the severity of the illness.
One hypothesis is that, through the mechanisms of molecular mimicry and individual genetic conditioning, the infection triggers off an autoimmune reaction which conditions the appearance of a chronic arthritis. Indian scientists concluded significantly in 2014 that the frequency of the allele HLA-DRB1*11 and the haplotype DRB1*11/DQB1*03 was lower in patients than in controls, conferring resistance. They also proved that the haplotype DRB1*04/DQB1*03 was significantly higher in patients with arthritis chronification, and found the allele HLA DQB1*04 solely in this patient group. In 2010, the same work group, from the longitudinal follow-up of a cohort of 203 patients for 10 months, confirmed that only 51% of patients were cured at the end of nine months. They observed that of those who had joint pain (74%), 36% met the American College of Rheumatology criteria to classify them as having rheumatoid arthritis and tested 20 of these for RF and anti-CCP. All serologies were negative except for one patient who tested positive for anti-CCP positive and who showed signs of joint destruction by NMR.1,8
If we review data from the 2006 outbreak on Reunion Island, we see that the majority of young patients recovered, with prevalence of persistence clearly higher in people over 60, who also had a higher viral load. Rapid establishment of an innate response was shown with an increase in the activation of NK cells and CD4 lymphocytes, followed by a weak response of the cytokins Th1/Th2, and high levels of IFN-alpha.9
Cases have been described in the literature where chronic arthritis follows an infection by CHIK. Some of these patients despite post-infectious origin, were treated with DMARDs due to the chronic nature of the condition, with favourable outcome. We should highlight that the efficacy of the DMARDs in this indication has not been accurately assessed. French researchers have postulated that the resistance or dependence of corticoids beyond 3 months would be highly suggestive of chronification.10
At present, treatment is essentially one of support, including anti-inflammatory drugs. Antiviral drugs and chloroquine have not proven to be effective and there is currently no available vaccine. For selected chronic patients, the corticosteroids methotrexate and other immunomodulatory agents may be of use.10,11
ConclusionScientific production aimed at this issue is limited and the evidence in all aspects is scarce. Although arthritis by CHIK are self-limiting and mild in somewhat more than half of the occasions, in several of the series up to 49% of patients chronic progression took over 9 months, sometimes causing joint destructions.1 It is unknown whether early establishment of treatment would lead to reduction of the probability of suffering from erosions. Diagnosis is serological. IgM presents from day one to day twelve of symptom initiation and IgG from the second month onwards although it is possible that raised levels will last for years. It should be noted that possible laboratory cross-reactivity exists or a co-infection may occur since the vector is shared with the dengue. Serological and clinical evolution is highly variable and genetic conditioning may play an essential role in the etiopathogenesis of chronification. The infection generates antibodies which protect the person throughout their life.
FundingNo financing sources exist, all the information was obtained during standard clinical practice.
Conflict of InterestsAll the authors have no conflicts of interest to declare.
We would like to thank all our colleagues at the Rheumatology Service and the Musculoskeletal Radiology Department for their support and for making everything increasingly easy for us.
Please cite this article as: Castro-Domínguez F, Salman-Monte TC, Ojeda F, Corzo P, Carrión-Barberá I, Garcia-Duitama IC, et al. Artritis erosiva por virus Chikungunya, caso y revisión de la literatura. Reumatol Clin. 2019;15:e119–e121.