Psoriatic arthritis (PsA) is a complex inflammatory disease with varied clinical characteristics. A pathognomonic characteristic of PsA is enthesitis. Entheseal inflammation ultimately leads to the production of new bone (enthesophytes). Dickkopf-related protein-1 (DKK-1) is a wingless (Wnt) inhibitor that inhibits osteoblast function.
ObjectivesAssessment of the serum level of DKK-1 and its association with disease activity and enthesopathy in PsA patients.
MethodsThis observational case–control study included 50 PsA patients and 50 healthy volunteers matched for age and gender. All participants were subjected to full medical history, clinical assessment, PSA activity using Disease Activity Index for Psoriatic Arthritis (DAPSA) score, the severity and extent of psoriasis were determined by the Psoriasis Area and Severity Index (PASI). Ultrasonographic assessment of the entheses was done in accordance with the Madrid Sonographic Enthesitis Index (MASEI). Serum level of DKK-1 and correlation with disease activity and enthesopathy in PsA patients were assessed.
ResultsThere was no significant difference between patients and controls regarding age and sex. The mean value of SPARCC index, DAPSA score and PASI score were 6.74±4.58, 33.24±15.26, and 8.35±10.93, respectively. There was significant difference between patients and controls regarding the serum levels of DKK-1 and MASEI score (p<0.0001). There was a significant positive correlation between serum DKK-1 and MASEI (r: 0.43527, p: 0.00158), MASEI inflammatory (r: 0.37958, p: 0.00655), and MASEI damage (r: 0.38384, p: 0.00593).
ConclusionsSerum DKK-1 levels were elevated in PsA patients and were found to be correlated with MASEI score for enthesopathy.
La artritis psoriásica (APs) es una enfermedad inflamatoria compleja con características clínicas variadas. Una característica patognomónica de la artritis psoriásica es la entesitis. La inflamación entesófila finalmente conduce a la producción de hueso nuevo (entesófitos). La proteína 1 relacionada con dickkopf (DKK-1) es un inhibidor sin alas (Wnt) que inhibe la función de los osteoblastos.
ObjetivosEvaluación del nivel sérico de DKK-1 y su asociación con la actividad de la enfermedad y la entesopatía en pacientes con APs.
MétodosEste estudio observacional de casos y controles; incluyó a 50 pacientes con artritis psoriásica y 50 voluntarios sanos emparejados por edad y sexo. Todos los participantes fueron sometidos a historia clínica completa, evaluación clínica, actividad de APs utilizando la puntuación del Índice de Actividad de la Enfermedad para la Artritis Psoriásica (DAPSA), la gravedad y la extensión de la psoriasis fueron determinadas por el área de psoriasis y el índice de gravedad (PASI). La evaluación ultrasonográfica de las entesis se realizó de acuerdo con el índice de entesitis sonográfica de Madrid (MASEI). Se evaluó el nivel sérico de DKK-1 y la correlación con la actividad de la enfermedad y la entesopatía en pacientes con artritis psoriásica.
ResultadosNo hubo diferencias significativas entre los pacientes y los controles con respecto a la edad y el sexo. El valor medio del índice SPARCC, la puntuación DAPSA y la puntuación PASI fueron 6,74±4,58, 33,24±15,26 y 8,35±10,93 respectivamente. Hubo diferencia significativa entre pacientes y controles con respecto a los niveles séricos de DKK-1 y la puntuación MASEI (p <0,0001). Hubo correlación positiva significativa entre DKK-1 sérico y MASEI (r: 0,43527, p = 0,00158), y daño MASEI (r: 0.38384, p = 0,00593).
ConclusionesLos niveles séricos de DKK-1 se elevaron en pacientes con APs y se encontró que estaban correlacionados con la puntuación MASEI para la entesopatía.
Psoriatic arthritis (PsA) is a complex inflammatory disease with various clinical features including peripheral and axial joint inflammation, enthesitis, dactylitis, nail disease, and psoriasis.1 Progressive bone destruction and abnormal bone growth can be detected throughout PsA.2
Patients with PsA show a variety of bone pathologies.3 Bone loss can take place systemically with a reduction of skeletal bone mineral density (BMD) or locally in the form of bone erosion and osteolysis affecting the peripheral joints.4 New bone formation and syndesmophyte formation may also occur. These different bone pathologies can be detected in the same patient.5
Four candidate bone-turnover markers in PsA were identified by a systematic literature review of serum-soluble bone and cartilage-turnover markers in PsA and psoriatic spondyloarthritis (PsSpA): Dickkopf 1 (DKK-1), which inhibits Wnt-mediated bone formation; osteoprotegerin (OPG), which inhibits RANK-mediated bone resorption; and matrix metalloproteinase 3 (MMP-3), which degrades the extra-cellular matrix of bone and cartilage, causing bone erosion and narrowing of the joint space; and macrophage colony stimulating factor (M-CSF), which encourages bone resorption.6
The balance between the osteoclast and osteoblast activities mainly depends on the regulation of the Wnt pathway, which is done by inhibitors as DKK-1 and sclerostin.7
The serum level of DKK-1 in PsA patients is controversial. The aim of this study was to investigate the serum level of DKK-1 and its association with disease activity and enthesopathy in PsA patients.
Patients and methodsIt's a case–control study conducted at a single center.
SettingPatients were recruited from the outpatient clinic of Rheumatology and Rehabilitation Department, Tanta University Hospitals.
PatientsThe study included 50 patients who met CASPAR8 criteria for PsA, and 50 healthy volunteers matched for age and gender. Patients who have used drugs affecting bone metabolism such as bisphosphonates, glucocorticoids, or vitamin D in the past six months, as well as those who are pregnant or who have cancers such as osteosarcoma, prostate cancer, or multiple myeloma were excluded from the study.
Duration of the study: 15 months (from March 2021 to May 2022).
Ethics approval and consent to participateThis study has been approved by the institution's ethics board with permission number 34483/2/21 and is in accordance with the Declaration of Helsinki's ethical principles as well as the ethical standards of the Tanta Faculty of Medicine. According to the local ethical commission, informed consent was received from each patient. Every patient file included a code number that incorporated the results of all investigations, ensuring the privacy of all patient data.
Clinical assessmentDemographic information and a thorough medication history were recorded. The Spondyloarthritis Research Consortium of Canada (SPARCC) Enthesitis Index9 was used to assess the enthesitis clinically. This index measures the tenderness at 16 enthesitis sites, including: bilateral greater trochanter, quadriceps tendon insertion into the patella, patellar ligament insertion into the patella and tibial tuberosity, Achilles tendon insertion, plantar fascia insertion, medial, and lateral epicondyles and the supraspinatus insertion. Each site's tenderness was graded using the following scale: 0 for non-tender and 1 for tender. PSA activity was estimated using the Disease Activity Index for Psoriatic Arthritis (DAPSA) score10 which is numerical summation of 66 swollen and 68 tender joint counts, pain, patient global assessment (PGA), and C-reactive protein (CRP) (mg/dL). Levels of disease activity were divided into four categories: remission (0–4), low disease activity (5–14), moderate disease activity (15–28), and high disease activity (>28).
The Psoriasis Area and Severity Index (PASI) score was used to determine the extent and severity of psoriasis; a representative area of psoriasis is selected for each body region. The severity of the psoriasis’ redness, thickness, and scaling is graded as none (0), mild (1), moderate (2), severe (3), or extremely severe (4).11
Laboratory assessment- •
Routine laboratory assessment: erythrocyte sedimentation rate (ESR) by Westergren method and CRP.
- •
Venous blood samples (10mL) were taken from all individuals after 10h of overnight fasting into sodium citrate and plain plastic tubes. The latter was allowed to clot and centrifuged at 2000rpm for 10min to separate the serum. The collected sera were stored in aliquots at −80°C until used. A citrated blood for erythrocyte sedimentation rate (ESR) by Westergren method, one of the aliquots used for measuring CRP (Thermo Fisher Scientific Inc. Konelab™/T Series CRP Plus 981794) and the other aliquot used for measuring DKK-1 by ELISA (cat no # Dl_DKk1-Hu).
DKK-1 was detected in serum by Enzyme Linked Immunosorbent Assay (ELISA): Reagent and sample preparation, and assay procedure were performed following the instructions of manufacturer. The ELISA kit used sandwich ELISA as method. The microelisa strip plate provided in this kit had been precoated with an antibody specific to DKK-1. Standard or samples were added to appropriate microelisa stripplate wells and combined to specific antibody. The horseradish peroxidase (HRP)-conjugated antibody specific for DKK-1 was added to each microelisa strip plate well and incubated. The free component was washed away. The tetramethyl benzidine substrate solution was added to each well. Only those wells that contain DKK-1& HRP conjugated DKK-1 appeared blue in color then turned yellow after the addition of stop solution. The optical density was measured spectrophotometrically at wavelength of 450mm. The optical density value was proportional to the concentration of DKK-1. The concentration of DKK-1 was calculated by comparing the optical density of the sample to the standard curve.
Ultrasonographic assessmentAccording to the Madrid Sonographic Enthesitis Index (MASEI),12 bilateral ultrasonographic evaluations of the brachial triceps tendons, proximal plantar fascia, distal Achilles tendon, proximal and distal patellar ligaments, and distal quadriceps. Musculoskeletal ultrasonographic (MSUS) examination was conducted using (SAMSUNG MEDISON, UGEO) with linear array transducers (9–13MHz). The ultrasound examination assessed the following fundamental enthesis lesions at each location: structure, thickness, calcifications, erosions, bursae, and power doppler signal in bursa or enthesis full tendon. The total MASEI score was further divided into the following: chronic damage, including enthesophytes, calcifications, and erosions (MASEI damage); and inflammatory changes including entheseal structural changes; thickening; bursitis and vascularization (MASEI-inflammatory).
Assessment of patients was performed by a rheumatologist experienced in MSUS imaging on the same day of the clinical and laboratory evaluation. Inter-observer reliability: Two physicians who were blind to the clinical and laboratory results independently read every image.
Statistical analysisData were statistically analyzed using SPSS version 20. Qualitative data were described using numbers and percentages. The Kolmogorov–Smirnov & Shapiro–Wilk test was used to verify the normality of distribution. Quantitative data were described using mean, standard deviation, median and interquartile range (IQR). Chi-square test was used for comparing categorical data. Student's t-test was used for normally distributed quantitative variables, to compare between two studied groups. Mann–Whitney test was used for abnormally distributed quantitative variables, to compare between two studied groups. Correlation between two distributed abnormally quantitative variables was done using Spearman coefficient. p values less than 0.05 was considered statistically significant.13
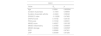
ResultsThere was no significant difference between patients and controls regarding age and sex. The mean duration of psoriasis was 6.24±6.27 years while the mean duration of PsA was 2.33±2.19 years. 31 patients were on conventional synthetic disease modifying antirheumatic drugs (csDMARDs), while 19 patients were receiving biological therapy. Demographic data are summarized in Table 1.
Demographic and disease-related characteristics of the PSA patients and controls.
| PSA patients (50) | Controls (50) | p value | |
|---|---|---|---|
| Age (years) | 38.70±10.49 | 35.8±6.61 | 0.175 |
| Sex: (male/female) | 23/27 | 25/25 | 0.689 |
| BMI | 27.65 | 26.29 | |
| Duration of psoriasis (ys) | 6.24±6.27 | NA | |
| Duration of psoriatic arthritis (ys) | 2.33±2.19 | NA | |
| Treatment received: | NA | ||
| csDMARDs | 31 | ||
| bDMARDs | 19 | ||
| Anti-TNF | 11 | ||
| IL17 inhibitor | 8 | ||
BMI, body mass index; csDMARDs, convential synthetic disease modifying antirheumatic drugs; bDMARDs, biologic disease modifying antirheumatic drugs.
Significant p value if <0.05.
The mean value of SPARCC index was 6.74±4.58. The mean value of DAPSA score was 33.24±15.26; 3 patients had low disease activity, and 23 patients had moderate disease activity, while 24 patients had severe disease activity. The mean value of PASI score was 8.35±10.93. There was significant difference between patients and controls regarding the serum levels of DKK-1 and MASEI score (p<0.0001). Table 2 summarizes clinical, laboratory, and radiological data.
Clinical, laboratory & ultrasonographic assessment of the PSA patients and controls.
| PSA patients (50) | Controls (50) | p value | |
|---|---|---|---|
| SPARCC index | 6.74±4.58 | ||
| DAPSA score (median±SD) | 33.24±15.26 | NA | |
| Remission (n) | 0 | ||
| Low disease activity (n) | 3 | ||
| Moderate disease activity (n) | 23 | ||
| Severe disease activity (n) | 24 | ||
| PASI score (median±SD) | 8.35±10.93 | NA | |
| MASEI score (median±SD) | 26.46±11.59 | 2.82±0.69 | <0.0001* |
| MASEI inflammatory (median±SD) | 12.72±5.17 | 0.76±0.56 | <0.0001* |
| MASEI damage (median±SD) | 13.74±7.94 | 2.06±0.71 | <0.0001* |
| CRP median (IQR) | 4.5 (3–10) | 6.0 (5.0–8.0) | 0.04* |
| ESR (1st hour) median (IQR) | 20 (15–30) | 18 (15.75–22) | 0.116 |
| DKK1 level (pg/mL) | 2680.675 (2078.975–3815.08) | 1194.65 (911.925–1335.198) | <0.0001* |
| Median (IQR) | |||
SPARCC, Spondyloarthritis Research Consortium of Canada; DAPSA, Disease Activity Index for Psoriatic Arthritis; PASI, Psoriasis Area and Severity Index; MASEI, Madrid Sonographic Enthesitis Index; CRP, C-reactive protein; ESR, erythrocyte sedimentation rate; SD, standard deviation; IQR, interquartile range.
There was a significant lower level of DKK-1 in PsA patients treated with bDMARDS (2180.52±1206.53pg/mL) when compared to those treated with csDMARDS (3575.58±1734.53) (p<0.005). There was no statistically significant difference regarding DAPSA, total MASEI, MASEI inflammatory and MASEI damage between patients treated with csDMARDs and those treated with bDMARDs. p=0.405, 0.565, 0.642, 0.588, respectively.
There was a statistically significant positive correlation between serum DKK-1 and MASEI (r: 0.43527, p: 0.00158), MASEI inflammatory (r: 0.37958, p: 0.00655) and MASEI damage scores (r: 0.38384, p: 0.00593). Table 3 summarizes correlations between DKK-1 and different parameters.
Correlation between DKK1 and age, duration of psoriasis, duration of psoriatic arthritis, SPARCC index, DAPSA, PASI, MASEI score, ESR and CRP.
| DKK1 | ||
|---|---|---|
| Value | Rs | p |
| Age | 0.0264 | 0.855594 |
| Duration of psoriasis | −0.1004 | 0.48959 |
| Duration of psoriatic arthritis | −0.2424 | 0.09042 |
| SPARCC index | −0.10299 | 0.47665 |
| DAPSA score | 0.16192 | 0.26125 |
| PASI score | 0.15162 | 0.29321 |
| MASEI score | 0.43527 | 0.00158* |
| MASEI inflammatory | 0.37958 | 0.00655* |
| MASEI damage | 0.38384 | 0.00593* |
| ESR | 0.05995 | 0.67921 |
| CRP | 0.00499 | 0.97256 |
SPARCC, Spondyloarthritis Research Consortium of Canada; DAPSA, Disease Activity Index for Psoriatic Arthritis; PASI, Psoriasis Area and Severity Index; MASEI, Madrid Sonographic Enthesitis Index; ESR, erythrocyte sedimentation rate; CRP, C-reactive protein.
Psoriatic arthritis (PsA) is a chronic systemic immune condition, affecting peripheral and/or axial joints. The purpose of this study was to evaluate the serum level of DKK-1 in PsA patients and their relationship to disease activity and enthesopathy.
Psoriatic arthritis patients showed a higher level of DKK-1 than the control group. Serum level of DKK-1 was correlated with total MASEI score, MASEI inflammatory, and MASEI damage scores.
According to Dalbeth N et al.,14 PsA patients with or without erosion had higher levels of DKK-1 than psoriatic controls, and there was no correlation between the level of DKK-1 and the pattern of bone disease in PsA patients.
Jadon DR et al.15 found that DKK-1 concentrations were significantly higher in PsA patients with radiographic axial affection compared with patients without axial affection.
Furthermore, Chung Y et al.16 reported that the level of serum DKK-1 in PsA was higher compared with patients with rheumatoid arthritis patients and healthy controls and that increased level of DKK-1 was correlated with swollen joint count. There is no difference between PsA patients with elevated DKK-1 and those with normal DKK-1 levels regarding the duration of arthritis/psoriasis, the number of tender joints, the frequency of nail psoriasis, dactylitis, and enthesitis. However, PsA patients with elevated DKK-1 have a higher swollen joint count, sacroiliitis, and bone erosion.
Sungsin Jo et al.17 reported that DKK-1 directly promoted bone formation in enthesis in ankylosing spondylitis patients.
On the other hand, Fassio A et al. showed that PsA patients had lower levels of DKK-1 than those with rheumatoid arthritis and the control groups.18 Additionally, Daoussis et al.19 observed that DKK-1 did not differ between PsA patients and controls, and no correlation was found between DKK-1 and acute phase reactant (ESR and CRP) indicating that expression of Wnt antagonist isn’t linked to acute phase response.
Enthesitis is characterized by a strong tissue reaction, which is an early sign of diseases like PsA. Enthesitis then leads to consequences including enthesophytes, calcaneal spurs, and plantar fasciitis. Resident mesenchymal cells, which have the capacity for proliferation and differentiation inside the chondroblasts and the osteoblasts to produce cartilage and bone, are likely the source of these new bone forms. PGE2 plays a significant role in promoting osteoblast differentiation. Similarly, Wnt proteins coupled with their inhibitors, DKK-1 and sclerostin, are effector molecules that enhance the activity of osteoblasts for the apposition of new bone in the entheses.20,21
DKK-1 acts as an endogenous inhibitor of the Wnt/β-catenin signaling pathways. Wnt-1 protein can signal proliferation via β-catenin after binding to low-density lipoprotein receptor-related protein-5/6 (LRP5/6) and the frizzled receptor. DKK-1 binds to LRP5/6 and prevents binding between LRP5/6 and Wnt-1, causing degradation of β-catenin which blocks the formation and differentiation of osteoblasts and stimulates the apoptosis of immature osteoblasts.22,23
Because DKK-1 is an inhibitor of the Wnt pathway, which stimulates osteoblastogenesis and the synthesis of new bone, one may assume that DKK-1 levels would decrease over the course of a spectrum of diseases with increasing new bone formation. However, in line with many previous studies, DKK-1 levels in SpA may be higher because DKK-1 is pathologically dysfunctional. According to Daoussis et al.,19 DKK-1 is dysfunctional in AS even though serum total DKK-1 levels are higher in patients with AS compared to those with healthy controls or PsA; they reported reduced binding of DKK-1 to its receptor in AS may lead to unopposed stimulation of Wnt signaling pathway. According to Yucong et al.,24 functional DKK-1 levels in serum were observed to be lower in AS patients compared to healthy controls since DKK-1 binds less strongly to its receptor LRP6. According to Heiland GR et al.,25 an absence of syndesmophyte development in AS patients is associated with elevated serum levels of functional DKK-1 binding to its receptor LRP-6. This could explain the elevated DKK-1 levels in our patients as an attempt to compensate for dysfunctional DKK-1. The osteoproliferative phenotype of SpA may be explained by inadequate Wnt-pathway inhibition caused by dysfunctional DKK-1, which stimulates unlimited bone formation. Another theory is that the serum of PsA patients has soluble DKK-1 inhibitors, such as autoantibodies against DKK-1 or soluble receptors.
Previous studies have suggested that DKK-1 participates in osteoblast development in a dual stage-dependent manner. DKK-1 is involved in physiological changes associated with mineralization because research has shown that it is decreased during extra-cellular matrix maturation but increases during the mineralization stage of osteoblast differentiation.26,27
The level of DKK-1 was lower in PsA patients treated with bDMARDS when compared to those treated with csDMARDS.
It was reported that after 12 months of anti-TNF treatment, DKK-1 level was lower in PsA patients when compared to rheumatoid arthritis patients.28 Also, treatment with secukinumab may influence WNT inhibitors (DKK-1 and sclerostin) as DKK-1 and sclerostin show significant increase after treatment with secukinumab.29
DKK-1 has been linked to structural damage pathogenesis, syndesmophyte production, and new bone formation in SpA, however most of the results are contradictory.19,23 Serum levels of DKK-1 were further elevated in AS patients receiving anti-TNF treatment,19 The authors proposed that the greater levels of DKK-1 may represent a compensatory mechanism to reduce Wnt signaling, which is activated after the treatment-induced reduction in inflammation. On the other hand, according to a different study, circulation levels of DKK-1 were lower in AS patients compared to healthy controls and remained unchanged after anti-TNF therapy.23 According to a prospective study on SpA patients found that treatment with TNF blockers caused a significant decrease in DKK-1 level. This decrease was correlated with the reduction of MRI bone marrow edema of the sacroiliac joint and spine. The reduction of DKK-1 by anti-TNF agents may be related to the inhibitory effects of these drugs on new bone formation in SpA.30
To our knowledge, this is few studies that evaluated the levels of DKK-1 in PsA patients in relation to enthesopathy which is a common feature in PsA patients and in this study musculoskeletal ultrasonography was used to evaluate enthesopathy using MASEI score which is more sensitive in evaluation of enthesopathy than clinical assessment. There were some limitations in this study as this is single-centered study, it was better if it was a multicenter study also it was better if the participants were a larger number. Our study is a cross-sectional study, future longitudinal studies are needed to assess if serum level of DKK-1 decreases overtime also future studies needed to assess the level of functional DKK-1 in PsA patients.
ConclusionSerum DKK-1 levels were elevated in PsA patients and were found to be correlated with MASEI score for enthesopathy so, it may be involved in enthesopathy formation in PsA.
Authors’ contributionsMAWA and SAT conceived the idea for the study and in conjunction with NME designed the study and wrote the analysis plan. MAWA and SAT undertook data analysis and interpretation, supported RME. The initial draft of manuscript was written by SAT and RME, with contribution from MAWA.
All authors contributed in the study methodology, analysis, and interpretation of the data and outcomes as well as the manuscript writing, reading, and approval of the final version.
AuthorshipAll named authors meet the International Committee of Medical Journal Editors (ICMJE) criteria for authorship for this article, take responsibility for the integrity of the work as a whole, and have given their approval for this version to be published.
Compliance with ethics guidelinesThis study has been approved by the institution's ethics board with permission number 34483/2/21 and is in accordance with the Declaration of Helsinki's ethical principles as well as the ethical standards of the Tanta Faculty of Medicine. According to the local ethical commission, informed consent was received from each patient. Every patient file included a code number that incorporated the results of all investigations, ensuring the privacy of all patient data.
Compliance with ethical standardsAll steps are performed according to the revised ethical principles of the Declaration of Helsinki in 2000, and local ethical and methodological protocols for approval of the study were followed.
Data availabilityThe datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
Consent for publicationThe final manuscript has been seen and approved by all the authors, and they have obtained the required ethical approvals, and they have given the necessary attention to ensure the integrity of the work and agree to publish this work.
Ethics approval and consent to participateThis study is in agreement with the ethical guidelines of the Declaration of Helsinki and it follows the ethical standards of Tanta Faculty of Medicine, with the institution's ethics board approval number 34483/2/21. Informed consent from all patients was obtained in accordance with the local ethical committee. Privacy of all patients’ data was granted as there was a code number for every patient file that included all investigations.
FundingNo funding or sponsorship was received for this study or publication of this article.
Conflict of interestThe authors declare no conflict of interest.
The authors would like to thank the participants of the studies.