The prevalence of osteoporosis (OP) and insufficiency fractures in psoriatic arthritis (PsA) remains controversial. The aim of this study was to describe the prevalence of OP and insufficiency fractures in a representative cohort of patients with PsA, and to analyse its association with general risk factors and characteristics of the psoriatic disease in our geographical area.
MethodsMulti-centric, descriptive study of patients with PsA. We recorded clinical characteristics, as well as protective and risk factors for OP and insufficiency fractures. Hip and lumbar densitometry and lateral X-ray of the spine were evaluated. Descriptive statistics for OP and risk factors were calculated. The patients with OP were compared to those without by univariate analyses, and results were adjusted by age and sex. The association of OP and fractures with clinical characteristics was analysed by logistic regression.
Results166 patients (50 men; 116 women) were included. OP was present in 26.5%, and it was more frequent in women and patients above 50 years old. Insufficiency fractures occurred in 5.4% of the total sample. In the logistic regression, OP was associated with age over 50 [OR 3.7; 95% CI (1.2–11.6); p=.02]. No association with clinical parameters was found. The most frequent risk factors among patients with OP were vitamin D insufficiency, sedentary behaviour, low calcium intake, and active smoking. In the logistic regression, OP was associated with early menopause [OR 11.7; 95% CI (1.29–106.0); p=.029] and sedentary behaviour [OR 2.3; 95% CI (1.0–5.2); p=.049].
ConclusionsIn patients with PsA, OP is more frequent in women and patients over 50 years old. A sedentary lifestyle and early menopause may add extra risk for OP. Type, duration disease, and treatments are not associated with OP or insufficiency fractures.
El objetivo de este estudio fue describir la prevalencia de osteoporosis (OP) y fracturas por insuficiencia en una cohorte representativa de pacientes con artritis psoriásica (APs) y analizar su asociación con factores de riesgo generales y características de la enfermedad psoriásica en nuestra área geográfica.
MétodosEstudio multicéntrico y descriptivo de pacientes con APs. Se registraron las características clínicas, así como los factores protectores y de riesgo de OP y fracturas por insuficiencia. Se evaluó la densitometría de cadera y lumbar y la radiografía lateral de columna. Se calcularon las estadísticas descriptivas de la OP y los factores de riesgo. Los pacientes con OP se compararon con los que no la tenían mediante análisis univariantes, y los resultados se ajustaron por edad y sexo. La asociación de la OP y las fracturas con las características clínicas se analizó mediante regresión logística.
ResultadosSe incluyeron 166 pacientes (50 hombres; 116 mujeres). La OP estaba presente en el 26,5% y era más frecuente en mujeres y pacientes mayores de 50 años. Se produjeron fracturas por insuficiencia en el 5,4% de la muestra total. En la regresión logística la OP se asoció con la edad superior a 50 años (OR: 3,7; IC 95%: 1,2-11,6; p=0,02), con la menopausia precoz (OR: 11,7; IC 95%: 1,29-106,0; p=0,029) y el comportamiento sedentario (OR: 2,3; IC 95%: 1,0-5,2; p=0,049).
ConclusionesEn pacientes con APs la OP es más frecuente en mujeres y en aquellos mayores de 50 años. Un estilo de vida sedentario y una menopausia precoz pueden añadir un riesgo adicional de OP. El tipo, la duración de la enfermedad y los tratamientos no se asocian a las fracturas OP ni a las fracturas por insuficiencia.
Psoriatic arthritis (PsA) is a systemic chronic inflammatory condition, which can affect joint and spine, and present with skin disease as well as entesitis and dactilitis.1 Besides the general risk factors for osteoporosis (OP), the persistent inflammatory environment, the reduction in physical activity or even immobility, the use of corticosteroids and impaired intestinal absorption increase the risk of bone mineral density loss in inflammatory rheumatic diseases.2,3 However, the impact of bone fragility in patients with PsA remains inconclusive. Reduction in bone mineral density (BMD) in patients with PsA was addressed in a systematic review,4 showing a prevalence of OP ranging from 1.4 to 68.8%. This wide range of frequencies might be explained by several inconsistencies regarding the inclusion criteria and the methodology in the studies analysed, but also by the fact that they were set in different populations, with different prevalence of OP. These results underline the need of further studies, which help to describe de prevalence of osteoporosis among patients with PsA.
The aim of this study was to describe the prevalence of OP and insufficiency fractures in a representative cohort of patients with PsA, and to analyse its association with general risk factors and characteristics of the psoriatic disease in our geographical area.
Materials and methodsStudy subjectsWe performed a multi-centric, cross-sectional, descriptive study of 166 patients with PsA, followed in the rheumatology units of four hospitals in the southeast area of Spain. The study was approved by the Clinical Research Ethics Committee of the Hospital General Universitario de Alicante (ISABIAL-approval number 180264).
Patients were eligible if they had a diagnosis of PsA made by a rheumatologist, and were selected randomly in every hospital. Inclusion criteria were: a disease duration of at least 1 year, age ≥21 years old and being actively followed in their respective rheumatology units. Pregnant women and patients with active neoplasms or other systemic uncontrolled conditions were excluded. Consecutive patients who fulfilled the criteria and signed the informed consent form were included until reach the sample size.
Osteoporosis was the dependant variable, according to WHO definition5,6 for women and men. All the patients were asked to undergo lateral X-ray of the dorsal and lumbar spine, and a hip and lumbar densitometry by DXA (dual energy X-ray absorptiometry). We recorded the presence of insufficiency fractures: vertebral fractures, and other insufficiency fractures from the anamnesis and clinical history (hip fracture, shoulder fracture, distal radio fracture or others). Clinical characteristics recorded were: age and sex; duration of disease, type of disease (pure axial, peripheral with or without axial), functional status by the modified Health Assessment Questionnaire (mHAQ), Bath Ankylosing Spondylitis Functional Index (BASFI) value for axial PsA, treatment with classical disease modifying anti-rheumatic drugs (c-DMARDs) and biological drugs (b-DMARDs)>3 months ever. Risk factors for OP and insufficiency fractures were collected. We also recorded protective factors for OP.
Statistical analysisAccepting an alpha risk of 0.05%, we assumed an expected prevalence of OP among PsA patients of 16%, based on a previous published Spanish cohort of patients with OP.7 The sample size calculated was 163 patients. The prevalence of osteoporosis, insufficiency fractures and the risk and protective factors was calculated. Descriptive data are shown as absolute numbers with percentages or mean±standard deviation (SD). The characteristics of the patients with OP were compared to those without by univariate analyses, and all the variables were analysed separating by age (two intervals: <50 and ≥50 years old) and sex. To quantify the strength of the association, we calculated the odds ratio (OR) with 95% confidence intervals (CI). We used logistic regression to analyse the significant results and to adjust confounding factors. Two different models were applied. The first one, combining clinical factors (HAQ, BASFI, biological therapy) with sex and age. The second one, combining the risk factors with sex and age.
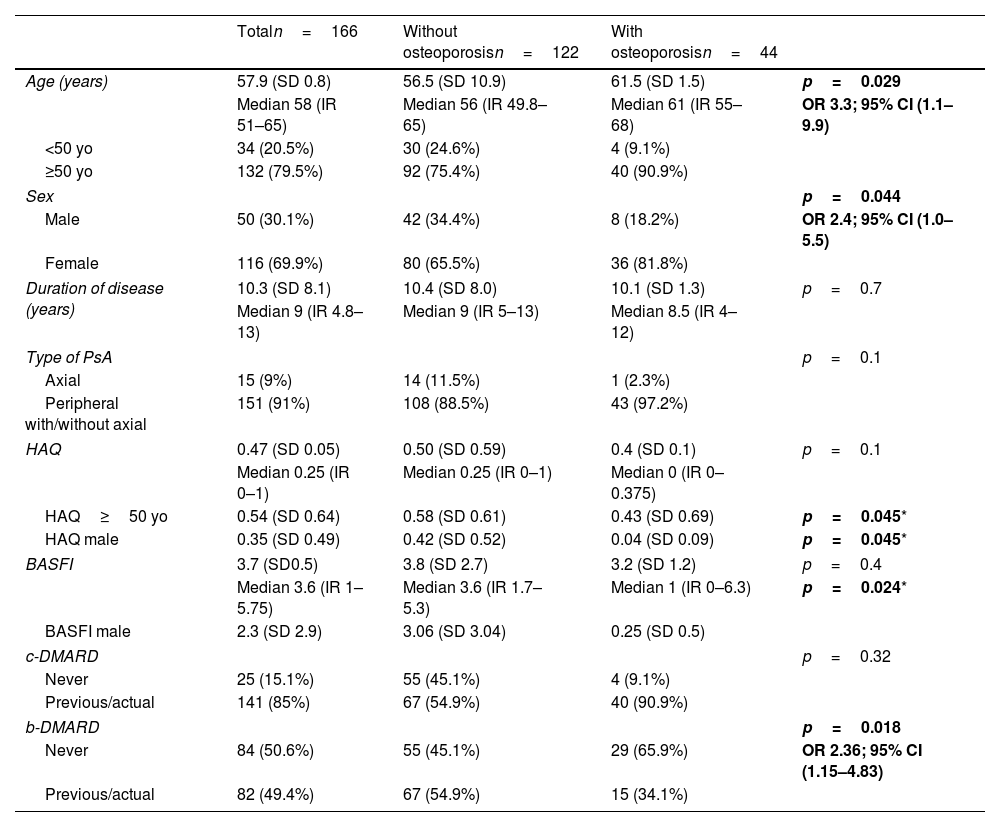
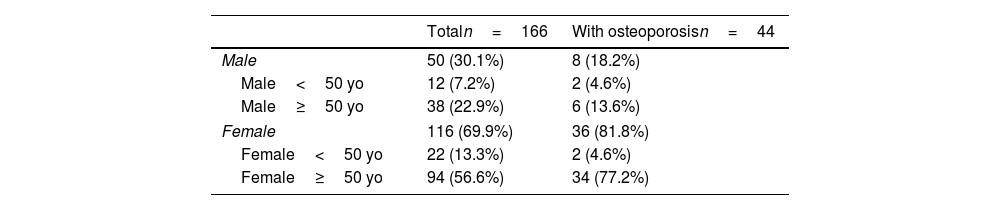
ResultsPrevalence of osteoporosis and insufficiency fracturesA total amount of 166 patients were included, 116 women (69.9%) and 50 men (30.1%), average age was 57.9 years old. The basal characteristics of the cohort are shown in Table 1. OP was present in 44 patients (26.5%), and it was more frequent in women (81.8% vs 8.2%; p=0.044). OP was also more frequent in patients above 50 years old (90.9% vs 9.1%; p=0.029). The frequency of OP by sex and age is shown in Table 2.
Demographical and clinical characteristics. Association with osteoporosis.
| Totaln=166 | Without osteoporosisn=122 | With osteoporosisn=44 | ||
|---|---|---|---|---|
| Age (years) | 57.9 (SD 0.8) | 56.5 (SD 10.9) | 61.5 (SD 1.5) | p=0.029 |
| Median 58 (IR 51–65) | Median 56 (IR 49.8–65) | Median 61 (IR 55–68) | OR 3.3; 95% CI (1.1–9.9) | |
| <50 yo | 34 (20.5%) | 30 (24.6%) | 4 (9.1%) | |
| ≥50 yo | 132 (79.5%) | 92 (75.4%) | 40 (90.9%) | |
| Sex | p=0.044 | |||
| Male | 50 (30.1%) | 42 (34.4%) | 8 (18.2%) | OR 2.4; 95% CI (1.0–5.5) |
| Female | 116 (69.9%) | 80 (65.5%) | 36 (81.8%) | |
| Duration of disease (years) | 10.3 (SD 8.1) | 10.4 (SD 8.0) | 10.1 (SD 1.3) | p=0.7 |
| Median 9 (IR 4.8–13) | Median 9 (IR 5–13) | Median 8.5 (IR 4–12) | ||
| Type of PsA | p=0.1 | |||
| Axial | 15 (9%) | 14 (11.5%) | 1 (2.3%) | |
| Peripheral with/without axial | 151 (91%) | 108 (88.5%) | 43 (97.2%) | |
| HAQ | 0.47 (SD 0.05) | 0.50 (SD 0.59) | 0.4 (SD 0.1) | p=0.1 |
| Median 0.25 (IR 0–1) | Median 0.25 (IR 0–1) | Median 0 (IR 0–0.375) | ||
| HAQ≥50 yo | 0.54 (SD 0.64) | 0.58 (SD 0.61) | 0.43 (SD 0.69) | p=0.045* |
| HAQ male | 0.35 (SD 0.49) | 0.42 (SD 0.52) | 0.04 (SD 0.09) | p=0.045* |
| BASFI | 3.7 (SD0.5) | 3.8 (SD 2.7) | 3.2 (SD 1.2) | p=0.4 |
| Median 3.6 (IR 1–5.75) | Median 3.6 (IR 1.7–5.3) | Median 1 (IR 0–6.3) | p=0.024* | |
| BASFI male | 2.3 (SD 2.9) | 3.06 (SD 3.04) | 0.25 (SD 0.5) | |
| c-DMARD | p=0.32 | |||
| Never | 25 (15.1%) | 55 (45.1%) | 4 (9.1%) | |
| Previous/actual | 141 (85%) | 67 (54.9%) | 40 (90.9%) | |
| b-DMARD | p=0.018 | |||
| Never | 84 (50.6%) | 55 (45.1%) | 29 (65.9%) | OR 2.36; 95% CI (1.15–4.83) |
| Previous/actual | 82 (49.4%) | 67 (54.9%) | 15 (34.1%) | |
BASFI: Bath Ankylosing Spondylitis Functional Index, b-DMARDs: biological disease modifying anti-rheumatic drugs, c-DMARDs: classical disease modifying anti-rheumatic drugs, CI: 95% confidence interval, HAQ: Health Assessment Questionnaire, IR: interquartile range, OR: odds ratio, PsA: psoriatic arthritis, SD: standard deviation, Yo: years old.
Results showed as average with standard deviation and median with interquartile range; or absolute numbers with percentages.
Frequency of osteoporosis by age and sex.
| Totaln=166 | With osteoporosisn=44 | |
|---|---|---|
| Male | 50 (30.1%) | 8 (18.2%) |
| Male<50 yo | 12 (7.2%) | 2 (4.6%) |
| Male≥50 yo | 38 (22.9%) | 6 (13.6%) |
| Female | 116 (69.9%) | 36 (81.8%) |
| Female<50 yo | 22 (13.3%) | 2 (4.6%) |
| Female≥50 yo | 94 (56.6%) | 34 (77.2%) |
Yo: years old.
Results showed as absolute numbers with percentages.
Of the total sample, 9 patients (5.4%) had insufficiency fractures. They were all women over 50 years old, and had a total amount of 14 insufficiency fractures (4 vertebrae, 2 hips, 4 distal radius, 4 others).
Association of osteoporosis with clinical variablesOP was more frequent in women, and in patients over 50 years old. No differences were found between the OP and non-OP groups regarding duration nor type of PsA. We did not observe any differences concerning HAQ neither BASFI values in the total sample. Results are shown in Table I (the variables, which showed association with OP after separating by sex or age, are detailed in the table).
With regard to the treatments, patients who had never been on b-DIMARDs had greater risk of osteoporosis [OR 2.36; 95% CI (1.15–4.83); p=0.018]; this difference did not remained after adjusting by age nor gender. The variables, which showed association with OP after separating by sex or age, are detailed in Table 1.
In the logistic regression. The presence of OP was associated with age over 50 years old [OR 3.7; 95% CI (1.2–11.6); p=0.02]. No other variables significantly predicted the presence of OP.
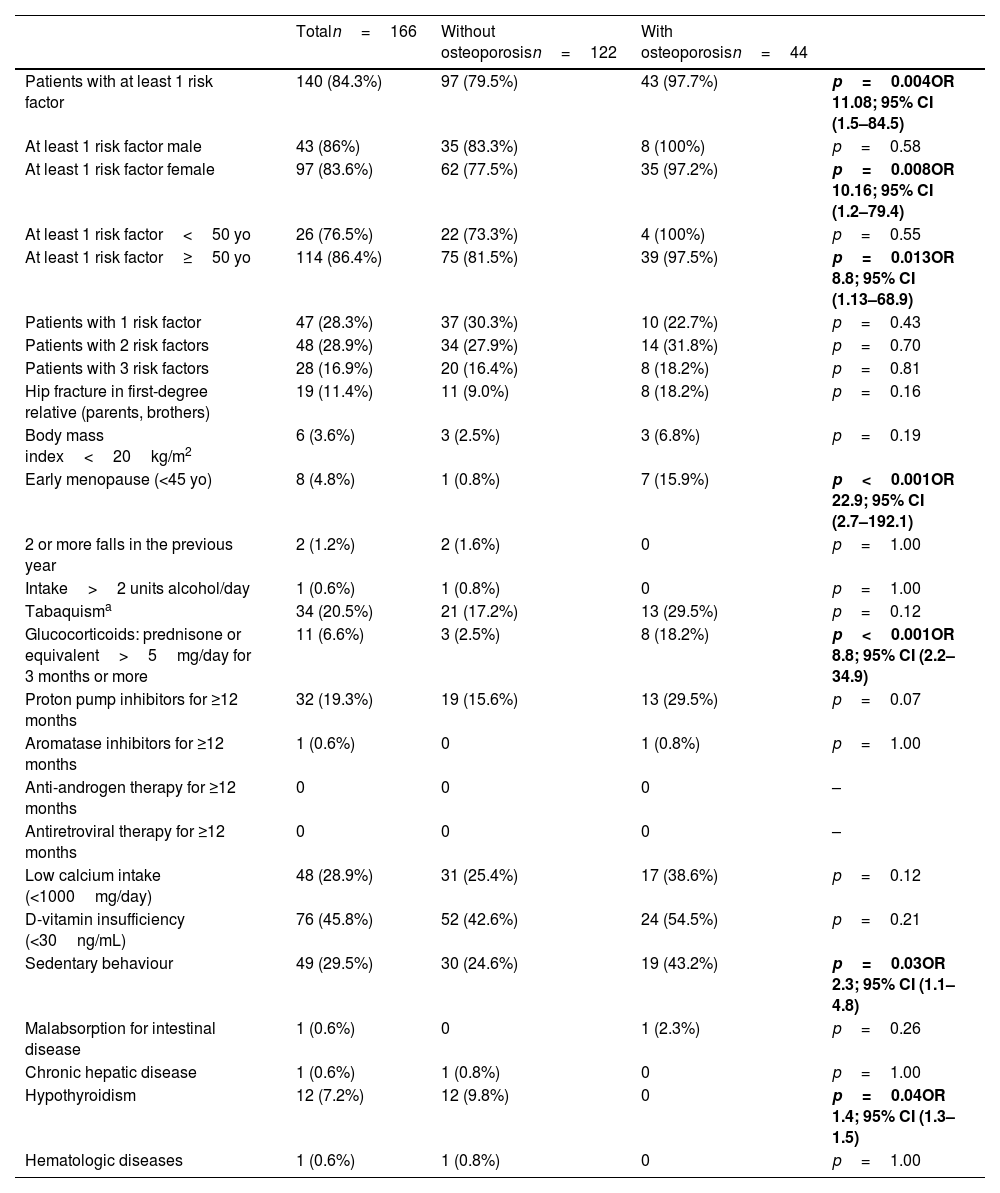
Osteoporosis risk factorsThe most frequent risk factors among patients with OP were: D-vitamin insufficiency (54.5%); sedentary lifestyle (43.2%); low calcium intake (38.6%); smoking (29.5%); use of proton pump inhibitors (29.5%); hip fracture in first-degree relatives (18.2%) and use of glucocorticoids (18.2%). The presence of at least one risk factor was more frequent in the OP group (p=0.004). OP was associated with early menopause (p<0.001), use of glucocorticoids (p<0.001), sedentary lifestyle (p=0.03) and hypothyroidism (p=0.04). Risk factors distribution in the total sample and in the two groups is shown in Table 3. The effect of the risk factors in OP was influenced by age and sex. After adjusting by sex, having at least one risk factor was associated with OP only in the female sex. After adjusting by age, the patients with OP over 50 years old had one risk factor at least.
Risk factors for developing osteoporosis. Results showed as absolute numbers with percentages.
| Totaln=166 | Without osteoporosisn=122 | With osteoporosisn=44 | ||
|---|---|---|---|---|
| Patients with at least 1 risk factor | 140 (84.3%) | 97 (79.5%) | 43 (97.7%) | p=0.004OR 11.08; 95% CI (1.5–84.5) |
| At least 1 risk factor male | 43 (86%) | 35 (83.3%) | 8 (100%) | p=0.58 |
| At least 1 risk factor female | 97 (83.6%) | 62 (77.5%) | 35 (97.2%) | p=0.008OR 10.16; 95% CI (1.2–79.4) |
| At least 1 risk factor<50 yo | 26 (76.5%) | 22 (73.3%) | 4 (100%) | p=0.55 |
| At least 1 risk factor≥50 yo | 114 (86.4%) | 75 (81.5%) | 39 (97.5%) | p=0.013OR 8.8; 95% CI (1.13–68.9) |
| Patients with 1 risk factor | 47 (28.3%) | 37 (30.3%) | 10 (22.7%) | p=0.43 |
| Patients with 2 risk factors | 48 (28.9%) | 34 (27.9%) | 14 (31.8%) | p=0.70 |
| Patients with 3 risk factors | 28 (16.9%) | 20 (16.4%) | 8 (18.2%) | p=0.81 |
| Hip fracture in first-degree relative (parents, brothers) | 19 (11.4%) | 11 (9.0%) | 8 (18.2%) | p=0.16 |
| Body mass index<20kg/m2 | 6 (3.6%) | 3 (2.5%) | 3 (6.8%) | p=0.19 |
| Early menopause (<45 yo) | 8 (4.8%) | 1 (0.8%) | 7 (15.9%) | p<0.001OR 22.9; 95% CI (2.7–192.1) |
| 2 or more falls in the previous year | 2 (1.2%) | 2 (1.6%) | 0 | p=1.00 |
| Intake>2 units alcohol/day | 1 (0.6%) | 1 (0.8%) | 0 | p=1.00 |
| Tabaquisma | 34 (20.5%) | 21 (17.2%) | 13 (29.5%) | p=0.12 |
| Glucocorticoids: prednisone or equivalent>5mg/day for 3 months or more | 11 (6.6%) | 3 (2.5%) | 8 (18.2%) | p<0.001OR 8.8; 95% CI (2.2–34.9) |
| Proton pump inhibitors for ≥12 months | 32 (19.3%) | 19 (15.6%) | 13 (29.5%) | p=0.07 |
| Aromatase inhibitors for ≥12 months | 1 (0.6%) | 0 | 1 (0.8%) | p=1.00 |
| Anti-androgen therapy for ≥12 months | 0 | 0 | 0 | – |
| Antiretroviral therapy for ≥12 months | 0 | 0 | 0 | – |
| Low calcium intake (<1000mg/day) | 48 (28.9%) | 31 (25.4%) | 17 (38.6%) | p=0.12 |
| D-vitamin insufficiency (<30ng/mL) | 76 (45.8%) | 52 (42.6%) | 24 (54.5%) | p=0.21 |
| Sedentary behaviour | 49 (29.5%) | 30 (24.6%) | 19 (43.2%) | p=0.03OR 2.3; 95% CI (1.1–4.8) |
| Malabsorption for intestinal disease | 1 (0.6%) | 0 | 1 (2.3%) | p=0.26 |
| Chronic hepatic disease | 1 (0.6%) | 1 (0.8%) | 0 | p=1.00 |
| Hypothyroidism | 12 (7.2%) | 12 (9.8%) | 0 | p=0.04OR 1.4; 95% CI (1.3–1.5) |
| Hematologic diseases | 1 (0.6%) | 1 (0.8%) | 0 | p=1.00 |
CI: confidence interval, mg: milligrams, mL: millilitres, ng: nano grams, OR: odds ratio, Yo: years old.
In the logistic regression, the presence of OP was associated with the presence of early menopause [OR 11.7; 95% CI (1.29–106.0); p=0.029] and sedentary lifestyle [OR 2.3; 95% CI (1.0–5.2); p=0.049].
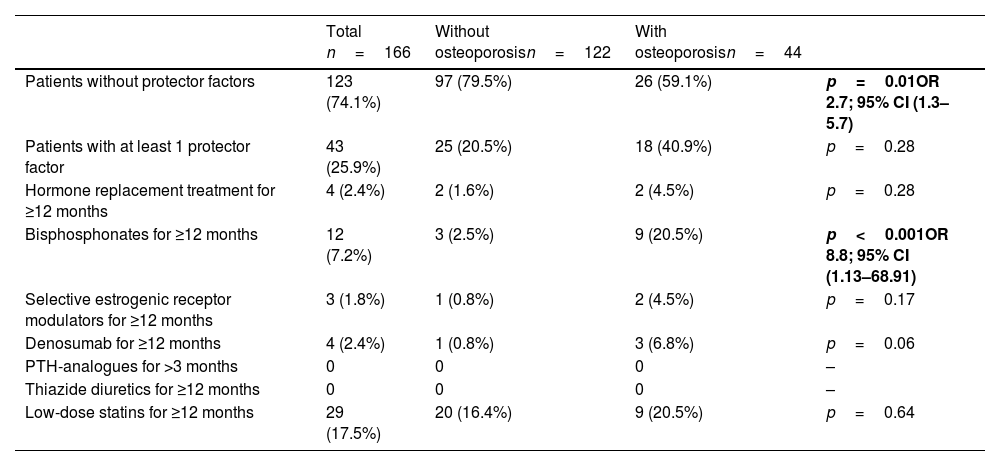
Protective factors for osteoporosisThe most frequent protective factor in the total sample was the use of low-dose statins (17.5%), followed by the use of bisphosphonates (7.2%). Protective factors in the total sample and in the two groups are shown in Table 4.
Protective factors for developing osteoporosis. Results showed as absolute numbers with percentages.
| Total n=166 | Without osteoporosisn=122 | With osteoporosisn=44 | ||
|---|---|---|---|---|
| Patients without protector factors | 123 (74.1%) | 97 (79.5%) | 26 (59.1%) | p=0.01OR 2.7; 95% CI (1.3–5.7) |
| Patients with at least 1 protector factor | 43 (25.9%) | 25 (20.5%) | 18 (40.9%) | p=0.28 |
| Hormone replacement treatment for ≥12 months | 4 (2.4%) | 2 (1.6%) | 2 (4.5%) | p=0.28 |
| Bisphosphonates for ≥12 months | 12 (7.2%) | 3 (2.5%) | 9 (20.5%) | p<0.001OR 8.8; 95% CI (1.13–68.91) |
| Selective estrogenic receptor modulators for ≥12 months | 3 (1.8%) | 1 (0.8%) | 2 (4.5%) | p=0.17 |
| Denosumab for ≥12 months | 4 (2.4%) | 1 (0.8%) | 3 (6.8%) | p=0.06 |
| PTH-analogues for >3 months | 0 | 0 | 0 | – |
| Thiazide diuretics for ≥12 months | 0 | 0 | 0 | – |
| Low-dose statins for ≥12 months | 29 (17.5%) | 20 (16.4%) | 9 (20.5%) | p=0.64 |
PTH: parathormone.
Our results show that 1 of 4 patients with PsA has OP, and osteoporotic fractures occurred in 5.4% of the total sample. Prevalence of OP and insufficiency fractures varies among different geographical areas, and the relevance of OP in patients with PsA may be related to the prevalence of OP in the population of reference. OP in women aged 50 years old or over in Spain has been described to be between 26% and 31.8%,8,9 and prevalent fractures were found in 15.8%.10 In our series of patients with PsA, OP in women over 50 years old was 36.2%, a little higher, compared with the general population in our area. We have not found previous population studies for OP by WHO standards in male. Regarding the frequency of risk factors for OP among patients with PsA in our series, early menopause and sedentary lifestyle were more frequent in the group of patients with OP. A sedentary lifestyle might be an indirect measure of disability caused by severe disease. Regarding protective factors, obviously, the patients with OP had been on anti-osteoporotic drugs more frequently, but beside this, there were no other differences between groups. Statins have been shown to improve bone density.11 However, the molecular mechanisms of lipid-mediated regulation in osteoclasts are not completely understood, and its effect on fracture prevention has not been studied. Nevertheless, statins can be considered protective factors for osteoporosis and therefore we compiled its prescription, although in our study they were not associated with lower risk for osteoporosis or fractures.
Previous works on OP in PsA are limited, with small study groups and conflicting results. The presence of OP was not always the main outcome, and insufficiency fractures were not described homogeneously. In a cross-sectional study of 116 patients with PsA, the authors described 6% of OP in the group, and no fractures.12 More recently, data published from the Nord-Trøndelag Health Study included 69 patients with PsA and 11,703 controls. They found lower prevalence of OP among patients with PsA, compared with the general population (4.4% and 2.8% of OP in lumbar spine and hip, respectively, vs 7.8% and 10.5% in the general population).13 In a recent population-based study, using multivariable linear regression adjusted for confounders, authors did not described the frequencies but found that lower heel-BMD was observed in PsA patients than in controls (male and female). Interestingly, the significance of higher risk of osteopenia in PsA patients was eliminated when conditioning on treatment with methotrexate.14
Higher prevalence of OP was found in two previous works. First, a case–control study with 189 PsA patients found that 30% of the patients had OP (47% among post-menopausal women).15 Second, in a cross-sectional study of 120 patients with PsA, OP was present in 57.3%; such prevalence is the highest described in patients with PsA, but the authors did not describe the selection criteria of the study patients, nor described the percentage of female sex.16 There are different reasons for the inconsistencies among these observational studies, such as the inclusion criteria, the different outcomes or the omission of confounding factors. Our results may be more accurate presenting the real frequency of OP because patients were randomly selected among four different cities, and variables were thoroughly described. Anyway, as we mentioned earlier, the problem of OP in patients with PsA seems mild in our region because the frequency does not differ remarkably from the general population.
In our cohort of patients with PsA the logistic regression did not confirm the association of HAQ and BASFI with OP. Only limited works have studied the association of OP with activity in PsA, without finding significant association.12,13 On the other hand, in the largest series published with data from the CORRONA registry, the authors found for the first time that patients with PsA and erosions had a significantly lower BMD in lumbar spine than those without erosions. The authors proposed that increased inflammatory cytokines in the circulation and in the joint combined with a marked upregulation of osteoclastic activity, common to both forms of bone loss, might explain this relationship.17 Therefore, a persistently active inflammatory environment could increase the risk of OP in PsA the same than in other inflammatory conditions. In a recent case–control study, patients with PsA showed higher prevalence of osteopenia compared to healthy individuals. This association was independent from the sex and menopausal status, which precluded a possible role of the inflammatory involvement.18 In a cross-sectional study which aimed to investigate the impact of b-DMARDs on bone structure, b-DMARD-treated PsA patients showed higher bone mass and better bone strength than patients receiving methotrexate or no treatments. These data also suggest that better control of activity in PsA is related to lesser bone disease.19 In a recent meta-analyses, patients with psoriatic disease had no differences of absolute BMD values that non-psoriatic controls but they were more likely to develop fractures; the higher risk for fracture may be associated with inherent aspects of the psoriatic disease and not necessarily with lower BMD nor a higher risk for osteoporosis.20
ConclusionsIn summary, in patients with PsA, the risk factors for OP are the same than in the general population, but sedentary lifestyle and early menopause may add extra risk. The type of the disease, the duration and the treatments are not associated with the presence of OP or fractures.
This is, to our knowledge, the first multi-centric study designed to analyse the frequency of OP and insufficiency fractures in PsA from a comprehensive point of view, including risk factors, protective factors and clinical characteristics. The strength of this study relies on the aleatory selection in different rheumatology units. The weakness relies on the nature of a descriptive small study. In order to definitively clarify if OP is a special concern in PsA, population-based studies should be conducted, including a holistic approach regarding activity in PsA and risk factors for OP in that specific population.
Informed consentInformed consent was obtained for all subjects, and the study was approved by the Clinical Research Ethics Committee of the Hospital General Universitario de Alicante (ISABIAL-approval number 180264).
Conflicts of interestMaría Paz Martínez-Vidal, Vega Jovani, José Raúl Noguera-Pons and Antonio Álvarez-Cienfuegos declare that they have no conflict of interest.