To describe the prevalence of non-alcoholic fatty liver disease (NAFLD), the association between FIB4 and ultrasound findings, and the clinical characteristics of psoriatic arthritis patients.
Material and methodsWe carried out an observational cross-sectional study of patients seen in the outpatient clinic from January 1st, 2020, to November 30th, 2020, with psoriatic arthritis.
ResultsOf the 90 patients studied, the prevalence of NAFLD was 56.67%. FIB4 presents an association with ultrasound findings (p = .030), the absence of enthesitis (p = .036), and longer duration of disease (Rho .213 p = .042). It also presents an association with hypertension (p = .027) and alcohol consumption (p = .021). However, biological treatment can be considered as a protective factor (p = .005). FIB4 acts as a NAFLD predictor with 69.2% sensitivity and 70.4% specificity.
ConclusionsThe prevalence of NAFLD was higher in our sample than in the standard population. FIB4 index may be useful in screening for silent liver damage in psoriatic arthritis in clinical practice.
Describir la prevalencia de la enfermedad del hígado graso no alcohólico (EHGNA), la asociación entre FIB4 y los hallazgos en la ecografía y las características clínicas de los pacientes con artritis psoriásica.
Material y métodosEstudio transversal observacional de todos los pacientes con artritis psoriásica vistos de forma consecutiva en consulta desde 01/01/2020 hasta el 30/11/2020.
ResultadosDe los 90 pacientes estudiados la prevalencia de EHGNA fue de 56,67%. EL FIB4 presenta asociación con la ecografía (p = 0.030), la ausencia de entesitis (p = 0.036) y la mayor duración de la enfermedad (Rho 0.213 p = 0.042). También con la presencia de hipertensión (p = 0.027) y el consumo de alcohol (p = 0.021). Sin embargo, el tratamiento biológico puede considerarse como un factor protector (p = 0.005). El FIB4 actúa como predictor de EHGNA con una sensibilidad 69.2% y especificidad 70.4%.
ConclusionesLa prevalencia de EHGNA fue superior a la población general. El índice FIB4 puede ser una herramienta válida en el despistaje de EHGNA en nuestra práctica clínica diaria.
Psoriatic arthritis is a chronic inflammatory disease included in the spectrum of psoriatic disease and its prognosis is conditioned by the evolution of the disease itself and the comorbidity that these patients present.
Among the associated comorbidities, non-alcoholic fatty liver disease (NAFLD) stands out for its prevalence. It is the most common hepatic pathology in the world and is defined as the accumulation of lipids in hepatocytes leading to their death and an increase in inflammatory processes. NAFLD is linked to the appearance of other comorbidities such as metabolic syndrome, insulin resistance, obesity and alterations in lipid metabolism.1,2
Liver biopsy is the diagnostic test of certainty, but due to its high prevalence, invasiveness and high cost, it is necessary to validate non-invasive techniques that can help predict patients at increased risk. The acronym FIB-4 is a term that stands for FIBROSIS estimated with 4 simple elements.3 It was proposed as a method to help determine the amount of fibrosis in the liver of patients with concomitant HIV and HCV infection.
The primary objective was to describe the prevalence of NAFLD in patients with psoriatic arthritis, secondly to find the correlation between FIB4 and ultrasound findings and finally to analyse the association of FIB4 with the clinical characteristics of the patients.
Material and methodsA cross-sectional observational study was conducted in patients from a regional psoriatic arthritis registry (SUEIRO registry), successively and with prior acceptance from 01 January 2020 to 30 June 2022.
Inclusion criteria included being >18 years of age, accepting to participate voluntarily, having undergone an ultrasound scan and not presenting alcohol consumption or other causes of liver pathology (metabolic, viral). The permitted alcohol consumption for men was <28IU/week and for women <17IU/week. Exclusion criteria were therefore considered to be <18 years of age, not signing the informed consent form or presenting a cause of chronic liver disease.
Patient characteristics assessed were age, sex, weight (kg), BMI (kg/m2), hypertension (HT), type 2 diabetes mellitus (DM2) and dyslipidaemia (DL). For disease data we considered the type of involvement (axial, peripheral and mixed), extra-articular involvement (skin and nail psoriasis, uveitis, inflammatory bowel disease, enthesitis and dactylitis), disease duration and remission. Treatment received has included non-steroidal anti-inflammatory drugs, corticosteroids, leflunomide, methotrexate and biologic drugs (Infliximab, Adalimumab, Etanercept, Golimumab, Certolizumab, Ustekinumab, Secukinumab, Ixekizumab).
The FIB4 index includes 4 variables: age, two liver enzymes called transaminases: ALT and AST and platelet count and was performed using the specific calculator (https://www.hepatitisc.uw.edu/page/clinical-calculators/fib-4) categorising the results as <1.45 low risk: 1.45–3.25 intermediate risk; >3.25 high risk of advanced fibrosis.
Statistical analysis was performed using SPSS v21. Demographic variables were calculated using descriptive methods. Categorical variables were expressed as absolute numbers and percentages, while quantitative variables were expressed as arithmetic mean and standard deviation. The association between variables was determined by bivariate analysis.
For categorical variables, the Chi-Square test was used, and if not within its assumptions, Fisher's Exact test was used. For continuous variables, the Student's t-test was used to compare means or, if the variables did not conform to normality, the Mann–Whitney U test, Spearman's test was used to analyse the correlation between continuous variables, and finally, multiple linear regression analysis was carried out.
ResultsA total of 90 patients were analysed, 51 patients had ultrasound abnormalities, which in our sample represents a prevalence of NASH of 56.67%. Among these ultrasonographic alterations, we obtained 41 cases of steatosis (45.6%), 9 cases of steatohepatitis (10%) and 1 case of cirrhosis (1.1%). Table 1 shows the remaining epidemiological characteristics.
Descriptive analysis of the demographic variables.
| Demographic variables | N = 90 |
| Sex (male vs female) | 57 (63,3%) vs 33 (36,7%) |
| Age (years) | 62,55 +/− 13,4 |
| Weight (kg) | 85,65 +/− 18,46 |
| BMI (kg/m2) | 31,18 +/− 5,4 |
| HBP | 53 (58,9%) |
| DM2 | 23 (25,6%) |
| DL | 42 (46,7%) |
| Duration of the disease (months) | 174,7 (+/−105) |
| Type of APS condition | |
| Axial | 5 (5,6%) |
| Peripheral | 69 (76,7%) |
| Mixed | 16 (17,8%) |
| Psoriasis | 75 (83,3%) |
| Psoriatic onychopathy | 15 (16,7%) |
| Uveitis | 2 (2,2%) |
| Enthesitis | 29 (43,3%) |
| Dactylitis | 10 (11,1%) |
| Inflammatory bowel disease | 0 (0%) |
| Remission | 18 (20%) |
| DAPSA | 10,13 (+/−7,17) |
| BASDAI | 5,1 (+/−1,94) |
| Biological treatment | 52 (57,8%) |
| Methrotexate | 38 (42,2%) |
| Leflunomide | 5 (5,2%) |
| Alcohol consumption (yes vs no) | 18 (20%) vs 72 (80%) |
| Ultrasound | |
| Steatosis | 41 (45,6%) |
| Steatohepatitis | 9 (10%) |
| Cirrhosis | 1 (1,1%) |
| FIB4 | 1,67 (+/−1,013) |
| Low risk of fibrosis | 52 (57,8%) |
| Moderate risk of fibrosis | 30 (33,3%) |
| High risk of fibrosis | 8 (8,9%) |
A mean FIB4 of 1.67 (+/−1.013) was determined, distributed as 52 of our patients (57.8%) had a low risk of fibrosis, 30 (33.3%) a moderate risk and 8 of them (8.9%) a high risk of fibrosis. In bivariate analysis, FIB4 was associated with ultrasound (p = .030).
Regarding the association between FIB4 and the characteristics of our patients, we found an association with the absence of enthesitis (p = .036) and longer disease duration (Rho 0.213 p = .042), with higher FIB4 values in those patients with a higher number of enthesitis and longer disease duration. Also, with presence of hypertension, (p = .027) and alcohol consumption, (p = .021). As for biologic therapy, those patients on biologic therapy had lower FIB4 levels (p = .005) and therefore this therapy could be considered a protective factor (Table 2).
Relationship between FIB4 and ultrasound and clinical characteristics of the patients. Bivariate analysis.
| NAFLD ultrasound* | Absence of enthesitis* | Longer duration of illness** | Presence of HBP* | Consumption of alcohol* | No biological therapy* | |
|---|---|---|---|---|---|---|
| MAYOR FIB4 | 2.6 (1.3−3.6) vs 1.2 (.9−1.7), p = .003 | 1.4 (1.1−2.3) vs 1.2 (.8−1.7), p = .036 | Rho 0.213 p = .042 | 1.5 (1.1−2.3) vs 1.2 (.9−1.4), p = .027 | 1.9 (1.2−3.5) vs 1.3 (.9−1.7), p = .021 | 1.7 (1.2−2.3) vs 1.1 (.9−1.7), p = .005 |
No association was found between FIB4 and sex (p = .106), type of psoriatic arthritis involvement (p = .633), presence of psoriatic skin involvement (p = .594), uveitis (p = .841), dactylitis (p = . 980), onychopathy (p = .847), disease remission (p = .881), DAPSA (Rho 0.054, p = .670), methotrexate (p = .974), leflunomide (p = .587), BMI (Rho 0.010, p = .931), DL (p = .259) and DM2 (p = .089). Stratification by BMI score showed that 11.4% of patients had a BMI < 25; 34.2% had a BMI between 25–30; and 54.4% of patients had a BMI > 30, which was not significant (p = .850). The mean BMI in patients with steatosis was 31.4 ± 5.35 and in patients with steatohepatitis 33.20 ± 6.4.
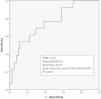
FIB4 acts as a predictor of NAFLD with a sensitivity of 69.2% and specificity of 70.4% with an area under the curve of 0.758 (95% CI 0.619−0.897) (Fig. 1).
A multiple linear regression analysis was performed including the variables biological treatment (including the different biological treatments) and the other therapies, HTN, ultrasound findings, enthesitis and DM2.4 In this study we found no significant association between these variables and the FIB result. In our study MTX had a p = .407; and LFN p = .886.
Binary regression analysis showed an association between steatohepatitis and FIB4 with a p = .044 and an OR of 2.517 (95%CI 1.023–6.190), independent of the presence of obesity (p = .224).
DiscussionIdentification of individuals with PsA and liver comorbidity is essential, especially considering the prevalence and associated morbidity and mortality. The prevalence of NASH in patients with psoriatic arthritis is higher than in the general population, varying according to demographic factors and influenced by independent factors such as joint and skin disease activity, ranging from 32% to 44%, higher in our sample.4,5
The FIB4 index is a non-invasive index easily accessible in daily clinical practice with a high negative predictive value and a sensitivity of almost 90%. Like FIB4, the use of these non-invasive methods to assess the risk of liver fibrosis is becoming increasingly widespread, but there are no protocols for their use in inflammatory arthritis, although their study and active search is increasing.6–8 The FIB4 results obtained in this study are associated with ultrasound findings and show that almost half of the patients analysed have a moderate/high risk of liver fibrosis. Among the intrinsic factors of the disease, we found an association with the absence of enthesitis and the duration of the disease, and biologic therapy as a protector. Extrinsic factors include high blood pressure.
Several studies indicate that the presence of hypertension or pre-hypertension causes a higher probability of NAFLD compared to normotensive patients, even in the absence of other metabolic risk factors. Furthermore, the development of HTN is associated with the progression of NAFLD.9
Perhaps because we were dealing with a population sample with a high percentage of overweight and obesity, we were unable to find an association between BMI and the FIB index4. However, the association between BMI and NAFLD is well correlated in the literature.10–12 The relationship between diabetes mellitus and NAFLD is widely known, with some studies estimating the prevalence of fatty infiltration in 62.2% of patients with DM2 as measured by ultrasound. However, regarding the use of non-invasive methods, one study has found lower accuracy in Hepascore, FIB4 and APRI in diabetic versus non-diabetic patients.13
In our study, patients on biologic therapy showed a benefit in relation to FIB4 and liver fibrosis risk prediction. TNFa inhibitors, although early studies pointed to a potential effect on inflammation in the liver, the benefits are still unclear, although disease control may influence the hepatic benefit.14,15 Regarding IL12/23 blockade, the data in the literature are consistent with pivotal trials of the drug. The influence of the IL-17 pathway in the aetiopathogenesis of NAFLD is a field under study, and although blockade of this signalling pathway is a possible target, translated into benefit with therapies that block it, prospective studies with well-defined objectives are necessary to obtain conclusive results.
Prospective studies with a control group and a larger sample size could provide more evidence for the management of these patients in real clinical practice.
LimitationsObservational and cross-sectional nature of the study. Sample size. Furthermore, it would have been more appropriate to include a group of controls ("healthy") matched by age, sex and body mass index, as these three factors will have a significant influence on the development of NAFLD and therefore the prevalence can be modified. The absence of liver biopsy precludes a diagnosis of anatomopathological certainty.
ConclusionsThe prevalence of NAFLD in our series was 56.67%, higher than in the standard population. In our study, using FIB4, we found that almost half of the sample was at risk of fibrosis and this finding was associated with ultrasound findings. The absence of enthesitis, longer disease duration, the presence of hypertension and alcohol consumption were associated with higher FIB4 values, and biological treatment could be considered a protective factor.
The use of FIB4 can be a valid tool in screening for NAFLD, being easily accessible and implementable in our daily clinical practice and with high diagnostic value.
Authors’ contributionAll the authors contributed equally in the research.
FundingJanssen has offered support to make the registry viable and operational.
Conflicts of interests and ethical aspectsThere are no conflicts of interest in this article. The source registry with code 2015/671 is approved by committee and patients signed informed consent for inclusion.
The authors with to thank the Grupo de Investigación Gallego en Artritis Psoriasica and the Sociedad Gallega de Reumatología for their advice and review of the article.