To describe the percentage of prescription of pharmacologic supplements in patients starting antiresorptive treatment (ART) for osteoporosis by specialists.
DesignCross-sectional, naturalistic, multicenter study with retrospective data collection.
Patients and methods88 Spanish primary care (PC) physicians participated as well as those from Bone Metabolism Unit/Rheumatology and Gynecology units. Patients were females with osteoporosis who started ART in the 12–36 months prior to the visit.
Main outcomesGeneral clinical variables and those related to osteoporosis treatment (both ART and pharmacologic supplements) and an opinion survey on pharmacologic supplements.
Results480 patients were included. Mean age (SD) was 65.8 (9.2) years. Pharmacologic supplements were prescribed in 69.6% of patients and were more frequent in patients treated in Bone Metabolism/Rheumatology Units (89.1%) than patients treated by PC (60.3%) and Gynecology (55.6%). In the physician survey, 72% of the Bone Metabolism/Rheumatology Unit physicians responded that the Vitamin D supplements were necessary for treatment of osteoporosis vs 38.5% of PC physicians (P=.058).
ConclusionsThe use of pharmacologic supplements in the onset of treatment with ART represents more than 60% of the sample, although differences were seen between specialists, with a greater percentage of patients with supplements in the Bone Metabolism/Rheumatology Units than that in PC and Gynecology, despite guidelines primarily recommend the use of pharmacologic supplements in these patients.
Describir el porcentaje de prescripción de suplementos farmacológicos en pacientes que inician pauta de tratamiento con antirresortivos (TAR) en pacientes con osteoporosis y por especialidades médicas.
DiseñoEstudio transversal, con recogida de información retrospectiva, naturalístico y multicéntrico.
EmplazamientoParticiparon 88 médicos españoles de atención primaria (AP), unidades de metabolismo óseo y mineral (UMO)/reumatología y ginecología.
ParticipantesMujeres con osteoporosis que inician tratamiento TAR en los 12-36 meses previos a la visita.
Mediciones principalesVariables clínicas generales y relativas al tratamiento de la osteoporosis (TAR, suplementos farmacológicos) y encuesta de opinión sobre suplementos farmacológicos.
ResultadosSe incluyó a 480 pacientes. La edad media ± DE era de 65,8 ± 9,2 años. Se prescribieron suplementos farmacológicos en el 69,6% de las pacientes, siendo más frecuente en aquellas pacientes tratadas en consultas de UMO/reumatología (89,1%) que en las pacientes tratadas en AP (60,3%) y en ginecología (55,6%). En la encuesta realizada a los médicos el 72% de los médicos de UMO/reumatología y el 66,7% de ginecólogos respondieron que los suplementos de vitamina D son necesarios en el tratamiento habitual de la osteoporosis frente al 38,5% de los médicos de AP (p=0,058).
ConclusionesEl uso de suplementos farmacológicos en la pauta inicial de tratamiento con TAR representa más del 60% de la muestra, aunque se detectan diferencias según tipo de especialista, con un mayor porcentaje de pacientes con suplementos en las consultas de UMO/Reumatología que en AP y ginecología, pese a que las guías recomiendan el uso mayoritario de suplementos farmacológicos en estas pacientes.
The SEIOMM (Spanish Society for Bone and Mineral Metabolism Research) defines osteoporosis as a skeletal disease characterized by reduced bone strength that predisposes a person to an increased risk of fracture.1
In Spain, more than 12% of the female population over age 50 has osteoporosis, which translates to about 2 million women with this disease.2
It is estimated that a quarter of women over age 50 met criteria for osteoporosis in a lumbar spine or femur neck densitometry.3 The annual incidence of osteoporotic fractures in Spain is very high and only the hip accounts for more than 60000 cases a year.4
Osteoporosis is thus a major health problem, not only because of the occurrence of fractures associated with the disease but also due to its associated social magnitude and impact. Due to its relationship with the progressive aging of the population, it is expected to rise thereby magnifying the prevalence of its burden on the health system.5–7
The therapeutic approach in osteoporosis has as its main objective the prevention of fractures; the available drugs can be grouped according to their mode of action in three main groups: the anti-resorptive agents (bisphosphonates, selective estrogen receptor modulators or SERMs, and calcitonin), the bone forming agents (PTH analogues) and those with both actions (strontium ranelate).8
It has been shown that an adequate calcium intake (1000–1500mg/day) reduces bone loss in adults,9 while vitamin D is useful for calcium10 intestinal absorption, so calcium and vitamin D are essential in maintaining bone homeostasis.11 It has been shown that vitamin D deficiency is more evident in the elderly12 population.13 Furthermore, a study conducted in 11 European countries found that 47% of the population of elderly women had deficient levels of vitamin D, and this deficiency is more frequent in Mediterranean countries than in northern Europe.14 On the other hand, and although there is evidence of the efficacy of vitamin D in the prevention of osteoporosis,10,15 results are contradictory regarding the decrease in fracture risk with both calcium and vitamin D16–18 intake.
Due to the large number of therapeutic options available and the variety of medical specialties that can diagnose and treat these patients, osteoporosis is one of the diseases with greater clinical variability19 therapeutic practice,20 especially with regard to the necessary measures to supplement the intake of calcium and vitamin D.21 The objective of this paper is to describe the percentage of prescription drug supplements in patients with osteoporosis who initiate therapy with antiresorptive therapies (ART) by type of specialist as well as their views on drug supplements.
Material and MethodsDesignThis article presents data from a subanalysis of a cross-sectional design study with retrospective data collection whose main objective was to assess persistence and adherence in patients with osteoporosis who start ART treatment (bisphosphonate or SERM), associated or not with pharmacological supplements (calcium and/or vitamin D).
88 doctors in Spain belonging to primary care (PC), units of bone and mineral metabolism (BMU), gynecology, and rheumatology participated in the study.
The study required the completion of a single visit in which the researcher collected the variables by reviewing medical records. On the other hand, we asked all physicians participating in the study to complete a survey about drug supplements (calcium and vitamin D).
This study was submitted for evaluation by the clinical research ethics committee of the Fundació Jordi Gol i Gurina (Barcelona).
Study PopulationThe inclusion of patients was conducted between December 2006 and May 2007 with consecutive recruitment of patients who were seen for any reason and met the evaluation criteria. Be included women who had started ART treatment (bisphosphonate or SERM) associated or not with pharmacological supplements of calcium and/or vitamin D, between 12 and 36 months before the study visit (whether to continue receiving these treatments or not the time of study visit), and medical history were available to allow the collection of minimal essential variables of the study (treatment received and dates of visit or prescription). We excluded those patients with secondary osteoporosis, those who were treated with bisphosphonates for malignant disease and those who had started treatment with calcitonin, hormone replacement therapy, strontium ranelate, tibolone, and parathyroid hormone in the same period. All patients included gave their written consent.
Study VariablesWe recorded age, general clinical variables (presence of comorbidities and their treatment), variables related to osteoporosis (history and type of fracture and time since last fracture), and variables related to the treatment for osteoporosis (specialty, prescribing physician's initial treatment, treatment indication and indication criteria, use of pharmacological supplements as well as participating physicians’ responses to the poll cited above). To facilitate the completion of the survey, the response categories were closed to all questions. In quantitative response questions, response options were different ranges of percentages and the researcher had to position the answer. In questions where the answers were not quantitative categories were “strongly agree” and “strongly disagree” with the statement made.
Statistical AnalysisWe conducted a descriptive analysis of the variables recorded for the entire sample and stratified by the specialty of participating physicians, PC, gynecology, and BMU/rheumatology (the data of the patients included by specialists from BMU were analyzed along with data from patients enrolled by rheumatologists because of the low number of centers and patients included by BMU).
We analyzed the number of patients and the number of patterns of onset. Both figures do not match because two patients were prescribed two (a bisphosphonate and SERM) ART schemes. Because of the retrospectively collected data, we made the assumption that one ART was prescribed first and then the other, so we considered two different patterns for these two patients. The results are presented as follows: mean, standard deviation and number of valid cases in the case of continuous variables and case count in each category, and relative frequency of total responses in the case of categorical variables. The comparison of results between specialties was performed using the chi-square in the case of categorical variables and Student's t test or ANOVA for continuous variables.
In all statistical tests performed we used a statistical significance level of 0.05.
For data analysis we used the statistical package SPSS version 15.0 for Windows.
Results88 doctors participated in the study, with 41 (46.6%) of them from PC, 34 (38.6%) specialists BMU/rheumatology and 13 (14.8%) gynecologists. The study included a total of 504 patients, of whom 24 were excluded (4.8%) for not meeting any of the criteria for inclusion, so the final sample analyzed was 480 patients. The final sample distribution by types of specialists included was PC 52.5% (252/480 patients), 13.1% (63/480 patients) included by gynecologists and 34.4% (165/480 patients) included by the BMU/rheumatology.
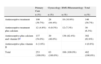
Sociodemographic and Clinical CharacteristicsThe mean age±SD of the patients in the study was 65.8±9.2 years. Patients included by gynecology were on average younger than when included by other specialties (P<.01). 69.2% of total disease suffered concomitant significant difference when observed between specialties, with a lower percentage of patients with concomitant diseases in gynecology (P<.01). A quarter of the sample (24.6%) had a history of fracture (P<.01), the most common being symptomatic vertebral fracture (9.2% of patients). The mean±SD time elapsed between the last fracture reported by the patient and the study visit was 5.6±7.2 years. Table 1 shows the results distributed according to the medical specialty of the investigators.
Sociodemographic and Clinical Characteristics of the Participating Sample in the Study in Relation to Medical Specialty.
| Primary Care n=252 (52.5%) | Gynecology n=63 (13.1%) | BMU/Rheumatology n=165 (34.3%) | Total n=480 (100%) | |
| Age (years),amean ±SD | 66.1±9.3 | 58.7±6.8 | 68.1±8.6 | 65.8±9.2 |
| Presence of concomitant disease,an (%) | 197 (78.2%) | 31 (49.2%) | 104 (63.0%) | 332 (69.2%) |
| History of fracture,an (%) | 62 (24.6%) | 5 (7.9%) | 51 (30.9%) | 118 (24.6%) |
| Type of fracture, n (%) | ||||
| Femoral neck | 5 (2.0%) | 7 (4.2%) | 12 (2.5%) | |
| Symptomatic spinal column | 20 (7.9%) | 3 (4.8%) | 21 (12.7%) | 44 (9.2%) |
| Asymptomatic spinal fracture | 12 (4.8%) | 1 (1.6%) | 10 (6.1%) | 23 (4.8%) |
| Distal forearm | 14 (5.6%) | 2 (3.2%) | 15 (9.1%) | 31 (6.5%) |
| Other | 22 (8.7%) | 12 (7.3%) | 34 (7.1%) | |
| Time since last fracture (years), mean±SD | 4.8±6.5 | 5.1±6.1 | 6.6±8.0 | 5.6±7.2 |
70% of patients (334/480) included in the study drug received ART plus supplement (calcium and/or vitamin D). As for the number of initial treatment prescribed, there were 482, because of the 480 patients included, two received a double ART initial treatment regimen (a bisphosphonate and SERM), considered as two different patterns, one for each type of ART. The initial regimen of ART more calcium and vitamin D was more frequent for the total sample (62.6% for the treatments prescribed 302/482), and specialties (UMO/rheumatology 82.4% corresponding to 136 / 166 of the prescribed treatments; PC 137/253 54% corresponding to prescribed treatments, 46% gynecologists prescribed treatments 29/63). Statistically significant differences were observed among the three specialty groups (P<.01) (Table 2).
Description of the Type of the Pattern of Antiresorptive Treatment With or Without Supplements Started in Patients Sampled According to Medical Specialty.
| Primary Care | Gynecology | BMU/Rheumatology | Total | |
| n (%) | n (%) | n (%) | n (%) | |
| Antiresorptive treatment | 100 (39.7%) | 28 (44.4%) | 18 (10.9%) | 146 (30.7%) |
| Antiresorptive treatment plus calcium | 12 (4.8%) | 6 (9.5%) | 12 (7.3%) | 30 (6.3%) |
| Antiresorptive plus calcium and vitamin Da | 137 (54.0%) | 29 (46.0%) | 136 (82.4%) | 302 (62.6%) |
| Antiresorptive plus vitamin D | 4 (1.6%) | 4 (0.8%) | ||
| Total | 253 (100.0%) | 63 (100.0%) | 166 (100.0%) | 482 (100.0%) |
P<.01, chi squared test.
The second most common treatment regimen in all specialties was ART without any associated drugs 30.7% of prescribed treatment regimens (146/482 treatments). Analyzing the patterns of initial treatment by specialty, we note that in PC and gynecology, the percentage of patients on ART was only 39.7% (corresponding to the prescribed treatments 100/253) and 44.4% (corresponding to 28/63 treatments prescribed), respectively, while the percentage is observed only in patients on ART recruited by BMU/rheumatology was lower (10.9%, corresponding to treatments prescribed 18/166) compared with other specialties (Table 2).
Pharmacological SupplementationPharmacological supplements are prescribed with ART in 69.6% (334/480) of patients included in the study. According to specialties, BMU/rheumatology prescribed pharmacological supplements to 89.1% of patients, while for patients seen in primary care and gynecology the percentage of those receiving pharmacological supplements was 60.3 and 55.6%, respectively (Table 3).
Use of Supplements by Medical Specialty.
| Primary Care | Gynecology | BMU/Rheumatology | Total | |
| Use of supplements, n (%) | ||||
| Yes | 152 (60.3%) | 35 (55.6%) | 147 (89.1%) | 334 (69.6%) |
| No | 100 (39.7%) | 28 (44.4%) | 18 (10.9%) | 146 (30.4%) |
| Total | 252 (100%) | 63 (100%) | 165 (100%) | 480 (100%) |
| Type of supplement, n (%) | ||||
| Calcium | 13 (8.5%) | 6 (17.1%) | 12 (8.1%) | 31 (9.3%) |
| Calcium plus vitamin D | 135 (88.8%) | 29 (82.8%) | 135 (91.8%) | 299 (89.5%) |
| Vitamin D | 6 (3.9%) | – | 1 (0.6%) | 7 (2%) |
| Total | 152 (100%) | 35 100%) | 147 (100%) | 334 (100%) |
The sum of different supplements is not the total sum because 2 patients started with calcium and vitamin D plus vitamin D and another calcium and vitamin D.
Of all patients who received pharmacological supplements, 89.5% (299/334) of these patients included calcium and vitamin D in their initial regimen. 9.3% (31/334) of patients were prescribed calcium and 2% of patients (7/334) received vitamin D (Table 3).
When analyzing the type of supplement by type of specialty, it was observed in all type of supplement that most commonly prescribed drug was calcium plus vitamin D, in UMO/Rheumatology at 91.8% of patients (135/147) and AP and gynecology consultation in 88.8% (135/152) and 82.8% (29/35) of patients, respectively (Table 3).
None of the patients included in the study through gynecology received vitamin D supplements alone as the initial pharmacological treatment.
Use of Antiresorptive Therapy TreatmentsThe most common ART in the initial regimen (with or without pharmacological supplements) was bisphosphonates in 79.2% (380/480 patients) of cases, compared to 21.3% (102/480) of SERM-treated patients. We found statistically significant differences between specialties in the use of bisphosphonates, the most frequent being the use of bisphosphonates in PC and BMU/rheumatology (81.7% and 83%, respectively), while the percentage of bisphosphonate use was bellowerow in gynecology, with 58.7% of the sample recruited by gynecologists (P<.01) (Table 4).
Initial ART and Pharmacologic Supplements by Medical Specialty.
| Type of ART No. (%) | Primary Care | Gynecology | BMU/Rheumatology | Total |
| SERM | 47 (18.7%) | 27 (42.9%) | 28 (17%) | 102 (21.3%) |
| Biphosphonate | 206 (81.7%) | 37 (58.7%) | 137 (83%) | 380 (79.2%) |
| Alendronatea | 118 (57.2%) | 25 (67.6%) | 73 (53.3%) | 216 (56.8%) |
| Alendronate+vitamin Da | 10 (4.8%) | – | 4 (2.9%) | 14 (3.7%) |
| Etidronate | 2 (0.9%) | – | – | 2 (0.5%) |
| Risedronate | 76 (36.9%) | 12 (32.4%) | 60 (43.8%) | 148 (38.9%) |
| Total | 252 (100%) | 63 (100%) | 165 (100%) | 480 (100%) |
Among the bisphosphonates (alendronate, etidronate, and risedronate) alone or with pharmacological supplements (calcium and/or vitamin D), alendronate was the most frequently prescribed, observed in 60.5% of the total sample including bisphosphonates as initial regimen (230/380 patients) followed by risedronate in 38.9% (148/380 patients) (Table 4). Per medical specialty, alendronate accounted for 62.1% (128/206 patients) of PC patients, 67.6% (25/37 patients) of patients from gynecology and 59.1% (77/137) of patients seen by BMU/rheumatology treated with bisphosphonates as the initial regimen (Table 4).
The highest percentage of use of SERM observed was in patients included by gynecologists compared to the rest of patients selected by other specialists (42.9% compared to 18.7% in gynecology and 17% in PC and BMU/rheumatology, respectively) (Table 4).
The Main Reasons for Indication of Antiresorptive Treatments and/or Pharmacological Supplements97.7% (469/480) of patients in which the reasons were available indicated that ART treatment was started in 64.6% (303/469) of cases for primary prevention and rest for secondary prevention.
We also assessed the main criteria of indication for treatment with ART, available in 470 of the 480 patients enrolled (97.9% of the sample). Of these, 71.9% (338/470) were prescribed ART following the BMD criterion, and the presence of risk factors accounted for 28.1% of patients (132/470).
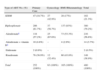
Medical Opinion Survey on Drug Supplements (Calcium and Vitamin D)Of the 88 physicians participating in the study, 76 (86.4%) responded to a survey on drug supplements (calcium and/or vitamin D). 42.1% of researchers believed that 10%–25% of patients have an adequate calcium intake, although no statistically significant differences were seen by type of specialists. The percentage of patients with adequate levels of vitamin D according to the researchers is between 25% and 50% (no significant differences by type of specialist). However, in the degree of agreement with the statement “calcium supplements are needed in the treatment for osteoporosis”, only 28.2% of GPs (11/39 researchers) were in full agreement with this statement, compared to 68% (17/25 researchers) of researchers from BMU/rheumatology and 75% (9/12 researchers) of gynecologists (P=.023). The same trend was observed in the percentage of researchers who strongly agree with the statement “Vitamin D supplements are necessary in the routine treatment of osteoporosis” with 38.5% of researchers from PC, 72% from BMU/rheumatology and 66.7% from gynecology (P=.058). According to the results of the survey, 46.2% of primary care physicians and 58.3% of gynecologists reported prescribing some type of supplement (calcium and/or vitamin D) in at least 75% of its patients, while the percentage was 92% in BMU/rheumatology (P<.01). As for side effects (SE) of pharmacological supplements (calcium and/or vitamin D), 75% of gynecologists reported that the presence of SE with the supplements are present in less than 10% of patients while this percentage would also be found for 48% of BMU/rheumatology and 35.9% of primary care physicians (Table 5).
Opinion Survey. Distribution of Answers Obtained on the Whole of Participating Physicians and in Relation to their Specialty (% of Participating Doctors).
| Primary Care | Gynecology | BMU/Rheumatology | Total | |||||
| n | % | n | % | n | % | n | % | |
| What percentage of patients do you believe has an adequate dietary calcium consumption? | ||||||||
| <10% | 4 | 10.3% | 1 | 8.3% | 3 | 12.0% | 8 | 10.5% |
| 10%–25% | 12 | 30.8% | 7 | 58.3% | 13 | 52.0% | 32 | 42.1% |
| >25%–5%–0% | 14 | 35.9% | 3 | 25.0% | 7 | 28.0% | 24 | 31.6% |
| >50%–75% | 6 | 15.4% | 1 | 8.3% | 1 | 4.0% | 8 | 10.5% |
| >75% | 3 | 7.7% | 1 | 4.0% | 4 | 5.3% | ||
| Total | 39 | 12 | 25 | 76 | ||||
| What percentage of patients do you believe has adequate vitamin D levels? | ||||||||
| <10% | 2 | 5.1% | 2 | 2.6% | ||||
| 10%–25% | 13 | 33.3% | 4 | 33.3% | 8 | 32.0% | 25 | 32.9% |
| >25%–50% | 19 | 48.7% | 3 | 25.0% | 10 | 40.0% | 32 | 42.1% |
| >50%–75% | 4 | 10.3% | 5 | 41.7% | 6 | 24.0% | 15 | 19.7% |
| >75% | 1 | 2.6% | 1 | 4.0% | 2 | 2.6% | ||
| Total | 39 | 12 | 25 | 76 | ||||
| Calcium supplements are necessary for the standard treatment of osteoporosisa | ||||||||
| TA | 11 | 28.2% | 9 | 75.0% | 17 | 68.0% | 37 | 48.7% |
| A | 16 | 41.0% | 2 | 16.7% | 6 | 24.0% | 24 | 31.6% |
| NA ND | 10 | 25.6% | 1 | 8.3% | 2 | 8.0% | 13 | 17.1% |
| D | 2 | 5.1% | 2 | 2.6% | ||||
| Total | 39 | 12 | 25 | 76 | ||||
| Vitamin D supplements are necessary for the standard treatment of osteoporosis | ||||||||
| TA | 15 | 38.5% | 8 | 66.7% | 18 | 72.0% | 41 | 53.9% |
| A | 21 | 53.8% | 4 | 33.3% | 7 | 28.0% | 32 | 42.1% |
| NA ND | 3 | 7.7% | 3 | 3.9% | ||||
| Total | 39 | 12 | 25 | 76 | ||||
| Approximately, what percentage of patients are prescribed a supplement of calcium and vitamin D along with antiresorptive agents?b | ||||||||
| <10% | 1 | 8.3% | 1 | 1.3% | ||||
| 10%–25% | 3 | 7.7% | 3 | 3.9% | ||||
| >25%–50% | 5 | 12.8% | 1 | 8.3% | 6 | 7.9% | ||
| >50%–75% | 13 | 33.3% | 3 | 25.0% | 2 | 8.0% | 18 | 23.7% |
| >75% | 18 | 46.2% | 7 | 58.3% | 23 | 92.0% | 48 | 63.2% |
| Total | 39 | 12 | 25 | 76 | ||||
| What percentage of patients do you consider that will present adverse events in relation to calcium and vitamin D supplements? | ||||||||
| <10% | 14 | 35.9% | 9 | 75.0% | 12 | 48.0% | 35 | 46.1% |
| 10%–25% | 14 | 35.9% | 2 | 16.7% | 10 | 40.0% | 26 | 34.2% |
| >25%–50% | 7 | 17.9% | 1 | 8.3% | 3 | 12.0% | 11 | 14.5% |
| > 50%-75% | 4 | 10.3% | 4 | 5.3% | ||||
| Total | 39 | 12 | 25 | 76 | ||||
A: in agreement; D: in disagreement; NA NDno agreement or disagreement; TA: total agreement; TD: total disagreement.
Data from this study have provided information on the use of calcium supplements and/or vitamin D in the initial treatment of osteoporosis by physician specialty, showing that more than half of patients received pharmacological supplements along with ART, being the most common regimen that of calcium plus vitamin D.
Although current clinical practice guidelines agree that the ART associated with pharmacological supplements of calcium and vitamin D should be prescribed to all patients with osteoporosis, having a fracture or not,8,22–24 the results of this study show that in our country there is still a considerable percentage of patients who received an ART regimen as initial therapy without associating it with drug supplements (calcium and/or vitamin D). These percentages vary importantly when analyzing the data by medical specialty, and while BMU/rheumatology specialists include pharmacological supplements at the onset in the most patients; this percentage is reduced in patients treated by primary care and gynecology. It is likely that these differences are due to a profile of greater severity of osteoporosis among patients served by BMU/rheumatology, in which we observed a higher proportion of patients with a history of fracture, or perhaps due to an increased interest of these specialists in compliance with the guidelines. On the other hand, it is interesting to note that patients included by GPs have a greater proportion of concomitant diseases, which is usually associated with polypharmacy, so the doctor may try to limit the supplements.
These results are consistent with the results of the survey asking about the percentage of supplement prescription by specialty: BMU/rheumatologists were those who said they prescribed supplements in a high proportion to their patients, while the percentage of primary care physicians and gynecologists is much lower. These data are in line with other previously published regarding the difference in treatment criteria by specialty25 and variability of clinical practice.
In the same survey, less than half of the researchers felt that 10%–25% of patients have an adequate intake of calcium and vitamin D, although no statistically significant differences were seen in specialists. These data could be significant if more data were available in each of the response categories of items in the survey.
These results may be comparable to those previously observed in a study several years ago in rheumatology consultations of Spain, which found deficient levels of vitamin D (87% of women were under 20ng/calcidiolml).26
The drug supplements pattern most frequently prescribed was the combination of calcium plus vitamin D, while the use of isolated calcium or vitamin D occurred in a very low percentage of cases. These data differ from the results of a previous study in the U.S. in 2003, in which it was observed that 41.9% of women diagnosed with osteoporosis took only calcium supplements, well above the 9.2% in our study.27 These results suggest that although the percentage of patients who are prescribed pharmacological supplements at the onset is not too high, there is a widespread practice of including calcium and vitamin D together when they are included as standard pharmacological supplements with ART, as recommended by practice guidelines.8,22–24
Although the number of patients enrolled through BMU is low, the proportion of the participating centers was equivalent to that of units in Spain at the time of the study. A limitation of this study is that the selection of researchers was carried out following geographical or population distributions, although we have tried to involve study centers around the country. Another factor that limits the representativeness of the results is that the sample comes from subjects selected from patients who came spontaneously to the clinic and whose data were collected retrospectively.
Although the data presented are the results of a subanalysis of a study with a different main purpose, the study design is adequate to estimate the use of supplements in patients initiating ART, so that information presented can form the groundwork for future studies in this field.
In conclusion, we can say that the use of pharmacological supplements in the initial regimen of ART accounts for over half the study sample, and the prescription of pharmacological supplements is mainly based on calcium and vitamin D in accordance with the recommendations of the clinical practice guidelines. On the other hand, variability has also been observed among specialists regarding the rate of prescription of pharmacological supplements in the initial treatment regimen, and this aspect is also reflected in the survey of participants by the same researchers, showing a higher percentage in supplement prescriptions by BMU/Rheumatology compared to other specialties.
Given the importance of preventive treatment of osteoporosis, it would be interesting to conduct future studies for analyzing the variability of some aspects of therapeutic management and to understand more fully the reasons that lead a doctor to prescribe certain treatment regimens.
Conflict of InterestStudy was financed by Merck Sharp & Dohme de España S.A.
Please cite this article as: Carbonell C, et al. Pauta de tratamiento inicial en pacientes con osteoporosis: uso de antirresortivos y suplementos farmacológicos (calcio y vitamina D) en la práctica clínica. Reumatol Clin. 2012;8(1):3–9.