Jaccoud arthropathy (JA) is a recurrent form of arthritis that initially produces reversible deformities of the hands and feet (less frequently knees, shoulders and wrists) and can lead to erosions that are different from those in rheumatoid arthritis (RA).1 Its association with autoimmune diseases has been described, particularly systemic lupus erythematosus (SLE), but also with systemic sclerosis (SS).2–4 Primary biliary cirrhosis (PBC) is a chronic cholestatic disease of autoimmune origin, characterized by the presence of anti-mitochondrial antibodies (AMA) which is the most common liver disorder SS (especially the limited cutaneous form), with an estimated prevalence of 3%–50%,5 this association is known as Reynolds (RS) syndrome and its first description was in 1971.6 Although arthritis occurs in 4%–42% of patients with PBC.7 JA development has not been previously described in this single entity or in RS.
We present the case of an 80-year-old woman, diagnosed at 57 with seronegative RA based on symmetric polyarthritis affecting metacarpophalangeal (MCP) and proximal interphalangeal (PIP) of the hands, wrists, hips and knees. She underwent treatment with gold salts, which were suspended after one year due to impaired cholestatic liver function, with a biopsy compatible with PBC. Since then she has received varying doses of corticosteroids, NSAIDs on demand and ursodeoxycholic acid 600mg/day. The liver function remained stable but she developed multiple joint deformities; as a result of steroids, she developed osteoporosis with inferior pubic ramus fracture and osteonecrosis of the left hip. From the age of 68 she began presenting Raynaud's phenomenon in the hands and feet without digital ulcers, xerostomia and xerophthalmia.
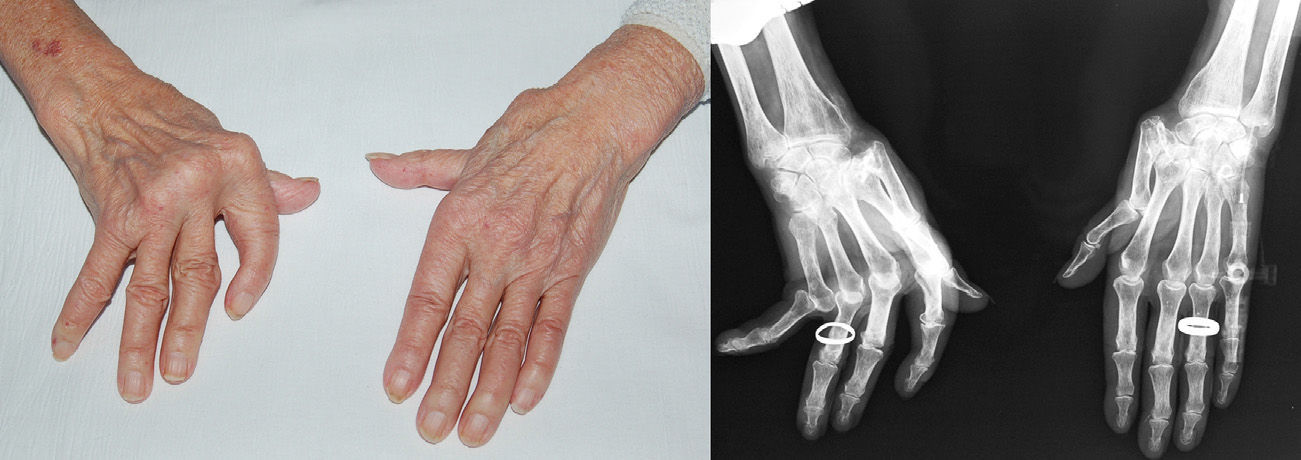
In March 2010, she was referred to our center for back pain secondary to a sacral fracture and vertebral collapse. Examination revealed nasal sharpening, microstomia, facial telangiectasias and distal sclerodactyly, subluxation and ulnar deviation of MCP predominantly on the right, ‘gooseneck’ deformity and ‘Z’ deformity of the thumbs (Fig. 1A), and hallux valgus and subluxation of metatarsophalangeal joints, with no signs of active synovitis. Cardiopulmonary auscultation was normal. Laboratory tests revealed slightly elevated liver enzymes (alkaline phosphatase 144U/l, gamma glutamyl transferase 93U/l), C-reactive protein 6.62mg/l, erythrocyte sedimentation rate 55mm/h, antinuclear antibody 1/320 with centromere antibodies and positive AMA, but the results for nuclear extractable antigen antibodies, cyclic citrullinated-peptide (anti-CCP), and rheumatoid factor (RF), complement and immunoglobulins were negative or normal. Radiology confirmed the hand deformities described and demonstrated the absence of erosions; calcification of the triangular ligament of the right carpus was also observed (Fig. 1B), and capillaroscopic study revealed the presence of dilated and tortuous loops without avascular areas. The diagnosis of SS limited to the skin associated with PBC and JA was established, being discharged with prednisone 5mg/day and calcium and vitamin D, and adding, in a later visit, alendronate 70mg/week, with adequate fracture recovery and good pain control.
Jaccoud arthropathy on the hands, with ulnar deviation of the MCP, ‘gooseneck’ deformity and ‘Z’ thumb deviation with these deformities being more pronounced on the right hand (A). X-ray of the hands in which, in addition to the abovementioned deformities we find juxtaarticular osteopenia, chondrocalcinosis of the right carpus and absence of erosions or degenerative signs (B).
Joint involvement in SS appears in 46%–97% of cases and may be the initial manifestation prior to Raynaud's phenomenon in 12%–65%.8 It presents as joint pain, arthritis, morning stiffness and functional limitation secondary to flexion contractures, relating both to joint inflammation and mechanical restriction secondary to periarticular fibrosis.4 Radiographic changes are usually mild, but some patients develop erosive arthritis similar to RA, with it associating with calcinosis and acrosteolisis.8 However, the development of JA is quite uncommon, with only 4 cases reported to date,2–4 so it is considered that it may correspond more to the coexistence of idiopathic JA than a manifestation of SS.3 It has been suggested that JA in SLE associated with inflammatory activity due to prolonged or recurrent low degree swelling of the synovial membrane and joint capsule, and ligamentous laxity cause an imbalance of muscle forces. However, in cases of associated JA and SS there is no clinical or imaging2,3 inflammation evident, so other mechanisms could be involved, including pericapsular and tendon fibrosis.1 A symmetrical erosive arthritis of small joints, often RF positive, has been described in PBC, which can be indistinguishable from RA. Up to 31% of PBC cases develop arthritis, characterized by a non-deforming asymmetric affection (although cases have been reported with deforming/erosive arthritis), negative for RF and anti-CCP, and recently it has been shown that it has a special histopathology regarding synovial infiltration predominantly by B lymphocytes and plasma cells.7 However, JA is not described in these patients. Pyrophosphate deposition disease has also been associated with JA,9,10 so that may have contributed to its development in our patient because there was evidence of chondrocalcinosis of the right wrist, but not in previous episodes of arthritis at that level. In conclusion, the development of JA in the RS seems to be rather incidental, because it is not properly a joint manifestation of any of the entities that make up this syndrome.
Please cite this article as: Sifuentes Giraldo WA, Grandal Platero M, de la Puente Bujidos C. Artropatía de Jaccoud asociada a síndrome de Reynolds. Reumatol Clin. 2014;10:103–131.