Hip pain is a frequent cause of medical attention in the daily clinical practice. Among the different causes included in the differential diagnosis we find ischiofemoral impingement, described initially in patients after joint replacement surgery, but later found in patients with no history of a causal disease.
El dolor de cadera es una causa frecuente de consulta médica en la clínica diaria. Entre las diferentes causas que entran en el diagnóstico diferencial está el síndrome de pinzamiento isquiofemoral, que se describió inicialmente en pacientes tras cirugía de recambio articular, pero que a posteriori se ha descrito en pacientes sin antecedente de patología causal.
Hip pain is a common cause of medical attention and diagnosis is difficult because the etiology is diverse.
One of them, little known, is ischiofemoral impingement syndrome, first described in women after joint replacement surgery1 but subsequently described in patients with no history of disease.2,3
Case ReportWe report the case of a 16-year-old casual athlete, with no known allergies or medical-surgical history of interest, consulting for hip pain over a year in development, located in the anterolateral aspect of the right hip and radiating to the anterior aspect of the knee, intervening with physical activity. The pain increased over time to preclude sports activity, except for short periods.
On physical examination the patient showed good general condition, without atrophy or deformities, and preserved mobility of the 4 limbs. There was snapping and production of pain with adduction, external rotation and extension.
Plain radiography of the lumbar spine and hips showed no abnormalities. Lab tests, including complete blood count, kidney and liver function, calcium, phosphorus, alkaline phosphatase, CPK, thyroid hormones, and autoimmunity tests, as well as acute phase reactants, were within normal parameters.
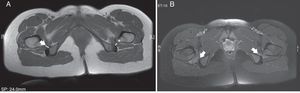
Given the clinical persistence we requested an MRI of the hip, which displayed a reduced space between the lesser trochanter and the ischial tuberosity bilaterally, with increased compression and T2 signal in both femoral muscles translating intramuscular edema. The distance ischiofemoral space measurement obtained was 9mm bilaterally and 5mm wide on the right femoral space and 6mm on the left (Fig. 1A and B). No FAI data was obtained.
Based on these findings, a diagnosis of ischiofemoral impingement syndrome was made and treated with NSAIDs, analgesics and rest, with progressive reintroduction of sports activities, showing marked improvement.
DiscussionThe pelvic bone anatomy provides two possible points of impingement. Impingement is a condition known and widely described, but the space between the lesser trochanter and the ischium is usually not considered, since it is wider between these structures.
Ischiofemoral impingement syndrome was first described in patients with persistent hip pain after hip1 replacement. The distance between the ischium and the lesser trochanter was reduced after surgery in these patients, while others, such as those with intertrochanteric fracture, pelvic corrective valgus osteotomy or hip degenerative arthritis, superomedial migration of the femur, subsequently impinged.
The concept of ischiofemoral impingement in patients without previous injury was recently described.3,4
The prevalence is unknown, since we have only small series of cases. Affected patients are typically women, suggesting a potential link between the female pelvic anatomical arrangement, with prominent and separated ischial tuberosities.5
It develops clinically from months to years, with pain anteriorly and medial to the hip, sometimes radiating to the lower extremity. Involvement is bilateral in one quarter of patients.
In those patients in whom there is clinical suspicion, plain light hip adduction, external rotation (unlike the study performed conventionally) and extension could potentially be helpful in some cases, with a normal value of the ischiofemoral space being 2cm.3
Diagnosis, however, is established through magnetic resonance. Characteristic findings are a decreased ischiofemoral space compared to healthy controls (ischiofemoral space of 23±8mm and femoral space of 12±4mm)6 and altered signals from the femoral muscle, which results in edema of the myotendinous junction or intramuscular rupture. If involvement is prolonged the clinical course is chronic, there may be muscle atrophy and muscle bundle replacement by fibrofatty tissue. Sometimes it can affect the insertion of the hamstrings and, to a lesser extent, the ilio-psoas, which was not observed in our case.
The differential diagnosis is made with those conditions involving groin pain, and by discarding tendinitis, bursitis, osteitis or siphysitis, among others.7
There is no optimal treatment with rest, use of analgesics and anti-inflammatory drugs or local injections having been used irregularly8 but successfully. Surgical treatment offers a definitive clinical relief by resection of the lesser trochanter.
Ethical disclosuresProtection of human and animal subjects. The authors declare that no experiments were performed on humans or animals for this investigation.
Confidentiality of Data. The authors declare that they have followed the protocols of their work centre on the publication of patient data and that all the patients included in the study have received sufficient information and have given their informed consent in writing to participate in that study.
Right to privacy and informed consent. The authors have obtained the informed consent of the patients and /or subjects mentioned in the article. The author for correspondence is in possession of this document.
DisclosuresThe authors have no disclosures to make.
Please, cite this article as: López-Sánchez MC, et al. Pinzamiento isquiofemoral: dolor de cadera de causa poco frecuente. Reumatol Clin. 2012. http://dx.doi.org/10.1016/j.reuma.2012.06.005