To determine and analyse the organisational approach adopted by Spanish rheumatologists to osteoporosis (OP) to define strategic priorities.
Material and methodA group of experts designed a questionnaire on OP in the rheumatologist practice. The survey was sent to the Spanish Society of Rheumatology (SER) members. Through the Delphi round, strategic priorities were agreed upon in OP.
ResultsThe priorities are: 1) The SER should promote the inclusion of OP in 100% of the services and expand the training offer; 2) Rheumatology services should promote the role of the nurse in OP, promote quality indicators and referral protocols agreed with primary care in addition to promoting their training in this area; 3) The SER and Rheumatology services should promote electronic consultation, OP monographic clinics and participation in Fracture Liaison Service units.
ConclusionsStrategic priorities in OP help identify areas of improvement at organisational, structural and quality standards level in this pathology.
Los estudios de opinión sobre la percepción del reumatólogo de la práctica asistencial en osteoporosis (OP) pueden ayudar a identificar áreas de mejora en la gestión de esta patología.
ObjetivoConocer y analizar el enfoque organizativo que adoptan los reumatólogos españoles ante la OP para definir prioridades estratégicas y establecer unos estándares de calidad.
Material y métodoUn grupo de expertos diseñó una encuesta sobre creencias y conductas en OP en la práctica del reumatólogo. La encuesta se remitió a los socios de la Sociedad Española de Reumatología (SER). Mediante ronda Delphi se consensuaron las prioridades estratégicas en OP.
ResultadosEl grupo de expertos consensuó como prioridades estratégicas en OP: 1) La SER debería impulsar la inclusión de la OP en el conjunto de prestaciones de todos los servicios de reumatología, así como ampliar la oferta formativa específica para médicos y enfermeras; 2) Los servicios de reumatología debieran fomentar el papel de la enfermera en OP, impulsar la implantación y el seguimiento de indicadores de calidad e implantar protocolos de derivación consensuados con atención primaria además de impulsar su formación en este área; 3) La SER y los servicios de reumatología deberían impulsar la implantación de la consulta electrónica y la consulta monográfica o dedicada a OP así como la participación del reumatólogo en unidades de fractura Fracture Liaison Service (FLS).
ConclusionesLas prioridades estratégicas en OP derivadas de la encuesta a los reumatólogos españoles ayudan a identificar las áreas de mejora a nivel organizativo, estructural y de estándares de calidad en esta patología.
Osteoporosis (OP) is a common process in rheumatology consultations. A cross-sectional study conducted in the Community of Madrid, that studied the healthcare activity of 41 rheumatologists with data from a total of 2311 patients, showed that metabolic bone disease was the most frequent reason for consultation, 19.7% of consultations, ahead of peripheral osteoarthritis (16%) and soft tissue disease (14%).1
In 2010, an estimated 21% of women and 5% of men>50 years of age in Spain suffered from OP.2 The care process for postmenopausal OP generally starts in primary care (PC), and some cases are referred to specialist care.
Concern about OP, both in the healthcare setting and in the population, leads to the frequent use of diagnostic tests and treatments; it is a major healthcare problem that needs to be improved.
The high prevalence of OP, the complexity of its management due to the many professionals involved and the importance of the role of the rheumatologist as the leader of this process, prompted this improvement group that set out to study current the clinical management of OP by rheumatology specialists. Opinion studies on the perception of rheumatologists can be a good method for detecting healthcare problems and identifying areas for improvement in clinical management and quality of care for these patients by consensus.3 Along the same lines, consensus documents seek to reach agreement on controversial issues such as, in this case, the management of OP by rheumatologists.4
The aim of this study, therefore, was to identify and analyse the organisational and clinical approach adopted by rheumatologists in the management of OP in Spain to define strategic lines and priorities and establish a list of quality indicators and standards to enable better management and continuous improvement in the care of OP and its complications.
Material and methodThe study design was qualitative and quantitative, and the approach was based on the consensus technique. The project was conducted between September 2017 and December 2018 with a mixed method, in 2 stages, combining a qualitative and quantitative approach.5
Qualitative research is considered particularly appropriate in the exploratory phase of a project; through it an in-depth understanding can be gained of individual experiences, opinions and beliefs associated with an object of study.6 To this end, a focus group was held with rheumatology experts who raised key issues in the care of the OP patient. The expert rheumatology opinion was based on more than 15 years’ clinical experience in the care and management of consultations, including OP.
The qualitative phase, given its inductive nature and limited representativeness, justifies a second quantitative phase to measure and weigh up the facts. In this second phase, data were collected from a sample of professionals through a self-administered online survey on the aspects previously identified by the experts. Since the ultimate aim of the work was to define strategic lines of action, a Delphi round was then conducted with the group of experts who prioritised the decisions to be taken. In total, 2 Delphi rounds were performed via e-mail.
Qualitative investigationThe qualitative phase consisted of a focus group in which 7 rheumatology specialists participated with a moderator. The aim was to gather extensive information on the rheumatologist's care practice in relation to OP, their perception of this disease and the organisation of care. A working guide was designed with various questions and subject areas: a) patient origin, b) patient care in PC, c) patient care in rheumatology, d) rheumatology consultation, e) continuity of care for patients with OP: report and follow-up, f) nursing and prevention programmes for patients with OP.
The session lasted 2 h, followed by a content analysis. The technique concluded with the identification of subjects of interest on the organisational and clinical approach adopted by rheumatologists to OP.
Quantitative researchThe quantitative phase consisted of the design, application and analysis of the data from a survey sent by email to rheumatologists who are members of the Spanish Society of Rheumatology (SER), with the aim of gathering information to provide a global, guiding and, as far as possible, representative vision of the clinical and care practice of the rheumatologist in primary OP, which would be postmenopausal OP with or without fracture, secondary OP (associated with other metabolic or inflammatory diseases, glucocorticoids, hypogonadism…) and fracture due to inflammation, or to the presence of other metabolic or inflammatory diseases. …) and fragility fracture.
A structured survey was designed with direct questions on usual practice and current beliefs regarding the most convenient needs and areas for improvement in relation to OP. Table 1 shows the subject areas of the survey.
List of the subject areas of the questionnaire.
| a) Volume, origin and characteristics of the patients seen for OP in the rheumatologist’s practice |
| b) Tests provided and quality of the referral of patients from primary care |
| c) Organisational and care aspects of OP in the rheumatologist’s practice: |
| access to bone density scan |
| characteristics of the patient attended |
| existence of protocols |
| existence of specialist clinics |
| existence of fracture units |
| d) Quality Management in OP: |
| quality indicators and standards |
| characteristics of the medical report |
| existence of functional and quality of life questionnaires in OP |
| e) Nursing care and prevention programmes |
| f) Expectations and areas for improvement |
A Likert-5 response format was used where 1 indicated minimum agreement or frequency and 5 indicated maximum agreement or frequency. The survey was prepared in collaboration with a group of 6 rheumatologists whose practice was not exclusive to OP. After a process of revision and refinement, the final survey comprised 24 questions (Appendix B Annex 1 additional material). The online data collection format was chosen through the SER, and disseminated to its members between September and December 2017.
The survey results are presented using descriptive statistics, mean, median and standard deviation and principal component factor analysis.
Decision phase: DelphiFollowing the methodology described by Linstone and Turoff in 1975, the group of experts was reconvened in a controlled communication format that avoided direct confrontation between experts and consequent influence.6 A self-administered online form was designed based on the key results of the survey, in which each expert had to indicate the importance they attached to implementing each proposed measure. The final aim was to prioritise the areas for improvement in the care of OP patients and the body responsible for making this improvement, choosing between the SER, the rheumatology services or both. Finally, a list of strategic priorities in OP was drawn up.
The results are presented by means of descriptive statistics; mean, median and standard deviation.
Ethical aspects: The protocol did not require approval by an Ethics and/or Research Committee, as it was a non-clinical practice project approved by the corresponding commission of the SER and conducted under the auspices of the SER’s CRETA programme. The respondents did not sign an informed consent form for the same reason.
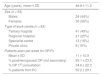
ResultsCharacteristics of the sample of rheumatologists who responded to the surveyThe response rate among SER members was 8%, with a sample of 108 surveys (84 valid responses) from rheumatologists spread over 22 provinces: Madrid (16.7%), Barcelona (14.8%), Alicante (7.4%) and Seville (7.4%) had the highest number of responses. Eighty-five percent of the respondents were in the 35–50 age range (Table 2). The sample mainly comprised doctors from tertiary hospitals (49%). Of the respondents, 90% were from the public sector and the average team size was 5 specialists.
Description of participating rheumatologists.
| Age (years), mean ± SD | 46.8 ± 11.2 |
|---|---|
| Sex (n = 54) | |
| Males | 24 (44%) |
| Females | 30 (56%) |
| Type of work centre (n = 83) | |
| Tertiary hospital | 41 (49%) |
| Regional hospital | 21 (25%) |
| Specialist centre | 13 (16%) |
| Private clinic | 8 (10%) |
| Patients seen per week for OP/Fx | |
| Mean ± SD | 11 ± 10.9 |
| % postmenopausal OP (not secondary) | 65.1 ± 23.5 |
| % OP 1st consultation | 34.6 ± 22.3 |
| % patients from PC | 50.2 ± 29.1 |
Fx: Fragility fracture; OP: Osteoporosis; PC: Primary Care; SD: Standard Deviation.
Care of OP is not included in the service package of 6% of the respondents.
The number of patients seen in a week for OP or fracture ranges from 6 to 15, 65% being postmenopausal women with no secondary causes of OP and 34% first visits. Rheumatologists believe that 42.7% (SD 25) of patients could have been treated in primary care alone. The specialties that most frequently refer to the rheumatologist were traumatology, PC, oncology and gynaecology. The main reasons for referral were, in this order: assessment of the results of bone density scans (DXA) and/or fragility fracture, assessment of OP due to glucocorticoids, assessment of OP in patients with chronic arthritis, treatment with aromatase inhibitors, concerns regarding the treatment of OP and concerns regarding odontological processes and their relationship with anti-osteoporotic drugs.
Tests provided and quality of the referral of patients from primary careOf the respondents, 31% work with a referral protocol agreed with PC; 46% of these included performing DXA and 88% included the assessment of clinical risk factors. Of the rheumatologists, 87.5% and 82% considered it important or very important that patients are referred with bone metabolism analysis and lumbar spine x-ray and 65.1% considered DXA and clinical risk assessment (FRAX/other scales) important or very important. Sixty-five percent of the rheumatologists reported that half or less of referred patients come having undergone some test and 2/3 of the patients referred come without evaluation of the clinical risk of fracture.
Organisational and care aspects of OP in the rheumatologist’s practiceOf the respondents, 20% do not have access to DXA in their health area (14% in regional hospitals, 18% in tertiary hospitals and 33% in specialty centres). Fifty-one percent believe that the DXA report helps them in decision-making and 36% that it is useful in determining the patient’s progress.
The rheumatologists believe that OP due to glucocorticoids, male and secondary OP, and patients with previous fractures and those at high risk of fracture should be seen by rheumatologists (Table 3).
Level of agreement of the rheumatologists on care activity in osteoporosis (scale 1–5, 5 being totally in agreement).
| Mean | Median | SD | Scales |
|---|---|---|---|
| 4.48 | 5 | 1.05 | Glucocorticoid OP is the task of the rheumatologist |
| 4.24 | 5 | 1.07 | Male OP is the task of the rheumatologist |
| 4.44 | 5 | 1.01 | Secondary OP is the task of the rheumatologist |
| 4.57 | 5 | .95 | OP associated with inflammatory disease is the task of the rheumatologist |
| 4.32 | 5 | 1.06 | The patient with a prior fracture is the task of the rheumatologist |
| 4.06 | 4 | 1.12 | OP due to aromatase inhibitors is the task of the rheumatologist |
| 4.56 | 5 | .89 | The care of patients at high risk for fracture is the task of the rheumatologist |
| 3.19 | 4 | 1.31 | Primary OP is the task of PC |
| 3.52 | 4 | 1.22 | The use of FRAX allows the PC physician to justify to the patient that they do not need treatment for their OP |
| 3.46 | 4 | 1.4 | An OP consultation in rheumatology should only exist for patients at high risk |
| 3.86 | 4 | 1.28 | Ours is the OP referral service in their area |
| 3.67 | 4 | 1.22 | OP guidelines are unclear and often misleading |
| 4.24 | 5 | 1.1 | There needs to be a national OP guideline for all specialties. |
| 2.83 | 3 | 1.2 | OP has so much variability that it is not suitable for protocolisation |
| 4.05 | 4 | 1.275 |
OP: Osteoporosis; PC: Primary Care; SD: Standard Deviation.
The percentage of implementation of different organisational strategies in OP and predicted implementation are shown in Table 4. Thirty-eight percent state that their department has a monographic clinic or one dedicated to OP, attended by 3–4 doctors and most spend 2 or more days per week. Of the rheumatologists, 74% believe that not having a monographic clinic is due to lack of resources.
Strategies for the care of patients with OP in rheumatology services.
| Currently existing (%) | Planned to be implemented in the future (<2 years) (%) | |
|---|---|---|
| A specific training programme in OP for residents | 23.8 | 76.2 |
| Physicians who subspecialize in OP and consultants in the service | 50.8 | 49.2 |
| Designated consultant or liaison rheumatologist in this disease in each health centre | 28.6 | 71.4 |
| Department’s own protocols on OP | 47.6 | 52.4 |
| Virtual consultation/electronic consultation/teleconsultation enabled in OP | 30.2 | 69.8 |
| Specialist OP clinic | 38.1 | 61.9 |
| Fracture units (FLS) | 16 | 32 |
FLS: Fracture Liaison Service; OP: Osteoporosis.
There are Fracture Liaison Service (FLS) units in 16% of the hospitals, and in 54% of cases these are rheumatology-led.
Quality management in OPOf the respondents, 43% use quality indicators as proposed by the SER, 17% use quality of life indices and 24% use their own quality indicators. The average delay for a first OP visit and review is 6 and 12 weeks and the estimated review/new patient ratio is 5.4.
Thirty-eight percent believe that the position of OP is like other diseases seen in rheumatology, while 42% answered that they have no idea.
Regarding the follow-up report, 65% consider the rheumatologist's medical report on OP to be acceptable, 82% believe it contains comments on treatment and healthy lifestyle. In 86% the report includes DXA, in 63% the DXA data is explained and in 58% FRAX data is included. Eighty-seven percent agree that a comprehensive and quality report in OP could differentiate it from other specialties that deal with OP.
Nursing care and prevention programmesSixty percent of the departments have a dedicated rheumatology nurse, who cares for patients with OP covering aspects such as education and drug administration (Table 5).
Nursing activities in rheumatology services. Mean percentages.
| Giving diets to patients | 35.7 |
|---|---|
| Explaining the exercises | 21.4 |
| Providing information leaflets on osteoporosis | 31 |
| Clarifying questions on taking and/or administering osteoporosis drugs | 26.2 |
| Instructing on prevention of side effects | 15.5 |
| Receiving patients for specific osteoporosis education consultation | 11.9 |
| Instructing patients on the prevention of falls | 9.5 |
| Attending to patients’ queries by telephone | 31 |
| Attending to patients’ queries in the clinic | 16.7 |
| Administrating denosumab and/or iv bisphosphonates | 26.2 |
The areas for improvement considered important by the respondents are the relationship with PC; standardising and defining care practice; strengthening the role of the rheumatologist as an expert in OP and developing specific training programmes in OP involving different levels of medical and nursing care and patients with OP (Table 6).
Areas for improvement as perceived by the rheumatologists (scale 1–5, 5 being totally in agreement).
| Mean | SD | Areas for improvement |
|---|---|---|
| 4.3 | 1.05 | Enhancing the relationship with PC in relation to OP |
| 4.26 | 1.06 | Enhancing the training of PC physicians in OP |
| 4.37 | 1.03 | Standardising the criteria for requesting tests among rheumatologists and PC |
| 4.17 | 1.07 | Establishing practical and well-defined OP protocols or guidelines through the SER |
| 4.24 | 1.02 | Standardising and clarifying the referral criteria for patients with OP to rheumatology |
| 4.52 | 1.00 | Enhancing the role of the rheumatologist as an expert in OP |
| 4.17 | .92 | Creating a registry, at SER level, on less common or rare bone diseases |
| 3.98 | 1.09 | Improving the information that we provide to patients on the SER website |
| 3.98 | 1.05 | Improving patient discharge reports |
| 4.04 | 1.06 | Promoting healthcare organisation workshops in OP |
| 4 | 1.13 | Promoting the training of specialist nurses through the SER |
| 3.83 | .97 | Promoting telematic consultations in OP |
OP: Osteoporosis; PC: Primary Care; SD: Standard Deviation; SER: Spanish Society of Rheumatology.
The strategic priorities for improving the clinical and organisational approach to the care of patients with OP, agreed by the group of experts through the Delphi round, were as follows:
- 1)
Strategic priorities that should be taken on through the SER:
- a
The SER should promote the inclusion of OP in all services provided, in 100% of the services (in 94% currently).
- b
Widening the SER’s specific OP training offer, for both doctors and nurses.
- a
- 2)
Strategic priorities that should be undertaken through the services:
- a
Promoting the nurses role in patients with OP.
- b
The department head should promote the implementation and monitoring of quality indicators in the care of patients with OP.
- c
Implementing referral protocols agreed with primary care.
- d
Improving the ratio of revisions/new consultations to come closer to the standard provided by the SER.2,3
- a
- 3)
Strategic priorities that should be undertaken jointly:
- a
Improving the care of patients with OP in PC, preventing patients who could be treated in primary care from being referred to specialists. This should involve firstly the rheumatology department itself and then the SER.
- b
Reducing the number of rheumatologists who still do not have access to DXA in their health area.
- c
Establishing as a healthcare criterion that patients with OP should be attended in PC, while those with OP due to glucocorticoids, male and secondary OP, and patients with previous fractures or at high risk of fracture should be seen in rheumatology.
- d
Implementing electronic consultation on OP in 60% of rheumatology services (in 30% currently).
- e
Implementing OP monographic clinics in 70% of rheumatology services.
- f
Ensuring that 60% of rheumatology services participate in FLS units.
- a
This paper presents the first consensus document on strategic priorities in OP from the rheumatologist’s perspective.
Several European medical associations support quality access to rheumatology services for the care of rheumatic diseases, including OP.7 This position is in contrast with the fact that about half the rheumatologists had no concrete idea of the position of OP compared to other rheumatic diseases. However, it is striking how often other specialties refer patients with OP to our clinics, giving us the lead in this disease. OP is included in the programme of the speciality and rheumatologists can lead OP in the same way as, for example, systemic autoimmune diseases. In our opinion, the areas for improvement identified in the survey pave the way for rheumatology to lead the field in OP.
There have been some new developments in recent years that affect the management of OP, such as the importance of secondary fracture prevention, generalised computerised histories and telematic connection with PC.
In this survey, the volume of total and new patients is 10–11 and 3.4 per week, respectively, while in a study of bone metabolism units in Spain it was 20 and 15 per week, respectively.8 Furthermore, the proportion of primary OP is higher in our study (65% vs. 48%). These results indicate that the survey was answered by rheumatologists whose focus of interest is not only OP.
Reasons for referral to rheumatology are very varied in our case, whereas in another study, half the referrals to primary care due to OP were motivated by doubts related to treatment.9
The characteristics of the PC physician mean that most patients with postmenopausal OP can be assessed and, if necessary, treated at primary care level10 and only in the case of concerns would they be susceptible to referral to rheumatology. The rheumatologists responded that almost half the referred patients could have been treated in PC. Rationalising referrals from PC and providing space in the rheumatologist's clinic for the care of secondary OP emerged in our survey as organisational approaches or areas for improvement in the management of OP. In this regard, different scientific societies are attaching a major role to the management of OP as a comorbidity.11
To reduce the variability of care, joint protocols would need to be drawn up for action with other specialities, especially PC. Only 31% of those surveyed work with a referral protocol agreed with PC.
In terms of the tests brought in the referral process from PC, the rheumatologists surveyed consider clinical risk assessment, bone metabolism analysis and plain x-ray of the lumbar spine to be more important than DXA. The frequency with which patients are referred with the tests performed is low, and between 50% and 75% of cases do not provide any tests at all. From this arises another area for improvement identified in our survey, encouraging the autonomy of the PC physician in the care of the patient with OP.
In various studies carried out in Spain, little use is made of FRAX® and other tools for the assessment of fracture risk.12,13 Nevertheless, in our survey the professionals agree that fracture risk factors are necessary to assess OP. Furthermore, when protocols for referral from PC are drawn up, priority is given to the assessment of clinical risk over DXA, as in the EPISER 2016 study in comparison with EPISER 2000.14
The approach is heterogeneous among physicians who manage OP. The need for a national consensus guideline on the management of OP containing recommendations for the appropriate use of clinical risk assessment tools and DXA is another area for improvement identified in our paper. This could reduce the variability that exists in the management of OP.15
Regarding other strategies on OP, the liaison rheumatologist consultant and telematic consultation, with a great deal of future projection, are not very well implemented. It should be noted that, although the specialist or monographic OP clinic is little implemented, when it is, it is very developed.
Regarding the secondary prevention of fractures, the rheumatologists believe that the fracture patient at high risk of presenting further fractures should be seen in rheumatology. Although there is experience and there are FLS models at national level that are rheumatologist-led,16 they are little implemented among the rheumatologists surveyed, more than half do not consider implementing them in the medium term, which contrasts with other strategies. The implementation of FLS in the rheumatological care of OP should clearly be a strategic line promoted by the SER.
Quality patient care, especially if there is multimorbidity and a focus on the complex patient, requires adequate care times. Among the rheumatologists surveyed, the average delay for the first visit was 6 weeks (SER standard: 5.6 weeks), while the average delay for revision was 12 weeks (SER standard: 9.5 weeks).17
The quality indicators set by the SER regarding OP consultations include the recommendation for dedicated OP consultations, that the delay for a first visit should not exceed 8 weeks and that the average length of a first visit should be 20 min.18 These SER indicators are only used by 43% of respondents, but their implementation is recognised as an area for improvement. EULAR has recently established recommendations for the prevention and management of osteoporotic fracture by non-medical health professionals.19 Quality nursing care has been outlined by the SER,20 but its implementation at a general level and in OP in particular is demanded by the majority of respondents in our study. In a review of the literature quality standards for hip fracture were defined.21 However, the SER does not have specific documents on OP or fracture management.
Telematic connection with PC is another organisational change that the rheumatologists indicate as an expectation, thus facilitating non-face-to-face consultations, as has been published.22
Our study has some limitations. As it is a small sample of respondents, it may not represent the opinion of the entire community of rheumatologists or routine clinical practice. The results reflect clinical experience and are exploratory in nature, providing a guiding view. The specialists being from all over Spain and the size of the sample make them illustrative. Despite the bias associated with recall in the responses when dealing with numerical figures, the few related questions give results that are close to the figures collected in other studies.
The authors of this paper believe that the organisation of OP care in rheumatology needs to change with the times. With the implementation of electronic media for interaction with PC and the current relevance of fragility fractures, we believe that the strategic priorities set out here contain a balanced message regarding the organisation of care in OP. The results of the survey bring us closer to the current situation of care in OP ("white paper") and identify possible areas for improvement at an organisational and structural level and in the development and implementation of quality standards in this disease.
Conflict of interestsThe authors have no conflict of interests to declare.
This Quality Improvement Project was carried out within the framework of the CRETA Project promoted by the SER with funding from Laboratorios ROCHE.
Please cite this article as: Naranjo A, Aguado P, de Toro J, Toledo MD, González T, Rosas J, et al. Enfoque organizativo y clínico de la osteoporosis en reumatología: encuesta y consenso OP-SER-Excellence. Reumatol Clin. 2021;17:322–328.