The patient was a 56-year-old man with microscopic polyangiitis and symmetrical peripheral polyneuropathy of the extremities who was positive for p-ANCA, EMG pattern of mononeuritis multiplex and skin biopsy showing the presence of nonspecific vasculitis. He had phlebectasia with plethora and tortuous vessels on dorsum of the fingers on both hands, paresis and hypoesthesia of fingers and toes with functional limitations. The administration of prednisone, azathioprine and a cyclophosphamide pulse achieved rapid improvement in the general symptoms, but the changes in the neuropathy occurred very slowly. After 47 months of treatment, he had mild phlebectasia in fingers and slight hypoesthesia in hands and feet, with normal laboratory tests. Phlebectasia was probably the result of an autonomic dysfunction due to vasculitis of the vasa nervorum and could be a sign to look for in similar cases.
Paciente masculino de 56 años con poliangitis microscópica y polineuropatía periférica simétrica de extremidades con p-ANCA positivo, patrón EMG de mononeuritis múltiple y biopsia cutánea con vasculitis inespecífica, quien presentaba flebectasia con plétora y trayectos tortuosos en el dorso de los dedos en ambas manos, paresia e hipoestesia digital en manos y pies con limitación funcional. Mediante la administración de prednisona, azatioprina y pulso de ciclofosfamida, mejoró rápidamente de los síntomas generales pero muy lentamente de la neuropatía. Después de 47 meses de evolución persiste discreta flebectasia digital en manos y ligera hipoestesia en manos y pies, con parámetros de laboratorio normales. La flebectasia, probablemente, fue el resultado de una disautonomía por vasculitis de la vasa nervorum y podría ser un signo a ratificar en casos semejantes.
Microscopic polyangiitis (MPA) predominantly affects males (1.8:1), with onset between the ages of 50 and 60 years, with an annual incidence of 2.6–11.6 cases per million inhabitants and a prevalence of 2–3 cases per 100,000 inhabitants. The course of the disease is chronic, with the possibility of recurrence. Forty-three percent of cases have neurological impairment, with peripheral polyneuropathy distribution (PPN), distal and symmetrical with dysaesthesias and digital paresis, principally in the territories of the terminal branches of the peroneal and ulnar nerves, due to vasculitis of the vasa nervorum.1–3 Other common manifestations are: flu-like syndrome (92%), kidney (74%), skin (46%) and lung (45%). Fifty to seventy percent of cases have anti-cytoplasmic neutrophil antibodies, associated anti-myelopolymerase (MPO), with perinuclear (p-ANCA) staining. Outcomes will depend on appropriate treatment according to the severity of the case, with 70% survival at 5 years.
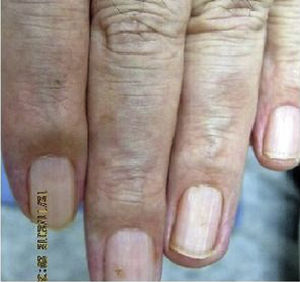
Clinical CaseA 56-year-old male patient hospitalised at the end of 2012 with a diagnosis of MPA with distal symmetrical PNP of the extremities, positive serology for p-ANCA (1:160), electromyography with a multiple mononeuritis pattern, and skin biopsy with non-specific vasculitis. On examination he had phlebectasia with plethora and tortuous vessels on the dorsum of the second to fourth fingers of both hands (Fig. 1) and paresis and hypoaesthesia of fingers and toes with grip and gait limitation. Mild and transient elevation of uraemia and albuminuria with erythrocyturia. He was treated with prednisone, azathioprine and pulse cyclophosphamide, with rapid improvement of the general symptoms and very slow improvement of the neuropathy manifestations. The digital phlebectasia was of a reversible course, and was minimal after 47 months’ follow-up (Fig. 2), but a mild digital hypoaesthesia persists in the hands and feet. The lab test results are normal, with negative p-ANCA. He continued on a maintenance dose of prednisone and azathioprine.
DiscussionThe diagnosis of MPA was well documented according to the classification of the 2012 Revised International Chapel Hill Consensus Conference Nomenclature4; the peripheral motor and sensory neurological manifestations were relevant due to impairment of the terminal branches of the median, ulnar and peroneal nerves, bilateral, attributable to necrosing vasculitis of the vasa nervorum as a pathophysiological mechanism in MPA. The digital phlebectasia was probably a result of concomitant neurovegetative vasomotor innervation, which subsequently involuted parallel to the sensory-motor neurological symptoms. Ratifying this finding in similar cases it could be given diagnostic value, since it has not been described in PNPs that are metabolic, toxic, infectious, immunological, paraneoplastic, iatrogenic etc. that present with dysautonomia, but at other levels and with different pathophysiologies.5–7
Ethical DisclosuresProtection of people and animalsThe authors declare that no experiments were performed on humans or animals for this investigation.
Data confidentialityThe authors declare that they have followed the protocols of their work centre on the publication of patient data.
Right to privacy and informed consentThe authors declare that no patient data appears in this article, and that the patient gave their informed consent.
Conflict of InterestsThe authors have no conflict of interests to declare.
Please cite this article as: Badía Flores JJ, Arévalo Martínez FG. Flebectasia digital en un caso de poliangitis microscópica con polineuropatía periférica. Reumatol Clin. 2019;15:368–369.