Psoriasis is a common inflammatory dermatosis that may be associated with a number of diseases. Recent studies provide evidence that there is a greater frequency of autoimmune diseases, but association with autoimmune connective tissue diseases is uncommon. The coexistence of psoriasis and lupus erythematosus is rare. Besides, the occurrence of morphea has rarely been reported in patients with lupus or psoriasis. We report a woman with cutaneous lupus and morphea profunda associated with psoriasis, with an excellent response to methotrexate, and review the literature.
La psoriasis es una frecuente dermatosis inflamatoria que puede asociarse a diversas enfermedades. Estudios recientes señalan que la presencia de enfermedades autoinmunes es mayor, pero es rara la asociación con enfermedades del tejido conectivo. La coexistencia con lupus es infrecuente. Por otra parte, la morfea raramente se ha reportado en pacientes con lupus o psoriasis. Presentamos a una paciente con lupus cutáneo y morfea profunda que posteriormente desarrolló psoriasis, con excelente respuesta a metotrexato y revisamos la literatura.
Psoriasis is a dermatosis frequently associated with different comorbidities but its coexistence with connective tissue autoimmune diseases (CTAID) is rare.1 Of these, the most common is systemic lupus erythematosus (SLE) which is much rarer when associated with morphea profunda. We present the case of a patient with cutaneous lupus erythematosus and morphea profunda, with subsequent psoriasis.
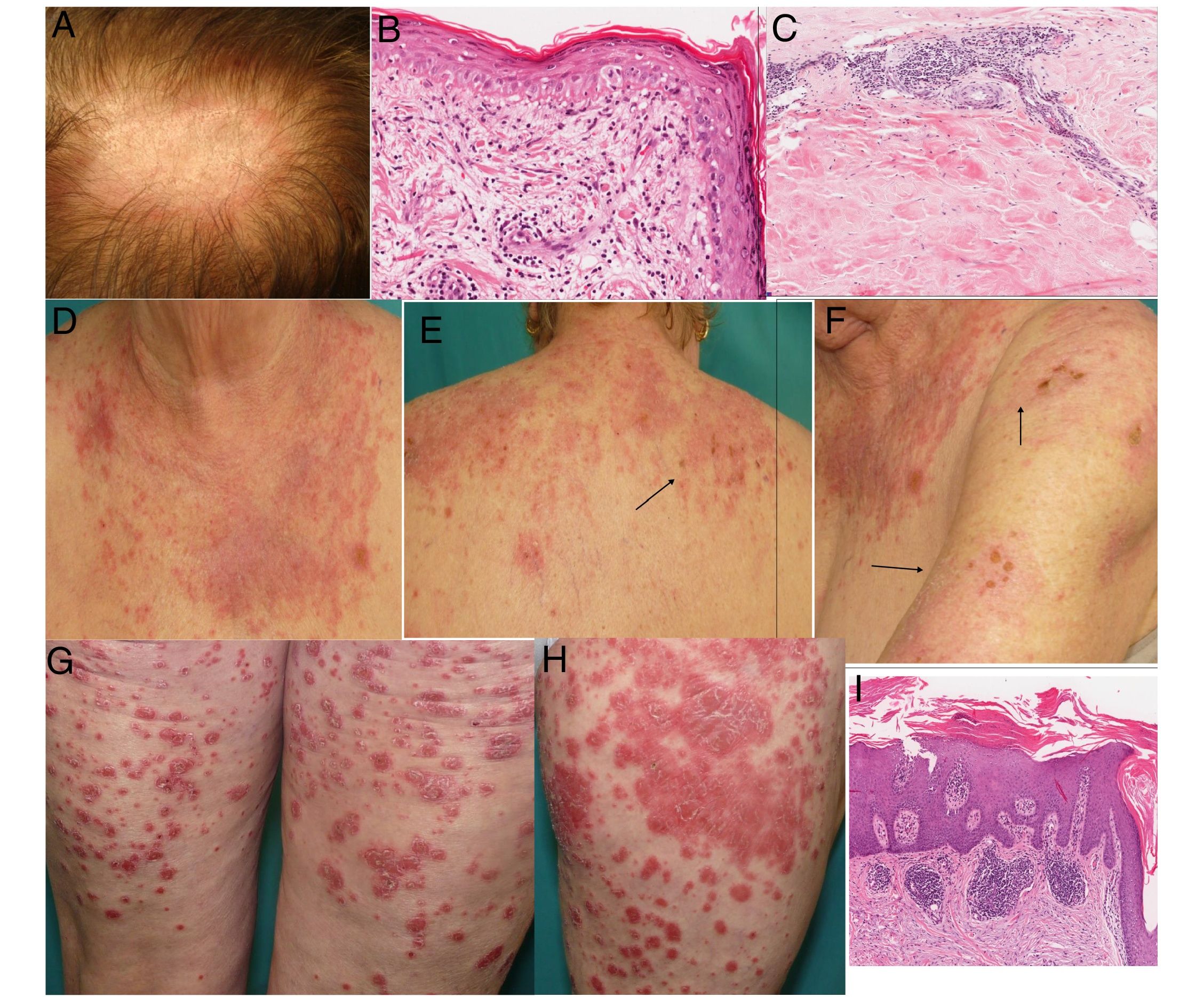
Clinical caseA woman aged 67, with a background of metabolic syndrome and ischaemic cardiopathy. She referred to her niece who had presented with lupus but denied any family history of psoriasis. In 2005 she attended consultation for an alopecic plaque on her scalp, with clinical and histopathological features compatible with discoid lupus erythematosus (Fig. 1A and B). The autoimmunity study tested normal with topical corticoids providing improvement of her condition. Two years later, she presented with profound, painful skin induration involving both hips and buttocks, with no visible superficial lesions. Biopsy was compatible with morphea profunda, and systemic lupus erythematosus (Fig. 1C) was ruled out. In 2009, she began to suffer outbreaks of erythematodermatous plaques and erosions in areas exposed to sunlight on face, upper trunk and shoulders, compatible with subacute lupus (SACLR) (Fig. 1D–F) which was confirmed with biopsy. Again, analysis with autoimmunity tested normal. Several cycles of prednisone (.5mg/kg/day) were required and temporary improvement ensued. After 6 months, overlapping with an outbreak of SACLR, new lesions appeared in the form of generalised erythematodermatous plaques, and psoriasis was histologically confirmed (Fig. 1 G–H). Weekly treatment with 7.5–15mg of methotrexate, topical corticoids and protection against sunlight was initiated, which has been continued up until now, with the lupus and mophea being resolved and only isolated plaque psoriasis presenting.
(A) Alopecic erythematosus plaque in scalp with flaking. (B) Biopsy of the scalp plaque: orthokeratotic hyperkeratosis, thickening of the basement membrane, vacuolar degeneration and apoptotic keratinocytes (haematoxylin–eosin 400×). (C) Biopst of the lumbar skin induration showing marked thickening of the septum, hyalinisation of collagen bundles and perivascular lymphoplasmocytic infiltration compatible with morphea. Absence of lobulillar panniculitis, hyaline fat necrosis, calcification focal points and lymphoid follicles ruling out lupus panniculitis (haematoxylin–eosin 200×). (D–F) Erythematodematosus plaques in areas exposed to sunlight with erosive and necrotic areas (arrows): SACLE. (G and H) Erythematosus plaques in thighs: plaque psoriasis. (I) Biopsy of a plaque: hyperkeratosis, parakeratosis, Munro's microabcesses, suprapapillary thinning and lengthening of dermal capillaries, typical of psoriasis (haematoxylin–eosin 200×).
Psoriasis is a chronic immune mediated inflammatory dermatosis. Several studies show that the incidence of AID is more common than in the general population, essentially if psoriasic arthritis (PA) exists.2,3 The coexistence of psoriasis and lupus is rare,4–8 in series and isolated cases (generally SLE), with its true incidence rate unknown. In one series of 9420 patients with psoriasis it was noted that .69% had associated lupus and this affected 1.1% of those with SLE.5 In a multicentre study of patients with psoriasis and lupus, 96 cases were found in 23 years, representing .015% and .017% of patients diagnosed with both disorders, and .95 and 3.43% of those diagnosed with psoriasis and lupus in one year, respectively.7 When they coexist there is no chronological predominance of either over the other,4,6,7 and the majority of patients are Caucasian women. They mostly present with plaque psoriasis involving the limbs, but palms and soles may also be involved, erythoderma6 and up to a third may have pustular psoriasis.7 Almost half have associated PA (more common than psoriasis without lupus), with a minority having lupus with PA, with no psoriasis.6 With respect to lupus, the most common is SLE following on from discoid and to a lesser extent from drugs and SACLE.6,7 Sensitivity to sunlight which was highlighted in our case, is more common than in lupus with no psoriasis.4,7 In general, both conditions are distinguishable, but may be confused in acute forms, if lupus occurs with papuloscamous eruption or erythoderma in cases of LES, SACLE and from drugs, with clinical and histological overlap.4 Almost 2 thirds may involve other AID, and monitoring is recommended.7 Regarding the pathogeny, recent evidence has indicated that both share over regulation of the Th17 pathway with raising of IL-17, IL-22 and IL-23,7 and although most studies are for SLE, it has also been demonstrated that in skin lupus the IL-17 increases, as it does in psoriasis. With regard to the association of morphea and psoriasis, incidence is unknown and scarcely twenty cases have been reported in the literature.9 However, it remains one of the AID most commonly associated with morphea, up to 2%,10 and generally affects adults with widespread morphea. Both conditions may have a common immunological base, since although morphea has been related to the Th2 pathway, those of LTh1 and LTh17 would also be essentially involved in initial stages.9 Moreover, although up to 12% of patients with systemic sclerosis have features of SLE, association with morphea is extremely rare. In general, they are plaque or lineal morphea associated to any variant of lupus, mainly discoid lupus. Patients are usually young and middle-aged women.11 A few isolated cases of clinical and histological overlap of cutaneous lupus and morphea in the same site have been reported, occasionally lineal (sclerodermiform erythematosus).12,13
In these patients, treatment is a challenge: phototherapy used in psoriasis may trigger or aggravate the lupus, whilst the drugs used – antimalarial drugs, systemic corticoids and rituximab, may provoke or worsen a case of psoriasis. Methotrexate would be first line treatment.6,7 Controversy surrounds the use of anti-tumour necrosis factor alpha but a background of lupus would possibly not be contraindicated.6 The involvement of the Th-17/IL-17/IL-23 axis in lupus and psoriasis supports the use of ustekinumab, with cases of favourable response having been described,14 whilst no experience of anti-IL-17 exists. Abatacept could be another therapeutic option. For morphea, methotrexate, systemic corticoids and UV light therapy is recommended.
ConclusionWe present the case of a patient with CLE, morphea profunda and psoriasis, a condition which has not been reported in the literature in the last 50 years. Further studies are needed to examine the real frequency of psoriasis and CLE and specifically, cutaneous lupus and morphea. The Th17 pathway could be the pathogenic nexus, with possible therapeutic involvement.
Conflict of interestsThe authors have no conflict of interests to declare.
Please cite this article as: García-Arpa M, Flores-Terry MA, Ramos-Rodríguez C, Franco-Muñoz M, González-Ruiz L, Ramírez-Huaranga MA. Lupus eritematoso cutáneo, morfea profunda y psoriasis en una paciente. Reumatol Clin. 2020;16:180–182.