Melorheostosis is also known as hyperostotic osteopathy, monomyelic eburnating osteitis or Leri and Joanny disease. It is a rare mesenchymal bone disease classified as a sclerotic bone dysplasia (Fair-Bank, 1951). It was initially described by Leri and Joanny (Leri–Joanny 1922),1 and affects males and females equally, with a prevalence of 0.9 per millón.2 We present the case of a 42 year old male with a history on pain for several months on the left leg, diagnosed with localized melorheostosis in the mid-third of the tibia and peroneus.
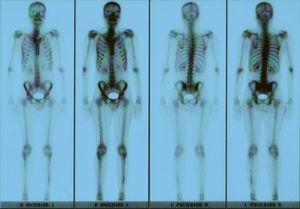
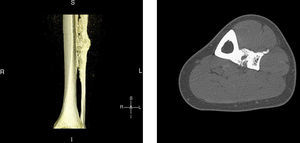
Clinical presentationA 42-year-old male with no prior history presented 3 months prior to his coming to our department with continuous pain in the middle third of the left leg. Upon examination there was selective pain on palpation on the mid third of the left tibia. No skin atrophy or deformity of the affected limb was detected. Laboratory analysis, including acute phase reactants, complete blood count, blood chemistry, bone remodeling markers in blood and urine, thyroid hormone and proteins, were normal. A simple X-ray of the left leg (Fig. 1) presented an image of hyperostosis with a thickened cortex on the mid third of the tibia and peroneus, extending along the bone and showing a “dripping candlewax” image. A bone scan with 99Tc (Fig. 2) observed an increase in uptake. A computerized tomography (Fig. 3a and b), showed dense cortical hyperostosis of the distal half of the tibial and peroneal diaphysis, with wavy and exhuberant borders, cortical sclerosis and periostic and endostic thickening, predominantly on the lateral tibia and mid peroneal, with a “dripping candlewax” aspect, suggestive of melorheostosis.
3D sagittal reconstruction, computerized tomography of the left leg: the distal half of the tibial and peroneal diaphysis shows dense cortical hyperostosis with wavy and exhuberant borders and associated periosteal and endosteal thickening, predominantly on the lateral tibia and medial fibula, giving an image of “dripping candlewax”, suggestive of melorheostosis.
To rule out malignancy or processes other than melorheostosis, a tibia biopsy was performed. Microbiological cultures of the sample were negative for aerobes, anaerobes and typical and atypical mycobacteria, as well as fungi. The patient was treated with analgesics and NSAIDs, and the pain disappeared within days of starting treatment. The patient has been monitored with tomography, showing no significant changes in the images so far.
DiscussionWe present this case because of the low incidence of the disease and on differential diagnosis doubts raised with other processes such as osteomyelitis or tumors. When it affects long bones it is usually diagnosed by the characteristic “dripping candlewax” image. To safely differentiate from neoplastic or infectious processes, a bone biopsy and microbiological cultures of samples of affected tissue must be performed (although they are not required for the diagnosis of melorheostosis). The disease can occur at any age, although the incidence is higher in the second and third decades of life. In fact, in terms of age of onset, in some series up to 50% of cases of the disease appear before 20.3 It may be asymptomatic for a long time, but the most common clinical manifestations are: (a) sclerotic changes confined to an extremity; (b) altered contour of the affected bone and even permanent development of genu varus or valgus deformities of the lower limbs; (c) pain, which is often intense, and (d) limitation of motion in joints formed by the affected bone. Alteration of skin pigmentation in the affected area is unusual, but in some cases sclerodermatous linear lesions appear (some authors have called linear scleroderma melorheostic) and skin changes seem to be representative of the proliferative disorder that causes hyperostosis. The presentation in the axial skeleton is rare but may be accompanied by severe nerve4 root involvement. The condition may be monostotic or polyostotic,5 affecting one or more bones of the limb, and the disorder affects the lower limbs more frequently, starting proximally and moving distally. The lower extremities are affected more often than the upper ones.6 Although rare, it may be associated with renal (artery stenosis), and vascular abnormalities (hemangiomas, arteriovenous malformations, aneurysms, varicose veins), lymphatic system disorders (lymphedema, lymphangiectasia) and tumors (lipomatous and desmoid tumors). Its etiology is uncertain (it is hypothesized that these alterations are a result of the same disorder, as vascular mesenchymal dysplasia). Recent studies suggest that it may be due to a mutation in the LEMD3 gene, which encodes a nuclear membrane protein involved in Smad signaling system. This mutation is also involved in the pathogenesis of osteopoikilosis and Buschke-Ollendorff syndrome (an autosomal dominant disorder that presents clinically with elastic nevi and osteopoikilosis).7 The diagnosis is usually performed by imaging techniques (radiography, CT, MRI and bone scans). When it affects the long bones it is typically characterized by a “dripping candlewax”8 image. A bone scan may help differentiate melorheostosis from other processes, such as osteopoikilosis and striated osteopathy, in which there is no increase in uptake. Laboratory tests showed normal levels of calcium, phosphorus and bone alkaline phosphatase. The differential diagnosis must include entities such as osteopetrosis, osteopoikilosis, striated osteopathy, infantile cortical hyperostosis and osteomas. The disease is a benign entity with a generally chronic course and periods of exacerbation and remission. There is no specific treatment. Therapy is symptomatic and aimed at controlling bone pain.9 In some cases, good results were obtained with infusions of pamidronate.10 In cases with significant bone deformity or soft tissue involvement, corrective surgical treatment may be appropriate.
Please cite this article as: Salman Monte TC, et al. Melorreostosis: presentación de un caso y revisión de la literatura. Reumatol Clin. 2011. doi:10.1016/j.reuma.2010.11.007.