Osteopoikilia, also referred to as osteopoikilosis, is an asymptomatic osteosclerosing dysplasia, of non-specific etiology first described by Albers-Shonberg.1 We report the case of a 49-year-old patient in whom osteopoikilosis affected both femurs, the pelvis and spine. To the best of our knowledge, spinal localization was exceptional.2 The diagnosis was made by chance when reviewing lumbar spine X-rays.
Clinical CaseThe patient was a 49-year-old woman with a history of: degenerative L5-S1 disk disease, who underwent total disk replacement with a prosthesis, and secondary facet syndrome. She was seen in the clinic due to back pain, which was secondary to mechanical disk disease. General analysis showed calcium 9.8mg/dl (8.5–10.5), phosphorus 3.2mg/dl (2.5–4.8), alkaline phosphatase 102U/l (35–104), intact PTH 22pg/ml (12–65) and vitamin D (25-0H) 57.50ng/ml (≥30).
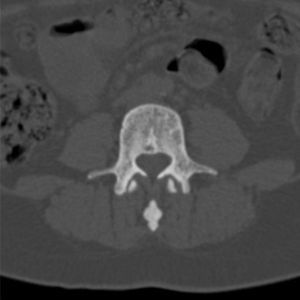
A routine X-ray of the lumbar spine (Fig. 1) showed many small, well-defined, homogeneous, circular areas of increased bone density in the vertebral bodies and throughout the axial skeleton we observed similar foci, which therefore led us to ask for AP pelvic X-rays (Fig. 2) and a CT of the pelvis and lumbar spine (Figs. 3 and 4), which showed radiodense round or oval lesions on the femoral head, neck, and the trochanteric regions, with the presence of small areas of increased density in the pelvis and the vertebral bodies suggesting, as a first diagnosis, osteopoikilosis. No soft tissue component or fractures in the areas of the cortex were seen, nor was the presence of periosteal reactions observed.
To rule out other processes, a bone biopsy of the iliac crest bone was performed which was normal, with large, wide, trabeculae, and connecting to each other. X-ray images highly indicative of osteopoikilosis and the normality of laboratory investigations, including bone biopsy, led us to the diagnosis of osteopoikilosis.
DiscussionOsteopoikilosis is a rare bone disease,2 with a prevalence of about one in 50000 patients3,4 consisting of a bone dysplasia with multiple radiodense foci located in the trabecular bone.5,6 It is more common in men and familial cases have been described, with autosomal dominant inheritance.5,6 It is described as a genetic mutation in the LEMD3 gene.4,7 It is clinically asymptomatic. The most common locations of occurrence seen are the carpal and metacarpal phalanges, the phalanges of the foot, metatarsals, tarsus, pelvis, femur, sacrum, humerus, and tibia. The involvement of the ribs, clavicles, spine, and skull is uncommon.5,8,9 Sometimes it may be associated with papular, yellowish or white, round or oval skin lesions, located on the lower back, buttocks, arms, and thighs, with certain symmetry (dermatolenticular disseminated fibrosis), something called the Buschke–Ollendorff syndrome or osteodermatopoikilosis.5 The diagnosis is radiological because the image is very indicative, characterized by foci of sclerosis, rarely over 10mm, without affecting cortical bone. Bone scans shows no pathological data, which is very useful in making the differential diagnosis with other osteocondensing lesions.5,9 Histologically, there is an increase in the number and thickness of the trabeculae of the spongy bone5,6,8 as in our case.
The differential diagnosis includes osteoblastic bone metastases, mastocytosis, tuberous sclerosis, striated osteopathy, melorheostosis, osteopetrosis, sclerosteosis, Erdheim–Chester disease or fluorosis.7,10
Ethical ResponsibilitiesProtection of people and animalsThe authors declare that procedures conformed to the ethical standards of the committee responsible for human experimentation and in accordance with the World Medical Association and the Declaration of Helsinki.
Data confidentialityThe authors declare that they have followed the protocols of their workplace regarding the publication of data from patients and that all patients included in the study have received sufficient information and have given their written informed consent to participate in the study.
Right to privacy and informed consentThe authors have obtained informed consent from patients and/or subjects referred to in the article. This document is in the possession of the corresponding author.
Conflict of InterestThe authors declare no conflicts of interest.
Please cite this article as: Pérez Ruiz J, Salman Monte TC, Blanch-Rubiò J, Campillo Ibáñez MÁ, Carbonell i Abellò J. Osteopoiquilia con afectación de la columna vertebral, una presentación atípica. Reumatol Clin. 2014;10:127–129.