PFAPA syndrome (periodic fever, aphthous stomatitis, pharyngitis and adenitis), or Marshall syndrome,1 is an autoinflammatory disease with no known genetic basis. It predominantly affects patients in the first decade of life. It is characterized by recurrent episodes of high fever of 3–6 days’ duration, accompanied by symptoms that define the condition: pharyngitis, cervical adenitis and aphthous stomatitis. The diagnosis is based on the clinical findings, and is reaffirmed by the elevation in acute phase reactants during the attacks, which returns to normal during asymptomatic periods, and negative results on microbiological tests. Although the episodes become increasingly less frequent until complete remission is achieved, the recurrence of the flares has a negative effect on the quality of life of the patient. The therapeutic options may have certain controversial aspects. Oral corticosteroids are the treatment of choice to resolve the attacks. However, after their use, an increase in the frequency of recurrence of the episodes has been reported.2 Tonsillectomy is performed in cases of refractory disease, but its use is questionable, given that the majority of the patients eventually achieve complete remission. Different drugs, like cimetidine and colchicine, have been employed as prophylaxis in the attempt to reduce the number and severity of the episodes.3 In recent years, a possible relationship between PFAPA syndrome and low serum vitamin D levels is being studied, and the question has been raised as to whether treatment with this vitamin could modify the course of the disease.4
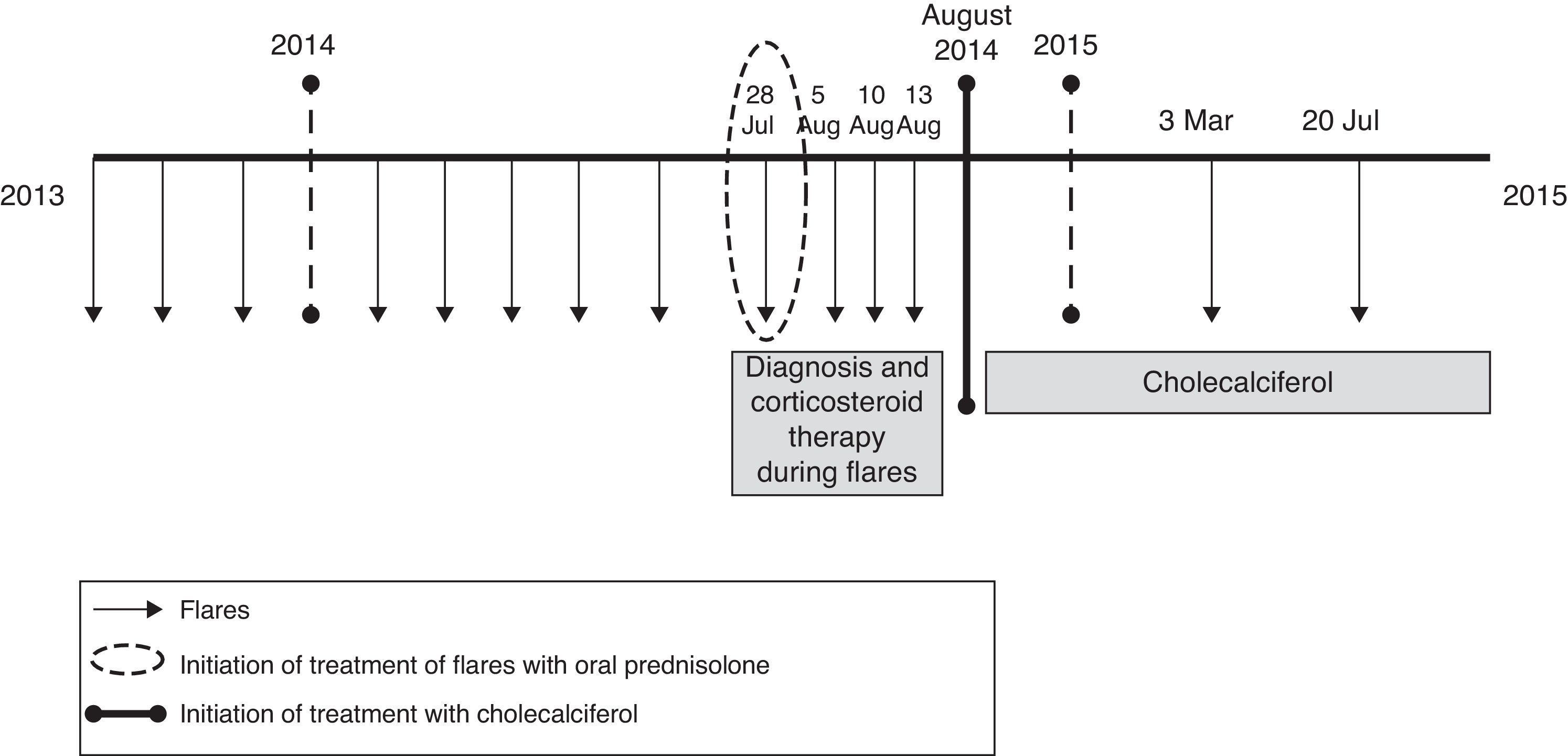
We report the case of a 32-month-old girl with a previous history of multiple visits to the emergency department due to episodes of fever, vomiting and recurrent tonsillitis, which occurred every 6–8 weeks. During these episodes, she had a transient elevation of acute phase reactants (maximum C-reactive protein: 15.39mg/dL) and of leukocytes of up to 15,000/μL with 85% neutrophils, and negative microbiological tests. As PFAPA syndrome was suspected, in one of the flares, she was given a single dose of oral prednisolone (1mg/kg/dose) as a diagnostic-therapeutic test, and the symptoms resolved immediately. It was observed that, after several flares in which she was treated with corticosteroids, the episodes became increasingly frequent. The serum 25-OH-vitamin D level was determined, and was found to be deficient (23.7ng/mL). Treatment was begun with 400IU of cholecalciferol and was maintained until the patient achieved a normal serum vitamin D level (40ng/mL). Since the initiation of treatment she has experienced a reduction in the number and severity of the episodes (Fig. 1), and had only 2 mild attacks over the following 12 months.
In recent years, we have begun to realize the importance of the role of vitamin D as an immune modulator.5 Several epidemiological studies have focused on determining the correlation between vitamin D deficiency and the risk of inflammatory diseases, including allergic and autoimmune disorders,6,7 and the possibility that vitamin D could be a therapeutic option in some of these diseases is being taken into consideration.8 Uncontrolled studies have found that, in patients with PFAPA, vitamin D therapy reduces the number, duration and severity of the episodes.9 However, there are no clinical trials comparing vitamin D with other therapeutic options or placebo. With our current level of knowledge, it is impossible to determine whether the favorable outcome is due to the treatment or to the natural course of the disease. Moreover, the dose of vitamin D and the required duration of treatment have yet to be defined. Therefore, in our patient, we opted for a standard dose until her serum 25-OH-vitamin D level had returned to normal. Despite these limitations, the use this therapy can be considered in patients with PFAPA with vitamin D deficiency, above all, because of its safety profile as compared to other therapeutic alternatives.
Please cite this article as: Rico Rodes A, Sabrido Bermúdez G, Llombart Vidal A, Alcalá Minagorre PJ. Síndrome de fiebre periódica, estomatitis aftosa, faringitis y adenopatías y vitamina D. ¿Una posible opción terapéutica? Reumatol Clin. 2016;12:363–364.