Male aged 74, with a background of de novo prostate cancer was referred for staging and treatment assessment. The patient was asymptomatic and denied suffering from any previous trauma or infections.
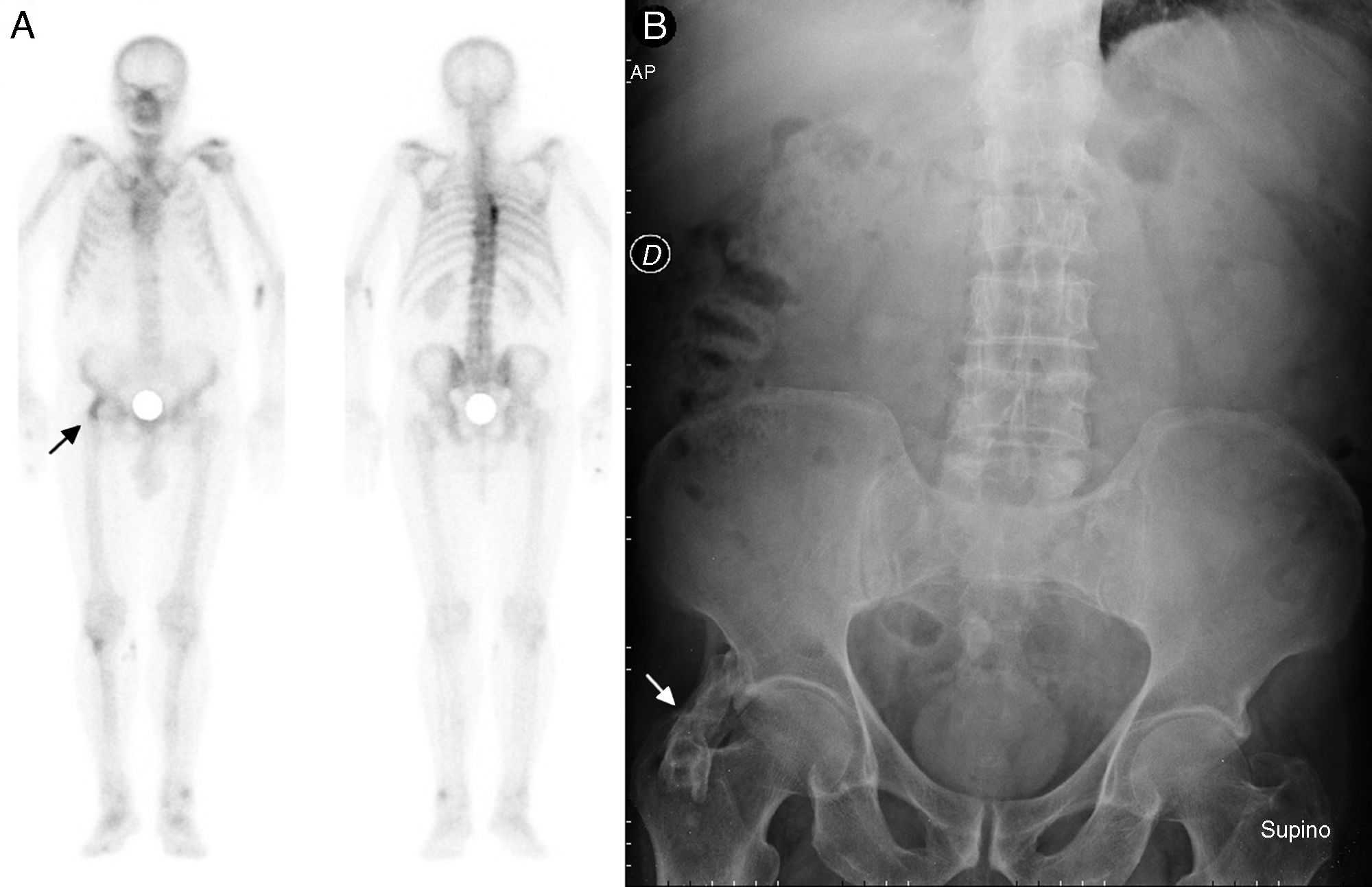
A complete whole body bone scan was performed with 99mTc-HDP in anterior and posterior projections (Fig. 1A) where an increase in uptake of the tracer of slight to moderate intensity was observed, together with lineal morphology in the projection region of the right anterior inferior iliac spine, of doubtful pathological significance (arrow).
Retrospectively reviewing the medical background and additional tests, in the plain X-ray of the abdomen in supine position (Fig. 1B) the presence of a radiodense image was observed, with well-defined edges and radiolucent areas on the inside, which appeared to depend on the iliac bone (arrow).
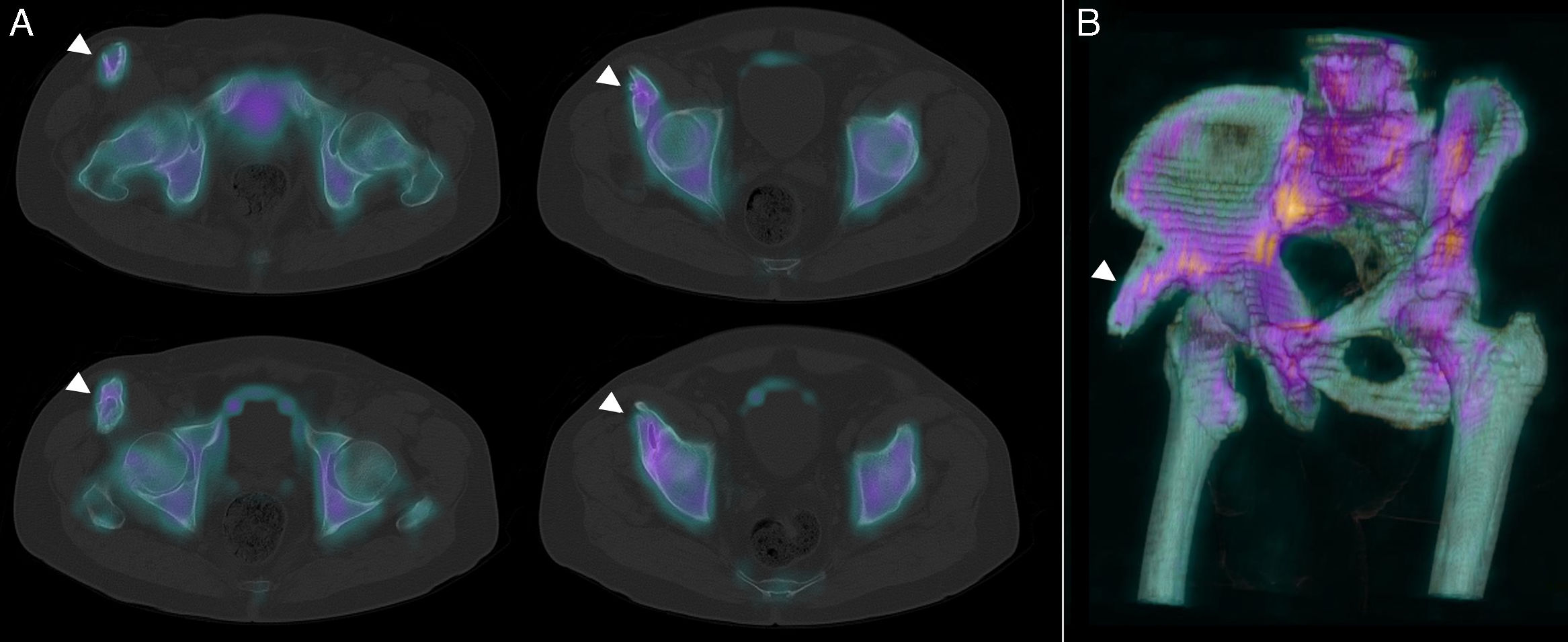
For further determination of the finding, SPECT/CT with 3D reconstruction was performed (Fig. 2A and B, respectively), confirming correlation with a bony outgrowth (arrow heads) of approximately 2.35×1.47cm towards superficial planes, anteriorly displacing the muscular belly of the sartorius which in the image morphology is continuous with the bone cortex and bone marrow tissue, and is suggestive of osteochondroma.
Osteochondroma or cartilage-capped bone spur, is the most commonly worldwide benign bone tumour,1 accounting for 20%–50% of benign tumours and between 10%–20% of all primary bone tumours, with a prevalence of approximately 3%.2
It is a proliferation of bone composed of the marrow and cortex capped by cartilage, an area of growth, which usually diminishes after skeletal maturity. Predilection is for long bone mataphysis, although they have been described throughout the skeleton.3 They have a certain potential for malignancy, evolving into chondrosarcoma in 0.5%–5% of cases.2,3 They may be single or multiple4 and appear spontaneously or after an injury.5
To sum up, when there is an incidental finding of a bony outgrowth with continuity of the cortical bone, cartilage-capped, osteoblastic activity similar to that of the adjacent bone tissue and without other morphofunctional malignancy criteria, the diagnosis of osteochondroma must be suggested as a first line option.
Conflict of interestsThe authors have no conflict of interests to declare.
Please cite this article as: Moreno-Ballesteros A, Calvo-Morón MC, García-Gómez FJ, Castro-Montaño J. Hallazgo incidental de osteocondroma pélvico. Reumatol Clín. 2020;16:183–184.