Termination of pregnancy in patients with rheumatic diseases is controversial and a bioethical analysis is rarely performed. In this study we analysed the case of a pregnant patient with lupus nephritis unresponsive to treatment, for whom termination of pregnancy is considered.
MethodsThe integrative model was applied combining different normative ethical theories.
ResultsFrom a utilitarian perspective, termination of pregnancy is justifiable, seeking the greatest benefit for the greatest number of stakeholders. Deontology justifies both terminating and continuing the pregnancy, focusing on the action itself and on autonomy. In virtue ethics the importance of decisions rests with the person who performs the action seeking flourishing; termination of pregnancy would be justifiable.
Discussion and conclusionsInterruption of pregnancy is a justifiable solution following the integrative model. Bioethical analysis of paradigmatic cases is essential to ensure the best possible action and as a precedent for future similar situations in rheumatology.
La interrupción del embarazo en pacientes con enfermedades reumatológicas es controvertida y pocas veces se realiza un análisis bioético. En este estudio analizamos el caso de una paciente embarazada con nefritis lúpica sin respuesta a tratamiento en quien se plantea la interrupción del embarazo.
MétodosSe aplicó el modelo integral incluyendo distintos sistemas normativos para el análisis del dilema.
ResultadosDesde el utilitarismo es justificable la interrupción del embarazo, buscando el mayor beneficio para la mayoría de las partes. La deontología justifica tanto continuar como interrumpir el embarazo, centrando la importancia en la acción misma y en la autonomía. Para la ética de la virtud la importancia de las decisiones recae en la persona que realiza la acción buscando el florecimiento; la interrupción del embarazo sería justificable.
Discusión y conclusionesLa interrupción del embarazo sería una solución adecuada según el modelo integral. El análisis bioético de casos paradigmáticos es fundamental para asegurar el mejor actuar posible en casos similares en Reumatología.
Termination of pregnancy in patients with rheumatological diseases is a controversial situation, as there are no statistics or evidence to make recommendations. Termination of pregnancy as a therapeutic alternative during periods of disease activity is performed based on the opinion of health professionals and is reported in 21.7%–25.3% of cases.1
Although termination of pregnancy as a therapeutic measure poses an ethical dilemma, clinical ethics analyses are rarely performed in rheumatology. A review found that publications devoted to bioethics in rheumatology accounted for 0.026% of all articles, despite the high frequency of ethical dilemmas in patients with autoimmune diseases.2 Taking into account the lack of an ethical perspective in rheumatology, the aim of this study is to analyse the case of a pregnant patient with lupus nephritis who did not respond to treatment and who was offered termination of pregnancy as a therapeutic alternative.
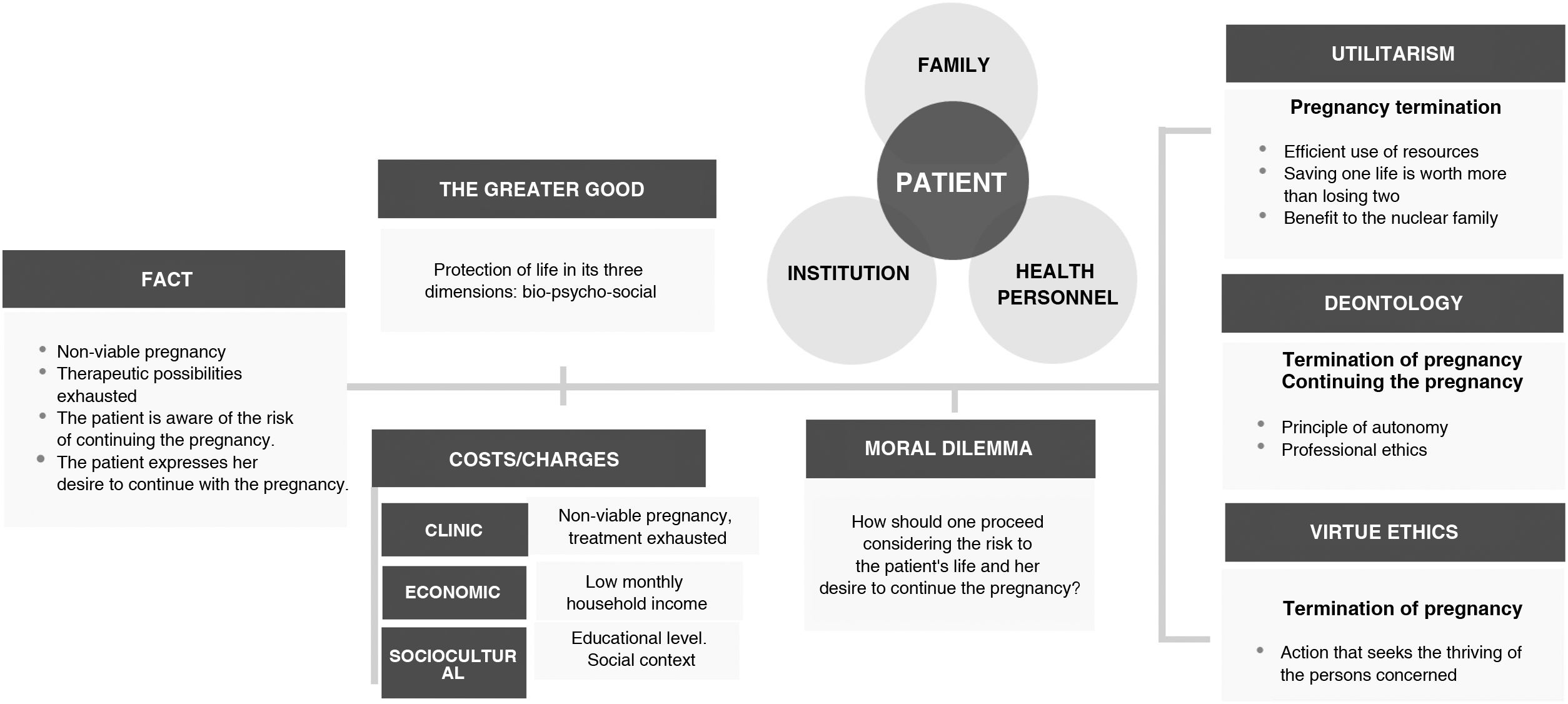
MethodsThe integral model was applied and an analysis was made from different normative ethical systems.3 The event, the greater good and the actors involved in the case were identified, as well as the central moral dilemma. Conclusions were drawn from utilitarian, deontological and virtue ethics perspectives, and then a joint analysis was made to establish an overall conclusion of the dilemma.
The treating medical staff reflected on their experience during the case.
Ethical considerationsThe patient signed the informed consent for the development of the case and its publication.
ResultsCase presentationA 30-year-old Catholic woman, in a civil partnership, originally from and resident of Mexico City, whose family nucleus was in vulnerable conditions due to her socioeconomic level and schooling.
The patient had been diagnosed with systemic lupus erythematosus according to SLICC 2012 classification criteria since 2019. At diagnosis, a remission induction scheme was started due to renal activity (lupus nephritis class III + V): methylprednisolone and cyclophosphamide from March to September 2019. In December 2019, cyclophosphamide was started every two months. Due to increased proteinuria, mycophenolate mofetil (2 g/d) was started in February 2020. Treatment was suspended from February to July 2020 due to the covid-19 pandemic. On resuming follow-up, an increase in proteinuria to 5720 mg in 24 h was documented, resulting in cyclophosphamide, mycophenolate mofetil (2 g/d) and prednisone (25 mg/d) being restarted every two months until April 2021, without achieving complete remission criteria. In April 2021, multi-target therapy (3 g/d of mycophenolate mofetil and 3 g/d of tacrolimus) was started due to poor response; however, the patient did not adhere to treatment for financial reasons.
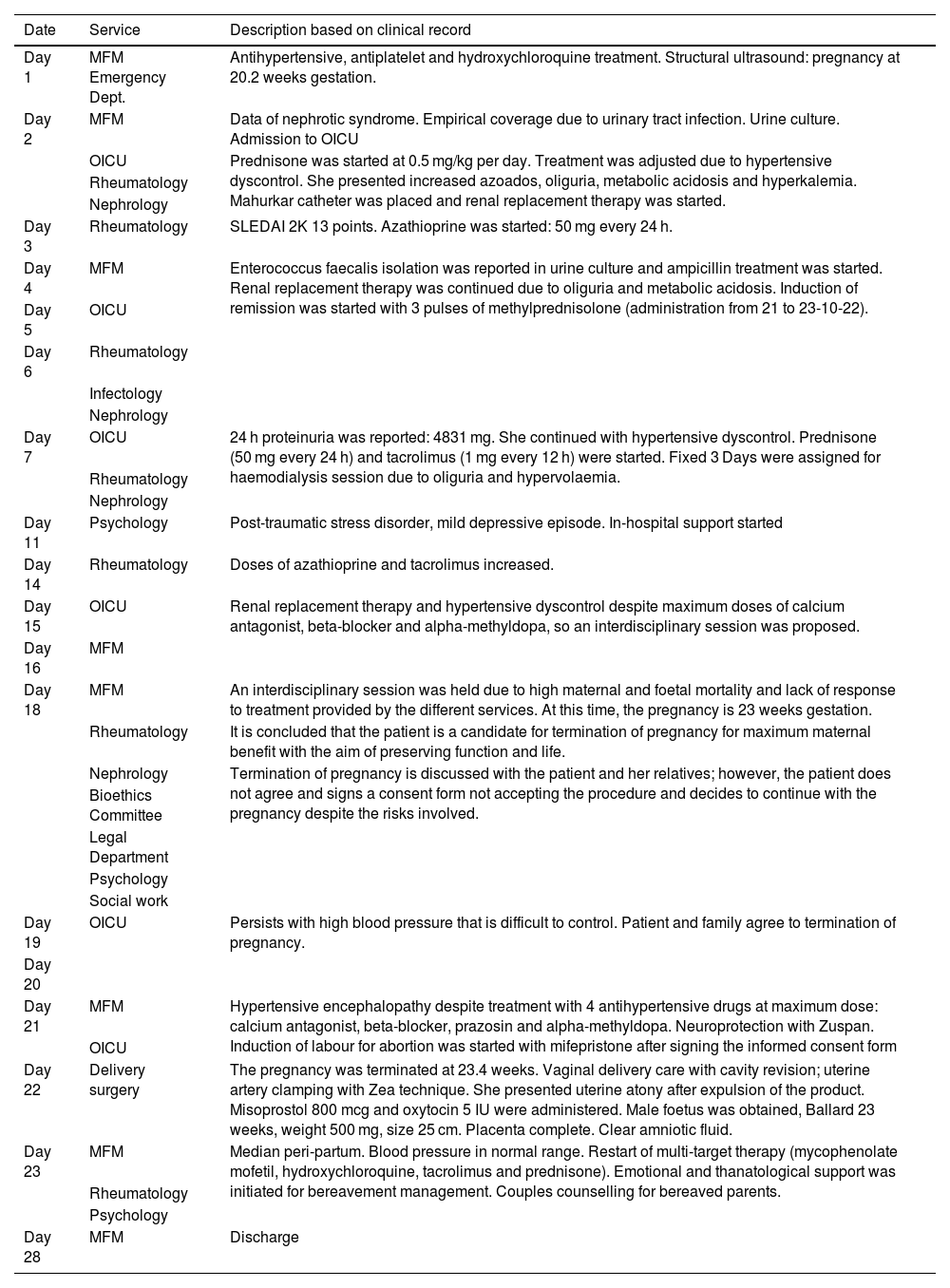
The patient attended a prenatal check-up appointment on 17 October 2022 for pregnancy at 20 weeks' gestation. Oedema in the lower extremities and arterial hypertension were identified, for which she was referred and hospitalised in gynaecology and obstetrics at a tertiary level hospital in Mexico, where her evolution was documented (Table 1).
Patient's evolution during hospitalisation.
| Date | Service | Description based on clinical record |
|---|---|---|
| Day 1 | MFM Emergency Dept. | Antihypertensive, antiplatelet and hydroxychloroquine treatment. Structural ultrasound: pregnancy at 20.2 weeks gestation. |
| Day 2 | MFM | Data of nephrotic syndrome. Empirical coverage due to urinary tract infection. Urine culture. Admission to OICU |
| OICU | Prednisone was started at 0.5 mg/kg per day. Treatment was adjusted due to hypertensive dyscontrol. She presented increased azoados, oliguria, metabolic acidosis and hyperkalemia. Mahurkar catheter was placed and renal replacement therapy was started. | |
| Rheumatology | ||
| Nephrology | ||
| Day 3 | Rheumatology | SLEDAI 2K 13 points. Azathioprine was started: 50 mg every 24 h. |
| Day 4 | MFM | Enterococcus faecalis isolation was reported in urine culture and ampicillin treatment was started. Renal replacement therapy was continued due to oliguria and metabolic acidosis. Induction of remission was started with 3 pulses of methylprednisolone (administration from 21 to 23-10-22). |
| Day 5 | OICU | |
| Day 6 | Rheumatology | |
| Infectology | ||
| Nephrology | ||
| Day 7 | OICU | 24 h proteinuria was reported: 4831 mg. She continued with hypertensive dyscontrol. Prednisone (50 mg every 24 h) and tacrolimus (1 mg every 12 h) were started. Fixed 3 Days were assigned for haemodialysis session due to oliguria and hypervolaemia. |
| Rheumatology | ||
| Nephrology | ||
| Day 11 | Psychology | Post-traumatic stress disorder, mild depressive episode. In-hospital support started |
| Day 14 | Rheumatology | Doses of azathioprine and tacrolimus increased. |
| Day 15 | OICU | Renal replacement therapy and hypertensive dyscontrol despite maximum doses of calcium antagonist, beta-blocker and alpha-methyldopa, so an interdisciplinary session was proposed. |
| Day 16 | MFM | |
| Day 18 | MFM | An interdisciplinary session was held due to high maternal and foetal mortality and lack of response to treatment provided by the different services. At this time, the pregnancy is 23 weeks gestation. |
| Rheumatology | It is concluded that the patient is a candidate for termination of pregnancy for maximum maternal benefit with the aim of preserving function and life. | |
| Nephrology | Termination of pregnancy is discussed with the patient and her relatives; however, the patient does not agree and signs a consent form not accepting the procedure and decides to continue with the pregnancy despite the risks involved. | |
| Bioethics Committee | ||
| Legal Department | ||
| Psychology | ||
| Social work | ||
| Day 19 | OICU | Persists with high blood pressure that is difficult to control. Patient and family agree to termination of pregnancy. |
| Day 20 | ||
| Day 21 | MFM | Hypertensive encephalopathy despite treatment with 4 antihypertensive drugs at maximum dose: calcium antagonist, beta-blocker, prazosin and alpha-methyldopa. Neuroprotection with Zuspan. Induction of labour for abortion was started with mifepristone after signing the informed consent form |
| OICU | ||
| Day 22 | Delivery surgery | The pregnancy was terminated at 23.4 weeks. Vaginal delivery care with cavity revision; uterine artery clamping with Zea technique. She presented uterine atony after expulsion of the product. Misoprostol 800 mcg and oxytocin 5 IU were administered. Male foetus was obtained, Ballard 23 weeks, weight 500 mg, size 25 cm. Placenta complete. Clear amniotic fluid. |
| Day 23 | MFM | Median peri-partum. Blood pressure in normal range. Restart of multi-target therapy (mycophenolate mofetil, hydroxychloroquine, tacrolimus and prednisone). Emotional and thanatological support was initiated for bereavement management. Couples counselling for bereaved parents. |
| Rheumatology | ||
| Psychology | ||
| Day 28 | MFM | Discharge |
MFM: maternal foetal medicine; OICU: obstetric intensive care unit.
Bioethical deliberation occurred at 23 weeks gestation: this was a non-viable pregnancy considering the infrastructure and resources available. By this time no favourable response was achieved, as the patient persisted with hypertension and required renal replacement therapy. The patient was informed on multiple occasions about the maternal and foetal risk of continuing with the pregnancy; she reported being aware and understanding the risk. Despite medical advice, she expressed her desire to continue with the pregnancy.
Four main actors in the dilemma were identified: the patient, her family, the health personnel and the institution. The family includes a 10-year-old daughter for whom the patient is the primary caregiver, as well as her mother and her husband as the primary economic provider. The health personnel involved included health professionals from different services, including psychology, social work and nursing. The hospital’s Legal Department and Bioethics Committee were involved as institutional representatives.
The possible costs in this case included clinical, family and economic costs. In addition, the socio-cultural context of the patient who, knowing the male sex of the product of her pregnancy, expressed the desire to give her husband a male child, became relevant. This is due to the burden given to motherhood in the social/cultural construction and the gender condition of women and pregnant women, placing reproduction at the centre of "duty" and personal fulfilment.4 In addition to this, there is the preference, especially of men, to have sons, whether for the preservation of the family name in a patrilineal system such as the Mexican one or due to other gender stereotypes.5 Therefore, even recognising the context, termination of pregnancy represented a cost to the patient's life plan.
The following central moral dilemma was established: How should one proceed, considering the risk to the patient's life and her desire to continue the pregnancy? Various normative systems can be applied to such a question.
Normative systemsUtilitarism. The consequences of the action represent the central component, which is why the greatest benefit must be sought at the lowest cost for the greatest number of people.6
In this case, termination of pregnancy seeks to safeguard the life of the mother and, considering only the consequence, saving one life represents a greater benefit than losing two. Taking into account the characteristics of the family nucleus, taking care of a premature newborn and a patient on renal replacement therapy would be complex and very costly. For the institution, safeguarding the mother would imply a more efficient use of human and material resources. From a utilitarian perspective, termination of pregnancy is justifiable.
Deontology. It focuses the importance of the decision on the action itself, which must be regulated by respect for autonomy.7 It is based on duty and the values of law and justice. In medicine, professional deontology focuses on the preservation of health, and therefore actions must be established in medical professional practice to guarantee this premise. In this case, it implies seeking all available therapeutic alternatives.
Termination of pregnancy would be justifiable, as such an action would preserve the patient's health. However, considering respect for the patient as an autonomous and dignified person, her expressed wish to continue with the pregnancy must be taken into account. If the actions are centred on autonomy, deontology would justify continuing the pregnancy even if the consequence is the death of the patient. It is concluded that, through the deontological system, both actions would be justifiable: to continue or not to continue with the pregnancy.
Virtue ethics. The focus of decisions lies with the person doing the action. The core values revolve around enhancing the human flourishing of the people involved.8
The flourishing of the patient and her family lies in preserving her life. In the case of the institution and the medical staff, it is about fulfilling their vocation in the service of life, so preserving the life of the patient would be appropriate, by ensuring her well-being on an individual level and decreasing maternal mortality on a more general level. In conclusion, virtue ethics would consider termination of pregnancy justifiable.
Medical reflectionThe experience of the treating staff in this case refers to the importance of assessing the patient's environment, her emotional, socio-economic and work status, her family and her values. The reflection also indicates a questioning of the ingrained idea among medical personnel that “the less we get involved, the better” or that medical knowledge is sufficient to acquire a position of authority in making decisions that are, in reality, ethically complex.
DiscussionThe comprehensive model is based on considering various ethical perspectives, so using this method for reflection allows us to generate a broad view of the dilemma beyond clinical factors, if the medical resources available to improve the patient's condition have been exhausted.9 In this case, we conclude that termination of pregnancy is justifiable and would be an appropriate solution to the dilemma presented (Fig. 1). However, taking into account the deep desire expressed by the patient to continue with her pregnancy, it would be essential that health personnel promote psycho-emotional accompaniment before, during and after the intervention in order for the intervention to be considered truly ethical.
One of the strengths of the comprehensive model is that it favours the participation of health personnel in reflection, which was directly expressed in this case. It is essential to recognise that health workers are affected by the difficult situations they face: their perspectives are required as moral agents as well as clinical experts.
ConclusionsCases such as the one discussed here can become paradigmatic, as it is a complex and problematic situation. In addition, the exercise of ethical analysis undertaken represents an opportunity for reflection on similar situations related to high-risk pregnancies in patients with a rheumatic diagnosis.
The particular experiences of rheumatic disease may give rise to specific dilemmas in treatment throughout life, including pregnancy. Since moral deliberation should not be universal or abstract but contextualised, it is important to be aware of the particular needs that arise in these cases.
FundingThis study received no funding.
Authors’ contributionTCG and AMdL contributed equally to the design, data collection, analysis and interpretation, writing and approval of the final version. ACLB and IPB participated in the study design and data analysis and approved the final version. GMR and JCdLC were involved in data interpretation and approval of the final version.
Conflict of interestsThe authors have no conflicts of interest to declare.
We thank the patient and her family for allowing her experience to be used as a learning exercise for health professionals. We thank Dr. Conrado García García for the facilities granted for access to the clinical information of the case.