To define the proportion of osteonecrosis (ON) in our patient population with lupus and to identify factors associated with the development of ON in systemic lupus erythematosus, as well as to carry out a descriptive analysis of ON cases.
Materials and methodsObservational retrospective study of 158 patients with SLE (ACR 1982 criteria). Demographic and laboratory data, clinical manifestations, SLICC, SLEDAI, cytotoxic and steroid treatments were compared. In patients with ON, we analyzed time of disease progression and age at ON diagnosis, form of presentation, joints involved, diagnostic methods, Ficat–Arlet classification, and treatment. To compare the means, t-test or Mann–Whitney's test was employed and the cHi-2 test or Fisher's exact test, as appropriate, was used to measure the equality of proportions.
ResultsON was present in 15 out 158 patients (9.5%), 13 women and 2 men, with a mean age of 30 (r: 16–66) at diagnosis and 35 months of evolution until diagnosis (r: 1–195). Among the 15 patients, 34 joints presented ON, 23 were symptomatic and 22 were diagnosed by magnetic resonance images. Twenty-six occurred in hips (24 bilateral), 4 in knees and 4 in shoulders. In 13 patients, ON involved 2 or more joints. At onset, 28 joints were in stage i–ii, one in stage iii and 5 had no data and; in the end, 14 were in stage iii–iv, 5 in stage i–ii and 15 had no data. Twenty-nine underwent conservative treatment with rest and 8 hips required joint replacement. ON progression was associated with Cushing's syndrome (P=0.014) OR 4.16 (95% CI 1.4–12.6) and 2nd year SLICC (P=0.042). No relation with clinical manifestations, lab results, cytotoxic treatment, steroid treatment (total accumulated dose, mean daily dose and duration) metilprednisolone pulses, or activity was found. All patients with ON received antimalarials, in contrast to 77% of those without ON.
ConclusionsThe proportion of ON was 9.5%, mainly in women, 76% in hips (26) and 92% bilaterally. They were associated significantly with Cushing's syndrome and accumulated damage at second year.
Definir la proporción de osteonecrosis (ON) en nuestra población lúpica, identificar factores asociados a su desarrollo y realizar un análisis descriptivo de las ON.
Materiales y métodosEstudio retrospectivo observacional. Se incluyó a 158 pacientes con lupus eritematoso sistémico (criterios ACR 1982), comparando datos demográficos, de laboratorio, manifestaciones clínicas, SLICC, SLEDAI, tratamiento citotóxico y esteroideo. En pacientes con ON se analizaron el tiempo de evolución y la edad al diagnóstico de ON, la forma de presentación, la articulación comprometida, el método diagnóstico, la clasificación Ficat y Arlet y el tratamiento realizado. Se utilizó la prueba de la t o la prueba de Mann–Whitney para la comparación de medias y para igualdad de proporciones o independencia, la prueba de la chi al cuadrado o exacta de Fisher, según correspondiera.
ResultadosLa ON ocurrió en 15/158 pacientes (9,5%), 13 mujeres y 2 hombres. Edad al diagnóstico de ON (mediana): 30 años (r: 16–66) y el tiempo de evolución hasta el diagnóstico de ON: 35 meses (r: 1-195). En los 15 pacientes hubo 34 articulaciones con ON, 23 sintomáticas y 22 diagnosticadas por RM. Veintiséis ON fueron en caderas (24 bilaterales), 4 en rodillas y 4 en hombros. En 13 pacientes la ON afectó a 2 o más articulaciones. Al inicio, 28 articulaciones estaban en estadio i-ii, uno en estadio iii y 5 sin datos y al final, 14 en estadio iii-iv, 5 en estadio i-ii y 15 sin datos. Veintinueve se trataron con reposo y 8 caderas requirieron reemplazo articular. La ON se asoció a aspecto Cushing (p=0,014), OR 4,16 (IC 95% 1,4-12,6) y SLICC 2.° año (p=0,042). No hubo relación con manifestaciones clínicas, datos de laboratorio, tratamiento citotóxico o dosis de esteroides ni actividad. Todos los pacientes con ON recibieron antipalúdicos, a diferencia de un 77% de aquellos sin ON.
ConclusionesLa proporción de ON fue del 9,5%, la mayoría fue en mujeres, el 76% en caderas (26) y el 92% bilateral. Se asociaron significativamente a aspecto Cushing y daño acumulado al segundo año. No se halló relación con el resto de las variables evaluadas.
Osteonecrosis (ON) is the joint manifestation of systemic lupus erythematosus (SLE) that leads to higher morbidity. Incidence of ON in SLE varies from 2.1% to 52%.1–19
Multiple factors have been associated with ON in SLE, including: Cushing's phenotype,1–7 Raynaud's phenomenon,4,5,8 vasculitis,4,6 neurological involvement,1,8 disease activity,9,10 arthritis3 cytotoxic treatment,1,3 superficial thrombophlebitis6 hematuria and proteinuria2 and antiphospholipid antibodies,1,6 among others. There is consensus among most authors regarding the relationship of ON with steroid treatment, but there is controversy whether this relationship depends on the cumulative dose, duration of treatment or the use of large monthly or bimonthly doses. The objectives of this study were to determine the proportion and distribution of bone necrosis in this population and to identify factors associated with its development.
Materials and Methods158 files of patients diagnosed with SLE who were treated at the JM Cullen Hospital in Santa Fe between 1989 and 2012 were retrospectively reviewed. They all met at least 4 classification criteria for SLE (ACR 1982).
Patients considered for inclusion into the study were those in whom the diagnosis of ON was clinically suspected and confirmed through X-rays (Rx), computed tomography (CT), magnetic resonance imaging (MRI) and/or scintigraphy. ON was staged using the Ficat and Arlet11 classification at baseline and at the last valuation of the joint: stage I: normal radiograph with positive MRI, CT scan or pathology; stage II: cystic or sclerotic changes in the X-ray with no signs of collapse; stage iii: collapse of the affected bone, and stage iv: both sides of the joint showing degenerative changes.
Both groups of patients with SLE (with and without ON), were compared for: demographic data, clinical manifestations, comorbidities, antibody profile, accumulated damage by Systemic Lupus International Collaborating Clinics/American College of Rheumatology (SLICC/ACR) damage index at first, second, fifth and tenth year of SLE progression, excluding the score for ON; activity of Systemic Lupus Erythematosus Disease Activity Index (SLEDAI) and exposure to immunosuppressive and antimalarial drugs prior to diagnosis of ON. Total cumulative dose of steroids was also reviewed and expressed as prednisone equivalents up until the diagnosis of ON or until the last control in patients who did present this complication, the duration of steroid therapy and the average daily dose that each patient received since the onset until treatment with corticosteroids ended. Methylprednisolone pulses were defined as the administration of 1000mg or more of prednisone equivalents.
The antibody profile included: antinuclear antibody (Hep 2 epithelial cells), anti-native DNA antibodies by indirect immunofluorescence on Crithidia luciliae, anti-extractable core antigen (anti-Ro, anti-La, anti-Sm and anti-RNP), anticardiolipin (IgG, IgM) and lupus anticoagulant.
The study was approved by the Ethics Committee of the Hospital. It did not require informed consent because of the anonymous nature of the study.
Statistical AnalysisThe Mann–Whitney test was used for comparison of means and proportions and for equal or independent proportions. The chi-square or Fisher's exact test was employed, as appropriate. Data were processed using SPSS 17.0, available from the Department of Mathematics FBCB-UNL. Statistical significance was set at 0.05.
ResultsThe total population of 158 patients with SLE was composed of 92% women, with an average age of onset of SLE of 28 years (R=9–62). Time on follow-up (median) was 87 months (R=0–497).
Among the 158 patients with SLE, 15 were identified as presenting ON (9.5%), 13 women and 2 men. The median time between the onset of SLE and diagnosis of ON was 35 months (R=1–195), the mean age at ON diagnosis was 30 years (R=16–66). Only 6/15 of ON patients had SLEDAI data in the year prior to an episode of ON and 3 of them showed activity of SLE, while four were active at the time of developing ON.
These 15 patients had a total of 34 affected joints: 23 were symptomatic, 9 were asymptomatic and in 2 cases the form of presentation was unknown. Twenty-two were diagnosed by MRI, 7 by X-ray and 2 using CT, with the rest diagnosed by a combination of methods (Table 1). The most commonly affected site was the femoral head (14 patients), being bilateral in 12 cases. These were followed in frequency by the knees and shoulders in 2 patients in each case, and all of them bilaterally (Table 2). Thirteen patients had 2 or more joints involved. Initially, 28 joints were at a precollapse stadium and, in the last evaluation, 14 joints showed radiographic signs of collapse (Table 3). 8 joints were subjected to arthroplasty due to persistent pain or limitation of range of motion (Table 4).
When patients with SLE with and without ON were compared, differences in age at onset of disease, gender ratio, duration of lupus and average mean SLEDAI were seen. Comparing comorbidities, clinical and antibody profiles, only a statistically significant association between ON and Cushing's phenotype was found (60% vs 26.5%, P=.014, odds ratio 4.161,4–6,6–12), as shown in Table 5.
Demographics, Clinical Activity and Antibodies.
| SLE with ON No.=15 | SLE without ON No.=143 | P | |
|---|---|---|---|
| Age at onset SLE (years), mean±SD | 28±11.72 | 28±10,28 | .952 |
| Gender (women/men) | 13/2 | 132/11 | .356 |
| Time since onset (months), median±SD | 130±82.56 | 106.5±95.46 | .356 |
| SLEDAI, mean±SD | 2.71±2.20 | 3.38±3.48 | .724 |
| Diabetes (no. patients) | 0/14 | 2/128 | |
| Hypothyroidism (no. patients) | 2/14 | 21/117 | .999 |
| Cushing phenotypea | 9/15 (60%) | 31/117 (26.5%) | .014 |
| Hypertension | 6/15 | 34/131 | .358 |
| Alcohol | 1/14 | 3/105 | |
| Tobacco use | 2/15 | 23/108 | .734 |
| % Neoplasia | 1/15 | 9/113 | |
| Alopecia | 4 (27) | 45 (31) | .999 |
| Malar rash | 12 (80) | 93 (65) | .389 |
| Photosensitivity | 9 (60) | 74 (52) | .543 |
| Raynaud's | 3 (20) | 41 (27) | .561 |
| Livedo reticularis | 1 (7) | 7 (5) | |
| Mucosal ulcers | 8 (53) | 50 (35) | .160 |
| Arthritis | 12 (80) | 111 (78) | .865 |
| Hip replacement. Jaccoud | 1 (7) | 6 (4) | |
| Renal involvement | 10 (67) | 69 (48) | .174 |
| Cardiac involvement | 4 (27) | 43 (30) | .999 |
| Pulmonary involvement | 7 (47) | 48 (33) | .311 |
| Neurological involvement | 2 (13) | 22 (15) | .999 |
| Myositis | 0 (0) | 1 (0.7) | |
| Vasculitis | 3 (20) | 18 (13) | .424 |
| Thrombosis | 2 (13) | 7 (5) | .205 |
| Leukopenia | 8 (53) | 54 (38) | .240 |
| Lymphopenia | 10 (67) | 76 (53) | .317 |
| Thrombocytopenia | 5 (33) | 31 (22) | .335 |
| Hemolytic anemia | 6 (40) | 54 (38) | .865 |
| FAN (+) | 12/15 (80) | 96/133 (72) | .760 |
| Anti-nDNA (+) | 5/13 (38) | 49/113 (43) | .777 |
| Anti-Ro (+) | 3/12 (25) | 26/72 (36) | .531 |
| Anti-La (+) | 0/9 (0) | 12/61 (20) | |
| Anti-Sm (+) | 0/7 (0) | 18/55 (33) | |
| Anti-RNP (+) | 1/6 (17) | 21/51 (41) | |
| ACL (+) | 2/9 (22) | 30/73 (41) | .471 |
| LA (+) | 2/8 (25) | 12/53 (23) | .999 |
The mean cumulative damage at the second year was significantly higher in patients with ON (P=.042), as shown in Table 6.
SLICC Accumulated Damage in Patients With and Without Osteonecrosis.
| SLICC/ACR damage index | SLE with ONMean±SD | SLE without ONMean±SD | P |
|---|---|---|---|
| 1st year | 0.60±0.89 (n=13) | 0.48±0.83 (n=89) | .402 |
| 2nd year | 1.20±1.30 (n=13) | 0.79±1.01 (n=82) | .042 |
| 5th year | 1.40±1.14 (n=11) | 1.62±1.42 (n=57) | .999 |
| 10th year | 1.80±0.84 (n=5) | 2.55±2.40 (n=29) | .711 |
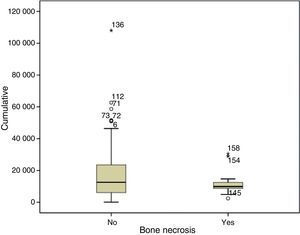
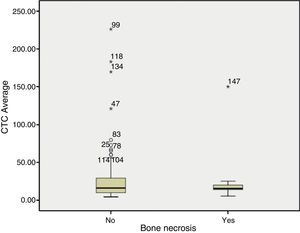
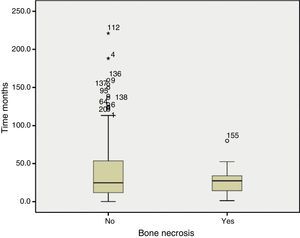
When compared against treatments we found no differences in exposure to cytotoxic therapy or pulse methylprednisolone, but it is worth noting that 100% of patients with ON, unlike 77% of patients without ON, had received antimalarials. With regard to steroid treatment, we found no differences in total cumulative dose (Fig. 1) or average daily dose in mg/day (Fig. 2), nor on the duration of treatment (Fig. 3).
DiscussionON is the osteoarticular manifestation that generates the highest morbidity in patients with SLE, first described by Dubois and Cozen in 1960.12 ON prevalence in this population was 9.5% and this value is comparable with those reported in other series.1–4,7,8,13–15,18
Coinciding with what has been published, ON prevails in females, the joint most commonly affected is the hip, followed by the knee and shoulder, in most cases on a bilateral basis, and it commonly involves 2 or more joints.1–5,7,9–18
Corticosteroids have been widely related in the pathogenesis of ON. The duration of treatment,3 the total cumulative dose,3 the mean daily dose1,6,14 and the use of high doses or large cumulative doses of steroids at different times during the first year of the disease1,2,5,14,15 have been reported as important factors in the development of this complication. Massardo et al.,2 found that patients with ON had no higher cumulative doses of steroids or higher average daily dose of steroids, but the duration of treatment was shorter. This would imply that patients with ON receive large doses of corticosteroids in a short period of time. According to Mok et al.,1 the need for high initial doses of steroids to control the disease is a risk factor, especially if patients are positive to anticardiolipin antibodies or develop Cushing's phenotype.
With respect to the use of pulse methylprednisolone intravenously, Massardo et al.,2 consider it a risk factor for ON; however, Migliaresi et al.,15 found no increased risk in patients receiving methylprednisolone pulses. Rather, this treatment regimen seems to reduce risk.
Our results, like those published by other authors show that the total cumulative dose2,5,7,9,15–17 the average daily dose,2,5,7,16 duration of steroid treatment1,2,5,7 and methylprednisolone pulse therapy1,15,18 are not associated with the development of ON. It is possible that ON reveals patients who have a special sensitivity to corticosteroids, as is shown with the relationship to Cushing's phenotype (as reported by Gladman et al.).7
A highly significant association between prior Cushing phenotype and development of ON has been observed in this and other studies.1–7 It is possible that increased deposition of fat in these patients at the trunk level is accompanied by an increase in the size and/or number of intramedullary lipocytes.5 Zizic et al.,5 postulate that treatment with corticosteroids results in hypertrophy of intramedullary lipocytes, that due to the rigid nature of the bone leads to an increase in the pressure of the bone marrow. This increased pressure results in decreased blood flow and ischemia. Ischemic tissue becomes edematous, resulting in a further increase in pressure with a potentiation of ischemia due to secondary compartment syndrome. Indirect evidence supporting this pathogenesis comes from results of core decompression treatment, which provides rapid relief of symptoms and can stop the disease.
The relationship between ON and antimalarial or cytotoxic treatment is controversial. Some authors found no association between taking antimalarials and the presence of ON9,18; Mok et al. found that patients without ON had been treated with antimalarial at higher rates than those with ON.1 In our series (similar to what was found by Gladman et al.), we found that all patients who had developed ON had received antimalarials, unlike 77% of patients without ON.3 It could be postulated that the activity and severity of SLE itself may predispose to this condition.
In ON has been associated with4,6 vasculitis, Raynaud's phenomenon,4,5,8 neurologic involvement,1,8 arthritis3 superficial thrombophlebitis6 and with hematuria and proteinuria2 among others. We did not find any of these relationships in this population.
There is no agreement on whether there is an association between antiphospholipid antibodies and development of ON in patients with SLE. Mont et al.,6 found a significant association between ON and ACL IgG; Mok et al.,1 associated it with lupus anticoagulant, and Asherson et al.,19 observed that patients with antiphospholipid antibodies and ON had received lower doses of steroids than those with ON and negative antiphospholipid antibodies. We, as in other series, found no differences regarding the presence of antiphospholipid antibodies.3,8,9,15,17,18
SLE activity and the use of large doses of steroids at the time of onset of ON or in the year prior to diagnosis of the disease were significantly associated with the presence of ON.9,10 Other authors reported a lack of correlation between activity and ON.3,14,17,18 We found differences between mean SLEDAI of one patient group and another; This can perhaps be explained by the attenuation of high activity scores in the years before the diagnosis of ON and other years with low values of SLEDAI, lack of data or by the small sample size.
The accumulated damage measured by SLICC, excluding the score for ON, was significantly higher for the second year in the group of patients with ON. Other studies have failed to find an association with this variable.9,18
In conclusion, patients with ON mostly presented bilateral hip affection. The cumulative damage at the second year was significantly higher than in patients without ON. This study provides evidence that Cushing's phenotype is the main risk factor for the development of ON in patients with SLE. No relationship to steroid treatment was found that these patients; it may be that they belong to a special group of patients with sensitivity to steroids. When suspecting ON in this population at risk, highly sensitive techniques such as MRI can be used to reach an early diagnosis.
Ethical ResponsibilitiesProtection of people and animalsThe authors declare this research did not perform experiments on humans or animals.
Data privacyThe authors state that no patient data appear in this article.
Right to privacy and informed consentThe authors state that no patient data appear in this article.
Conflicts of InterestThe authors declare no conflicts of interest.
To Elena Carrera and Liliana Contini, for statistical assistance (Biometrics Unit, Mathematics Department, Faculty of Biochemistry and Biological Sciences, UNL, Santa Fe, Argentina).
The authors also wish to thank Raúl Galoppe, Ph.D. (Montclair State University) for his help in translating the abstract.
Please cite this article as: Gontero RP, Bedoya ME, Benavente E, Roverano SG, Paira SO. Osteonecrosis en lupus eritematoso sistémico. Reumatol Clin. 2015;11:151–155.