We present the case of a 49-year-old male with a history of hyperlipidemia and significant alcohol intake. In May 2004, during an outpatient visit, he referred 10 years of recurrent episodes of monoarthritis lasting three days, successively affecting either the left knee, left tarsus, elbow, left or bilateral first metatarsophalangeal joints, with no other accompanying symptoms. Physical examination showed signs of a left knee effusion, restricting flexion to 90° and tophi on the left olecranon.
Laboratory tests showed uricemia of 9.4mg/dl and GGT 166U/dl. The remaining parameters (CBC, TSH, CPK, rheumatoid factor, HLA B27, anti-CCP antibodies, immunoglobulins, 24h urine uric acid) were normal. X-rays of the left foot were performed (Fig. 1), showing marginal erosions and sclerotic borders of the first metatarsal head, with increased adjacent soft tissue. A left knee radiograph (Fig. 2) showed lytic lesions with well-defined edges and incipient degenerative changes of the tibial epiphysis at the femorotibial level. We performed arthrocentesis of the left knee. Monosodium urate crystals were found in synovial fluid (SF). SF culture was negative.
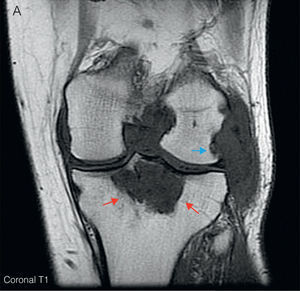
Given the radiological lesions of the left knee, we completed the study with a left knee MRI (Fig. 3) which showed synovial proliferation which revealed diffuse, hypointense lesions on T1, with bone erosions in the posterolateral margin of the femoral condyle. A large Baker's cyst with areas of high and low signal on T2 were seen, as well as lytic, hypointense lesion on T1, T2 with a heterogeneous signal level on the proximal tibial epiphysis and a maximum diameter of 5cm that after administration of gadolinium showed enhancement, something characteristic of tophaceous deposits.
(A) Left knee coronal T1MRI. It shows a diffuse hypointense synovial proliferation with bone erosion of the posterolateral margin of the femoral condyle (blue arrow) and intercondylar notch. A hypointense lytic lesion is seen in the proximal tibial epiphysis with a maximum diameter of 5cm (red arrows). (B) Sagittal T2. There is an increased signal heterogeneity at the level of the tibial epiphyseal lytic lesion (red arrows), along with a large Baker's cyst located behind the medial gastrocnemius muscle (green arrows), with areas of high and low signal for synovial hypertrophy. (C) Sagittal T1-Gd. After administration of gadolinium, enhancement shows the level of peripheral tibial lytic lesion (red arrows) and Baker's cyst (green arrows). (For interpretation of the references to color in this figure legend, the reader is referred to the web version of the article.)
Based on the above, the patient was diagnosed with chronic gouty arthritis with intraosseous and intraarticular tophi. Dietary measures were initiated and treatment begun with allopurinol (300mg/d) and colchicine 1mg daily. Due to the persistence of clinical uricemia of 6.2mg/dl, benzbromarone was added (up to 100mg doses per day), until the patient was asymptomatic. Current levels of uric acid are 3.6mg/dl and there was a slight decrease of the tibial intraosseous tophus size.
DiscussionIt is estimated that the prevalence of gouty arthritis in the general population is 1.4%,1 and represents approximately 5% of monoarthritis seen in consultation. The tophus is a nodular mass composed of sodium urate salts and surrounded by a chronic inflammatory reaction with abundant vascularization. It is a late complication of hyperuricemia maintained and present in only a minority of patients. They usually form in juxta-articular regions, although virtually any tissue2 can present them. It is not uncommon for intraosseous tophi to form in advanced crystal arthropathy, reaching 13.3% in patients in some series.3 A definitive diagnosis requires histopathological confirmation, but imaging tests may be useful. Plain radiographs can show juxta-articular and intraosseous calcifications and erosions of the articular surface, creating problems of differential diagnosis with avascular4 necrosis and osteochondroma. The presence of bone erosions is a marker of intrabone5 tophi. These can be seen as a soft tissue or intraosseous mass. The joint space is generally respected and periosteal new bone formation and subchondral collapse can appear. Is a useful tool to determine the severity of involvement, with standardized methods and a Sharp/Van der Heijde6 score available for indexing. Ultrasound is a useful tool for its low cost, no radiation, and speed of implementation, also used to guide invasive techniques. It has a high sensitivity for detecting monosodium urate deposits, even in patients with asymptomatic hyperuricemia. It is able to appreciate bone erosions earlier than plain X-rays. On the other hand, it is the only standardized technique for measurement of tophi and can demonstrate subclinical inflammatory activity by capturing Doppler hypervascular areas around the monosodium urate deposits. The typical findings in gout with this technique are: a double contour sign, aggregated punctate echogenic tissue, “snow storm” synovial fluid appearance with hyperechogenic areas, and soft tissue edema, in addition to the aforementioned bone erosions and hypervascularity.6–8 Computed tomography (CT) is useful in the recognition of monosodium urate deposits. These deposits have an attenuation of approximately 160 Hounsfield units (HU), while calcium crystals exhibit an attenuation of 450HU, even bone tissue and calcified tophi.8 It provides more specific images than ultrasound or MRI, as well as aid in the diagnosis of complications, and intraosseous tophi and bone erosions, and can guide joint aspiration.6 Magnetic resonance imaging (MRI) is a tool that, while non-specific and with certain limitations, such as suboptimal definition for intraosseous abnormalities, a high cost, and poor availability, is the method of choice for evaluating soft tissue, ligaments, muscles and tissues as well as juxta-articular joint space, and effusions or synovial proliferation, cartilage abnormalities, due to a spatial resolution far superior to other imaging tests. In particular, it has great utility in determining the etiology of functional limitations of unknown causes in the knee joint in patients with gout.2,6 Importantly, the synovial membrane is too thin to be assessed with this imaging method, so that it can only be seen when a pathological process enlarges it. The differential diagnosis of synovial thickening raises the possibility of longstanding rheumatoid arthritis, pyrophosphate arthropathy, villonodular synovitis, hemophilic arthropathy, amyloid arthropathy, synovial chondromatosis, and chronic granulomatous processes such as arthritis or fungal infection or tuberculosis.2,6,9 Gout is often found presenting a synovial effusion and synovial pannus. The tophi are seen as an amorphous lesion, eccentric and asymmetric, with variable intensity depending on their composition: protein, fibrous crystals, hemosiderin, and calcium, although the latter are rare and found in very old lesions. It is common to observe one of these morphological patterns: amorphous mass, linear crystalline deposits, or cystic lesions in the juxta-articular bursa. Intraosseous tophi are hypointense or of intermediate intensity on T1, heterogeneous-looking from hyper-to hypointense on T2, depending on the amount of calcium in the tophi, with more calcium, less intensity. It usually enhances after contrast administration, which translates hypervascularization and is a predictor of bone erosion. It also often is accompanied by juxta-articular findings such as erosions, edema of soft tissues, bone marrow edema, or extraarticular2 tophi.3,6,9–11 Isolated tophi may pose problems in differential diagnosis with tumors such as fibroblastic tumors and benign xantofibroma, but it is rare to find surrounding edema in these.10
In short, chronic tophaceous gout presents a constellation of clinical and radiological findings which are important to know for a correct differential diagnosis and further treatment. Although MRI is not a specific test for the diagnosis of gout, it does allow early detection of intraosseous and intraarticular tophi and bone erosions in patients with gout, helping us to recognize this entity and avoid a bone biopsy in selected patients. Thus, MRI can play a special role in the identification of clinical complications and monitoring response to treatment.
Ethical disclosuresProtection of human and animal subjects. The authors declare that no experiments were performed on humans or animals for this investigation.
Confidentiality of Data. The authors declare that they have followed the protocols of their work centre on the publication of patient data and that all the patients included in the study have received sufficient information and have given their informed consent in writing to participate in that study.
Right to privacy and informed consent. The authors have obtained the informed consent of the patients and /or subjects mentioned in the article. The author for correspondence is in possession of this document.
Please cite this article as: Rodríguez Leal CM, et al. Tofo tibial intraóseo en gota crónica. Reumatol Clin. 2012. doi:10.1016/j.reuma.2011.10.010.