Describe patients with noninfectious aortitis and their response to treatment in a regional hospital.
MethodsReview of patients with noninfectious aortitis, diagnostic technique used and immunosuppressive therapy received.
ResultsWe report 8 patients (7 women and one man) diagnosed with aortitis by positron emission tomography (PET). The mean age was 69 years (interquartile range [IQR] 62–72.2). Three months of treatment with tocilizumab improved symptoms, erythrocyte sedimentation rate and C-reactive protein level (P<.001 and P<.012, respectively) in the 6 patients in whom it was used.
ConclusionsTocilizumab was an effective and safe treatment in those patients diagnosed with aortitis refractory to steroids and conventional immunosuppressive therapy.
Describir pacientes con aortitis no infecciosa y su respuesta al tratamiento de un hospital comarcal.
MétodosRevisión de pacientes con aortitis no infecciosa, técnica diagnóstica utilizada y tratamiento inmunosupresor recibido.
ResultadosSe encontraron 8 pacientes (7 mujeres y un hombre) diagnosticados de aortitis mediante tomografía por emisión de positrones (PET). La mediana de edad fue de 69 años (IQR 62-72,2). Tocilizumab (TCZ) mejoró los síntomas, la VSG y la PCR a los 3 meses del tratamiento (p<0,001 y p<0,012, respectivamente) en los 6 pacientes en que se utilizó.
ConclusiónTCZ fue eficaz y seguro en los pacientes que fueron refractarios a esteroides y a otros tratamientos inmunosupresores.
Non-infectious aortitis is a rare entity which often remains undetected. Symptoms may be highly varied from headaches or typical symptoms of rheumatic polymyalgia (RPM) to other less common symptoms including dyspnoea, fever, and claudication in lower limbs. On occasions it may be observed within the context of a recognized great blood vessel (giant cell arteritis [GCA] or Takayasu's disease), associated with a systemic disease (essentially an IgG4 related disease) in isolation or associated with RPM. As a result, these possibilities have to be considered for the administration of appropriate treatment.
It is often the case that immunosuppresive treatment with steroids, methotrexate or azatioprine is insufficient, and this obliges us to seek new therapeutic options. In this study we present our experience in a regional hospital.
Material and methodsA retrospective search of patients diagnosed with non-infectious aortitis was made during the years 2010–2016 and the following data were collected: age, sex, initial symptoms on diagnosis, temporal artery biopsy, diagnostic technique used, time from onset of symptoms to diagnosis made by positron emission tomography (PET), time elapsed to the initiation of tocilizumab (TCZ) in patients considered refractory to standard treatment with steroids and immunosuppressive drugs, and final drug dose. An initial recording of erythrocyte sedimentation rate (ESR)/C reactive protein (CRP) level was made and 3 months after remission was achieved. Remission was defined as an improvement in clinical symptoms and normalization of ESR and CRP.
Statistical analysisThe description of the quantitative variables was made using the median and the interquartile range (IQR) and the comparison of variables was carried out with the Wilcoxon test.
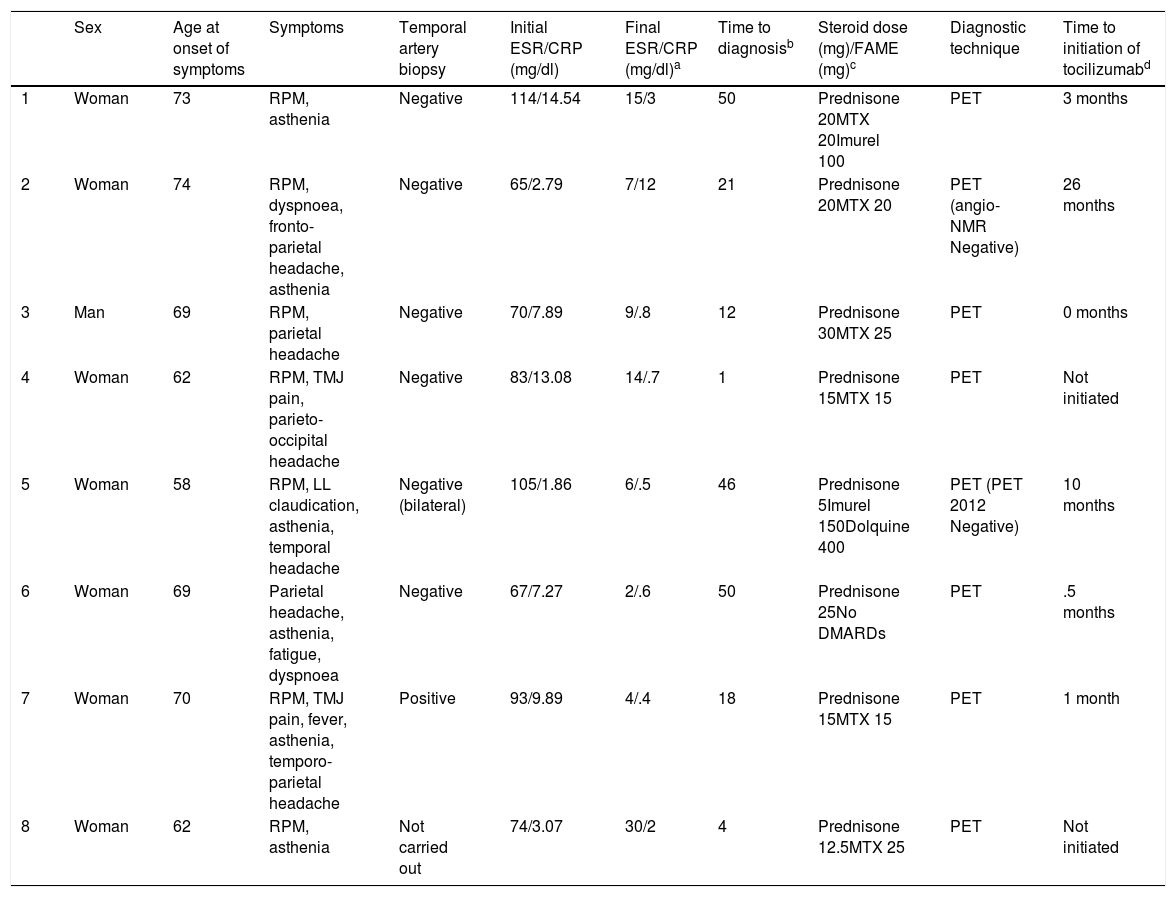
ResultsWe found 8 patients: 7 women and one man. The mean age of presentation was 69 years (IQR 62–72.2). The most common clinical symptom at onset was RPM, headache and asthenia. Six of the 8 patients presented with parietal headache or parieto-occipital headache of recent onset. All except patient 8 underwent a temporal artery biopsy (Table 1). In patient 5 the bilateral temporal artery biopsy tested negative. Out of all of the patients, only patient 7 tested positive. The ESR median at onset and end was 78.5 (IQR 67.7–102) and 10.9 (IQR 4.5–14.7), respectively (P<.001) and the median of the CRP (mg/dl) at onset and at the end was 7.6 (IQR 2.9–12.3) and .7 (IQR .5–1.8), respectively (P<.012). The median of delayed diagnosis was 19.5 (IQR 6–49) months. The median steroid dose where a resurgence of symptoms was observed was of 17.5mg (IQR 13.1–23.7) days of prednisone. All the patients except patient 6 received concomitant treatment with disease-modifying anti-rheumatic drugs (DMARDs). Methotrexate was used in all patients except patient 6 to a maximum dose of 25mg weekly. Patients 1 and 5 were also treated with azatioprine at doses of 100 and 150mg daily, respectively. The final diagnostic test was the PET. In patient 2 the PET was compatible with aortitis, and the angiographic magnetic resonance (angio-MR) was negative. The median time from diagnosis of the disease to treatment initiation with TCZ was 2 months (IQR .4–14). Of the 8 patients in this series, 6 required treatment with TCZ.
Patient characteristics.
| Sex | Age at onset of symptoms | Symptoms | Temporal artery biopsy | Initial ESR/CRP (mg/dl) | Final ESR/CRP (mg/dl)a | Time to diagnosisb | Steroid dose (mg)/FAME (mg)c | Diagnostic technique | Time to initiation of tocilizumabd | |
|---|---|---|---|---|---|---|---|---|---|---|
| 1 | Woman | 73 | RPM, asthenia | Negative | 114/14.54 | 15/3 | 50 | Prednisone 20MTX 20Imurel 100 | PET | 3 months |
| 2 | Woman | 74 | RPM, dyspnoea, fronto-parietal headache, asthenia | Negative | 65/2.79 | 7/12 | 21 | Prednisone 20MTX 20 | PET (angio-NMR Negative) | 26 months |
| 3 | Man | 69 | RPM, parietal headache | Negative | 70/7.89 | 9/.8 | 12 | Prednisone 30MTX 25 | PET | 0 months |
| 4 | Woman | 62 | RPM, TMJ pain, parieto-occipital headache | Negative | 83/13.08 | 14/.7 | 1 | Prednisone 15MTX 15 | PET | Not initiated |
| 5 | Woman | 58 | RPM, LL claudication, asthenia, temporal headache | Negative (bilateral) | 105/1.86 | 6/.5 | 46 | Prednisone 5Imurel 150Dolquine 400 | PET (PET 2012 Negative) | 10 months |
| 6 | Woman | 69 | Parietal headache, asthenia, fatigue, dyspnoea | Negative | 67/7.27 | 2/.6 | 50 | Prednisone 25No DMARDs | PET | .5 months |
| 7 | Woman | 70 | RPM, TMJ pain, fever, asthenia, temporo-parietal headache | Positive | 93/9.89 | 4/.4 | 18 | Prednisone 15MTX 15 | PET | 1 month |
| 8 | Woman | 62 | RPM, asthenia | Not carried out | 74/3.07 | 30/2 | 4 | Prednisone 12.5MTX 25 | PET | Not initiated |
TMJ: temporomandibular joint; LL: lower limbs; DMARDs: disease-modifying drugs; MTX: methotrexate; PET: positron emission tomography; RPM: rheumatic polymyalgia.
Patients 4and 8 did not start treatment with TCZ: patient 4 due to complications (bilateral pulmonary thromboembolism) and 8 due to being controlled with methotrexate and prednisone. Treatment with TCZ was suspended in patients 1 and 2 due to major improvement after 6 months, but had to be re-established due to a worsening of clinical symptoms and analytical tests and to the PET results, with good posterior control. There were no secondary adverse effects to the use of TCZ.
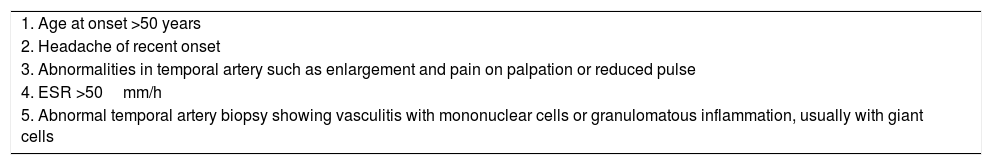
DiscussionIn this review, 7 out of 8 patients presented with clinical symptoms of RPM, with ESR over 50mm/h and aged over 50. Six of them had concomitant headaches, which led to them meeting three criteria, sufficient, according to the American College of Rheumatology (ACR) of 1990, for the diagnosis of GCA,1 although only one of them (patient 7) tested positive in the temporal artery biopsy (Table 2). Since it is known that in the GCA there exists the possibility of involvement of great supraaortic vessels and the aorta itself, demonstration of aortis by PET enabled us to consider the diagnosis in all of our cases, ruling out the possibility of overlapping with non-infectious idiopathic aortis or aortis associated with other processes.2 Due to all of the above we deduced there remained a need for updating GCA criteria of the ACR to adjust the sensitivity and specificity of current diagnostic resources.2–4
Classification criteria of giant cell arteritis (GCA) from the American College of Rheumatology (ACR) 1990.
| 1. Age at onset >50 years |
| 2. Headache of recent onset |
| 3. Abnormalities in temporal artery such as enlargement and pain on palpation or reduced pulse |
| 4. ESR >50mm/h |
| 5. Abnormal temporal artery biopsy showing vasculitis with mononuclear cells or granulomatous inflammation, usually with giant cells |
EST: erythrocyte sedimentation rate.
The presence of three of more of the five criteria accounts for the diagnosis of GCA.
PET appears to be a good tool for diagnosis, especially in the very initial stages of the disease, to assess response to treatment and/or disease recurrence.5 Several studies suggest, given its specificity and predictive positive value, that it is superior to CT and angio-MR.6,7 However, it remains unclear how useful it is in long-term follow-up of the disease activities, which in several cases, despite observing clinical and analytical improvement, metabolic activity continues to be present.5–7
TCZ has demonstrated its efficacy in GCA after results obtained from the GiACTA8 study. Studies have been published which demonstrate the efficacy of TCZ in non-infectious aortitis even when other biological therapies have been attempted previously, such as the anti-tumour necrosis factor alpha (antiTNF-α).9 Treatment with antiTNF-α has been used in an attempt to control remission maintenance induced by steroids in GCA, with poor results.10 In our series TCZ was a safe and effective treatment in the cases where it was administered.
ConclusionIn this series PET was the definitive diagnostic test for aortitis and GCA in all patients. Corticosteroids and conventional immunosuppressive treatment was insufficient for good control of the disease in the majority of patients. Treatment with TCZ was effective and safe in this series of patients when non-infectious aortitis refractory to treatment with corticosteroids and DMARDs.
Conflict of interestsThe authors have no conflict of interests to declare.
Please cite this article as: Aldasoro Cáceres V, Ibáñez Bosch R, Rivas Zavaleta N, Álvarez Rodríguez B, Intxausti Irazábal JJ, Jiménez de Aberasturi JRD, et al. Aortitis no infecciosa: experiencia con tocilizumab en un hospital comarcal. Reumatol Clin. 2019;15:e96–e98.