The purpose of this study is to determine the rate of bleeding complications in patient's anticoagulated with acenocoumarol according to the international normalized ratio (INR) coagulation index. A cross-sectional study was performed with 901 charts of patients who underwent arthrocentesis or joint infiltration between 2009 and 2013; the charts were grouped on the basis of having an INR higher or lower than 2.0 (268 and 633, respectively). Comparisons were performed in terms of rates of early or late bleeding complications. A 0.37% rate of early bleeding complications (<24h) was observed in the group of patients with INR<2 and 0.99% in the group of patients with INR≥2 (P=.47). Only one case of late complication was presented by bleeding between 24h and 30 days, in the group of patients with INR≥2. We conclude that oral anticoagulation with acenocoumarol at therapeutic doses does not increase the risk of bleeding joint punctures.
El propósito del presente estudio es determinar la tasa de complicaciones por sangrado en pacientes anticoagulados con acenocumarol en función del índice normalizado internacional (INR) de coagulación. Se realizó un estudio retrospectivo con 901 registros de pacientes a quienes se les practicó una artrocentesis o infiltración articular entre 2009 y 2013, se agruparon los registros en función de tener un INR superior o inferior a 2,0 (268 y 633 registros, respectivamente) y se compararon las tasas de complicaciones por sangrado. Se observó una tasa de 0,37% de complicaciones por sangrado tempranas (<24h) en el grupo de pacientes con INR<2 y una tasa de 0,99% en el grupo de pacientes con INR≥2 (p=0,47). Solo se presentó un caso de complicación por sangrado tardío, entre 24h y 30 días, en el grupo de pacientes con INR≥2. Concluimos que la anticoagulación oral a dosis terapéutica con acenocumarol no incrementa el riesgo de sangrado por punciones articulares.
The diagnostic and therapeutic treatment of patients with joint disease in the emergency room often includes the need for joint or perijoint1 punctures. Anticoagulant treatment is often an impediment to these procedures because of the risk of bleeding.2 This represents a significant obstacle to performing these procedures as it is estimated that around 12 per 1000 inhabitants in Spain are receiving oral anticoagulants.3 This resistance, however, does not seem to be supported in the few studies performed with warfarin2,4,5 and, on the other hand, delays diagnosis with the potential risk of irreparable joint damage or even death.1,6,7 No studies have been conducted to measure this risk in acenocoumarol users.
The objective of this study is to determine the risk of complications related to the performance of joint puncture in patients who are on anticoagulant therapy with acenocoumarol at therapeutic doses.
Patients and MethodsA retrospective study of the records of 760 patients in whom 901 arthrocentesis or joint infiltration procedures were performed between 2009 and 2013, done in 3 centers: Emergency Department of the Hospital Universitario Ramón y Cajal (Madrid), Comprehensive Diagnostic and Treatment Center “Francisco Diaz” (Alcalá de Henares) and “San Juan” (Arganda del Rey) Medical Center. All patients were receiving anticoagulant treatment with acenocoumarol. All records included had an analytical determination of the international normalized ratio (INR) coagulation on the same day of the procedure or before up to 24h.
804 arthrocentesis or infiltrations (89%) were performed in the Emergency Department of the Hospital Universitario Ramón y Cajal. The rest of the procedures were performed in the other 2 centers. In all the centers, patients had a notification mechanism for immediate complications, except in the “San Juan” (11 patients) Medical Center as the center itself has no means of urgent assessment and emergencies are referred to other institutions.
The technique for performing the procedures followed no pattern or established protocol. In 12% of the procedures, ultrasound guidance in real time was used.
Records were stratified into 2 groups according to the arbitrary criterion used in the largest series of patients treated with warfarin2 as a function of having an INR equal to or greater than 2.0 or maintained below this figure. The use of low molecular weight heparins as replacement therapy in cases of suspension of acenocoumarol or the use of antiplatelet therapy was not considered.
Study VariablesEpidemiologic variables of patients, data on use of antiplatelet therapy and comorbidities were simultaneously collected. The main variables were clinically significant bleeding and significant joint pain within 30 days from the day of the procedure.
DefinitionsClinically significant bleeding: bleeding during the period immediately following the procedure that required reversal of anticoagulation, hospitalization or surgery.
Clinically significant joint pain: joint pain related to the procedure that has caused the patient to seek further medical evaluation.
The assessment of the main variables was performed 24h after the procedure, within 24h and the thirtieth day after the procedure.
Statistical AnalysisSynthesized global baseline variables were analyzed using central descriptive statistics and dispersion measures. To determine the presence of confounding variables between the groups according to the number of INR, a Wilcoxon test was used for continuous variables and a Fisher's exact test for dichotomous variables. The complication rate per group was compared using Fisher's exact test. All statistical tests were 2-tailed with an alpha error of 0.05. For statistical analysis, the gstat program v2.0 (Biometrics Department, GlaxoSmithKline SA, Tres Cantos, Madrid) was used.
ResultsBetween 2009 and 2013 records of 901 infiltration procedures or arthrocentesis performed in 760 patients were reviewed.
Most procedures were performed by a rheumatologist (77.6%) or a family physician (16.6%). 5.8% of the procedures were performed by orthopedic or rehabilitation physicians. The most frequently infiltrated or aspirated joints were the knee and shoulder. 58% of the procedures were performed on the knee, 40% on the shoulder and 2% on other joints. Seventy-two percent of the procedures were infiltrations, 14% were aspirations and 14% were aspirations and injections. Six hundred and thirty-three procedures were performed in patients with an INR≥2.0 and 268 in those with an INR<2.0. 100% of the infiltrations had a therapeutic indication. 88% of the arthrocentesis had a diagnostic indication, 10% a therapeutic indication and in 2% the indication was identified in the medical record.
Of interest we noted that the INR values for the first group interval was 2.0–8.1, with an average of 2.9; SD: 1.6.
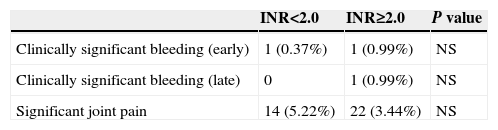
Two clinically significant bleedings were recorded. Both occurred before the first 72h of knee arthrocentesis (INR 3.4) and a shoulder infiltration (INR 1.9). Higher concentrations of clinically significant pain were not identified according to INR levels in any of the two groups. The mean INR of the patients who had clinically significant pain was 1.4 and 3.3 in the group INR<2.0 or ≥2.0, respectively.
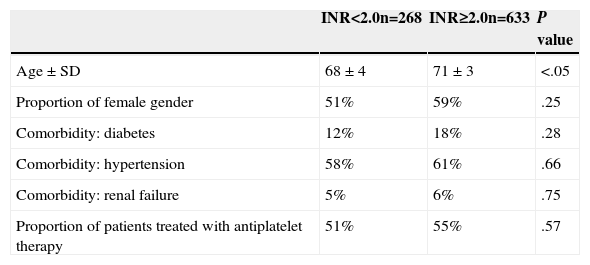
Table 1 summarizes the baseline characteristics of the 2 groups. No significant differences in the proportion of female patients, the mean age, comorbidities (hypertension, diabetes, renal failure) and use of antiplatelet agents were identified.
Baseline Characteristics of Patients in Whom the Procedures Studied Were Performed.
| INR<2.0n=268 | INR≥2.0n=633 | P value | |
|---|---|---|---|
| Age±SD | 68±4 | 71±3 | <.05 |
| Proportion of female gender | 51% | 59% | .25 |
| Comorbidity: diabetes | 12% | 18% | .28 |
| Comorbidity: hypertension | 58% | 61% | .66 |
| Comorbidity: renal failure | 5% | 6% | .75 |
| Proportion of patients treated with antiplatelet therapy | 51% | 55% | .57 |
No statistically significant differences in the rate of clinically significant bleeding or the rate of clinically significant pain between the two groups (Table 2) were identified.
Of the 22 procedures performed on the patients with INR≥2.0 in whom there had been clinically significant pain, 17 (77.2%) were performed by rheumatologists, 3 (13.6%) by family physicians and one (4.5%) by an orthopedist. Of the 14 procedures performed in patients with INR<2.0; 9 (64.2%) were made by rheumatologists and 5 (35.7%) by family physicians. No statistically significant differences were identified in the development of complications depending on the specialist who performed the procedure (P>.05 for both comparisons).
DiscussionThis is the first article in which complications related to the performance of joint puncture in anticoagulated patients with acenocoumarol are presented. According to our results, we believe that the use of acenocoumarol at therapeutic doses does not pose an increased risk of bleeding when performing arthrocentesis or infiltration and, therefore, delaying these procedures to reverse the INR is unnecessary. The few available studies with warfarin agree that there are no statistically significant differences in the rate of bleeding complications according to the INR at the time of the procedure.2,4,5 Both treatments, acenocoumarol and warfarin, act on coagulation factors dependent on vitamin K, differing primarily in that the half-life of warfarin is around 48h, while that of acenocoumarol is 10h.3,8,9
The results of our study are consistent with those obtained by Ahmed and Gertner2 in terms of early and late complications due to bleeding, but in our study, joint pain was much higher in both the groups. This increase could be explained by the fact that a significant proportion of the patients whose records were included came from an area where access to emergency re-evaluations is relatively easy. Both Thumboo and O’Duffy4 and Salvati et al.5 performed prospective studies that had a small sample size, agreed that the rate of bleeding complications in patients using warfarin was low and confirmed the safety of these procedures without reversing anticoagulation.
Limitations of the StudyThe first limitation of this study is its retrospective nature and the possibility of underreporting complications. The data collection model was based on the study of Ahmed and Gertner.2 We believe that the arbitrary definitions of the main variables are limited to circumstances of real clinical interest and the probability of underreporting is low and in any event within 2 homogeneous groups of patients.
The second limitation is the lack of homogeneity of the groups according to the value of the INR. In our study, older age was observed in the group of patients with INR≥2. We do not believe that this difference justifies the slight increase in bleeding complications or the need for repeated pain assessment. By contrast, whereas no statistically significant differences were identified, a reduction in the age difference would play for a minor difference in the occurrence of these complications.
Taking these two considerations into account, the sample size of our study is the largest ever published and it is the first study with patients using acenocoumarol; we believe our results can serve as a basis for considering that oral anticoagulation should not be a risk factor for the development of bleeding complications after joint puncture and, therefore, its performance should not delay the procedure when indicated.
Ethical ResponsibilitiesProtection of human and animal subjectsThe authors declare that this research did not perform experiments on humans or animals.
Confidentiality of dataThe authors declare that they have followed the protocols of their workplace regarding the publication of data from patients, and all patients included in the study have received sufficient information and gave written informed consent to participate in the study.
Right to privacy and informed consentThe authors have obtained informed consent from patients and/or subjects referred to in the article. This document is in the possession of the corresponding author.
Conflict of InterestThe authors declare no conflict of interest.
Please cite this article as: Guillen Astete C, Boteanu A, Medina Quiñones C, Garcia Montes N, Roldan Moll F, Carballo Carmano C, et al. ¿Es seguro realizar infiltraciones o aspiraciones articulares en pacientes anticoagulados con acenocumarol? Reumatol Clin. 2015;11:9–11.