Intramuscular myxomas are benign and rare tumors that affects predominantly the lower limbs. The association of myxomas and fibrous dysplasia, usually polyostotic, is rarer. This association is known as Mazabraud's syndrome, of which about 81 cases have been described in the literature. We present a new case of this uncommon association to emphasize the importance of recognizing this syndrome in the diagnosis and appropriate management of the patient.
Los mixomas intramusculares son tumores benignos y poco frecuentes, que se presentan predominantemente en los miembros inferiores. Más infrecuente es la asociación de mixomas y de displasia fibrosa, generalmente poliostótica. Esta asociación se conoce como síndrome de Mazabraud, de la que se han descrito aproximadamente 81 casos en la literatura. Presentamos un nuevo caso de esta rara asociación, para enfatizar la importancia de reconocer este síndrome en el diagnóstico y manejo adecuado del paciente.
Mazabraud's syndrome represents the uncommon combination of one or more intramuscular myxomas and fibrous dysplasia. Described for the first time by Henschen in 1926, it was Mazabraud who reported his second case in 1967, stressing its association with fibrous dysplasia.1 It is important to be familiar with this association, as it can differentiate a myxoma—a benign tumor—from malignant mesenchymal tumors with myxoid material, a difficult undertaking.2,3
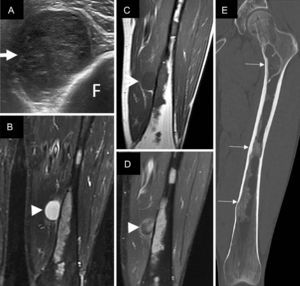
Clinical ObservationWe report the case of a 45-year-old man who presented with a hard, painless mass in the medial surface of his left thigh that had grown slowly in recent months. He was referred to our center with musculoskeletal ultrasound, which documented an intramuscular lesion, in the distal third of his left thigh, with well-defined borders, heterogeneous echogenicity and good posterior transmission (Fig. 1A). Magnetic resonance imaging (MRI) demonstrated a solid intramuscular mass measuring 3cm in the vastus medialis muscle; it was hypointense in T1-weighted sequences and hyperintense in T2, with no calcifications, and with a peripheral and patchy enhancement in its interior after the administration of intravenous gadolinium; another 1-cm intramuscular lesion was observed with characteristics similar to those of the image, in the left great adductor muscle, but it was not clinically palpable. In bone, with enhancement, we identified expansive diaphyseal intramedullary lesions in left femur and left tibia, consistent with fibrous dysplasia. Computed tomography (CT) of lower limbs showed the typical ground glass pattern of fibrous dysplasia (Fig. 1B–E).
(A) Axial image of left thigh ultrasound, showing an intramuscular soft tissue mass, that is hypoechoic and heterogenic (arrow), compatible with a solid lesion. (B–D) Coronal views from MRI of left thigh, showing the well-defined, markedly hyperintense, intramuscular mass in the STIR sequence (arrowhead in B), hypointense in T1 (arrow in C) and with heterogeneous enhancement after intravenous gadolinium administration in the T1 postcontrast sequence, with fat saturation (arrowhead in D), compatible with myxoma. Bone lesions can also be visualized in femur with diffuse enhancement after contrast administration. (E) Coronal CT view of femur with bone window, which shows the bone lesions with increased density, with a “ground glass” pattern typical of fibrous dysplasia (small arrows). CT, computed tomography; F, femur; MRI, magnetic resonance imaging; STIR, short tau inversion recovery.
The characteristics of the bone lesions were compatible with polyostotic fibrous dysplasia, and the coexistence with intramuscular soft tissue lesions were suggestive of Mazabraud's syndrome.
The larger intramuscular mass was removed surgically and pathology confirmed the diagnostic of myxoma in the smaller lesion.
DiscussionIntramuscular myxomas are soft tissue tumors that grow slowly, are generally painless, and tend to arise in patients with Mazabraud's syndrome in muscles near the bones most affected by the fibrous dysplasia. These tissues usually precede the development of the myxoma by years or even decades.3,4
A number of hypotheses have been proposed to explain Mazabraud's syndrome, including a common histological origin during embryonic development, and changes in early bone and soft tissue growth. Mutations have recently been identified in certain genes implicated in cell proliferation, including the GNAS gene (20q13.2-13.3).5
Myxomas have a high attenuation in CT, in which they appear to be cystic lesions. In MRI, they are characterized as hypointense intramuscular masses in T1-weighted images and hyperintense in T2, and are enhanced after the administration of a contrast medium. One can occasionally see a perilesional fat rind and edema in adjacent muscules.2,4
The treatment of myxomas consists of follow-up of the lesion and/or local resection of the tumor in symptomatic or growing lesions. In our patient, we resected the larger mass and decided on conservative management of the second tumor.
ConclusionsMazabraud's syndrome is an uncommon association that should be taken into account in patients with soft tissue tumors and fibrous dysplasia. Awareness of this syndrome may help in establishing a correct preoperative diagnosis, and reduce the need for unnecessary biopsies or surgical measures.
Ethical DisclosuresProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this investigation.
Confidentiality of dataThe authors declare that they have followed the protocols of their work center on the publication of patient data.
Right to privacy and informed consentThe authors must have obtained the informed consent of the patients and/or subjects mentioned in the article. The author for correspondence must be in possession of this document.
Conflicts of InterestThe authors declare they have no conflicts of interest.
Please cite this article as: Ramírez Mejía AR, Moreno Casado MJ, Ahumada Pavez NR, Rojas Soldado MÁ. Síndrome de Mazabraud. Nuevo caso clínico y revisión de los hallazgos. Reumatol Clin. 2016;12:336–338.