Pleuroparenchymal fibroelastosis (PPFE) is a new entity that was recently included in the group of rare or infrequent idiopathic interstitial pneumonias.1 It is characterised by the development of an elastic fibre-rich fibrosis that affects the pleura and subpleural pulmonary parenchyma, predominantly in the upper lobes.2 It may be idiopathic or secondary to multiple processes, including systemic autoimmune diseases.3
We present the case of a 52 year old women from Peru who has lived in Spain for 23 years. She works as a home help and has no relevant family or personal history. A year ago arthralgia when moving commenced together with xerostomy but without xerophthalmia or any other associated symptom. Physical examination, cardiopulmonary auscultation and musculoskeletal and cutaneous examination were normal. Haemogram, general biochemistry and creatine kinase (111 U/l) were normal. IgG immunoglobulin in serum was raised (2.410 mg/dl). FR was positive (242 UI/mL), ACPA was negative, ANA was positive (1/640), anti-Ro was positive (240 UI/mL), anti-La was positive (75 UI/mL) and anti-DNA was negative. The following complementary tests were requested: serological tests for VHC and VHB, Interferon Gamma Release Assay (IGRA), sacroiliac X-ray imaging, echocardiogram, specific myopathy antibodies (anti-MI2, anti-SRP, anti-PM-SCL, anti-PL7, anti-PL12, anti-KU, anti-OJ and anti-EJ) and capillaroscopy, all of which were normal or negative.
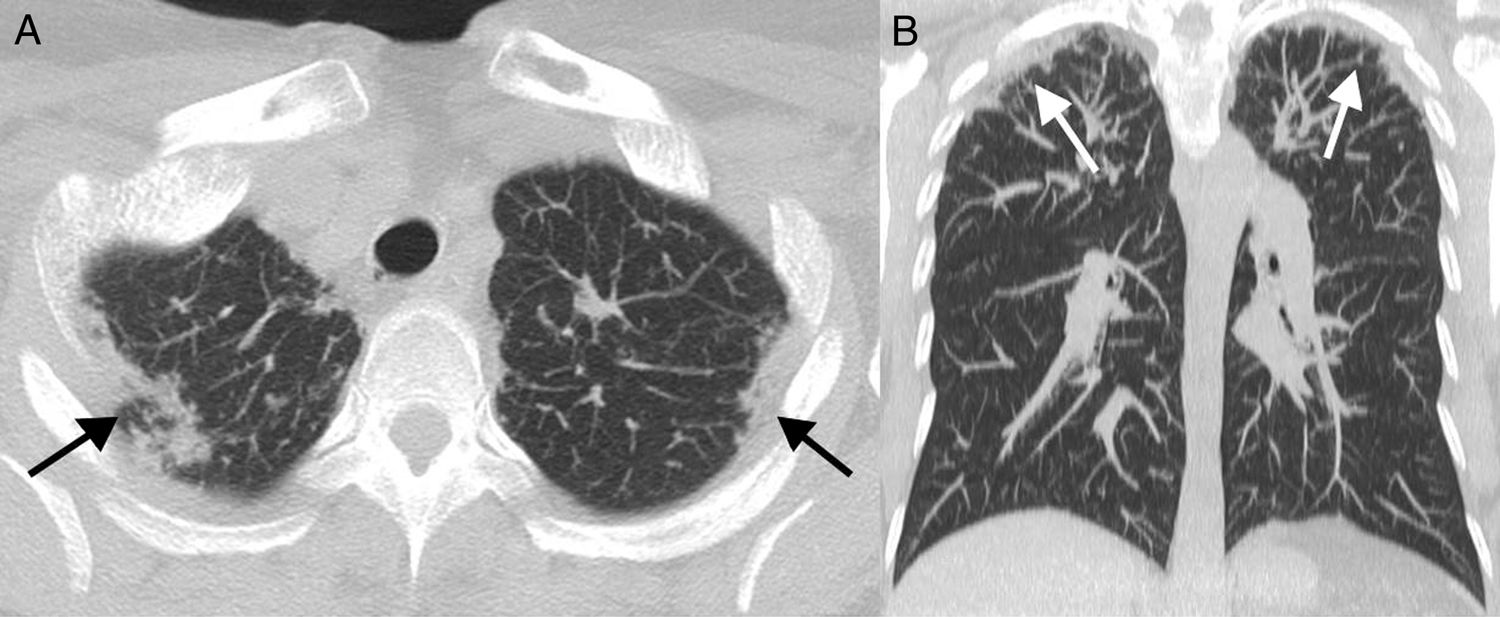
Salivary gland biopsy revealed the presence of multiple areas of lymphocyte infiltration. She was diagnosed primary Sjögren syndrome on the basis of ACR-EULAR 2017 criteria.4 Thoracic X-ray imaging showed pleural thickening and fibrosis in the apical cap, and pulmonary TCA imaging showed subpleural consolidations together with predominantly bilateral apical pleural thickening, leading to a moderate loss of volume in both upper lobes, all of which is compatible with PPFE (Fig. 1). Respiratory function tests including CO diffusion were normal.
Treatment commenced with 5 mg/day prednisone, in spite of which the patient described worsening of the xerostomy and a subjective sensation of dyspnoea during moderate efforts. A second pulmonary CTA showed no radiological progression after a 6 month follow-up.
PPFE was first described in 1992 by Amitani et al. as idiopathic pulmonary fibrosis of the upper fields, and in 2004 it was recognised by Frankel et al. as a new clinical-pathological entity. Since then approximately 120 cases have been described worldwide, above all in Asiatic populations.5 Of all these cases, about 20% were associated with connective tissue pathologies.6In 2013 this entity was included in the classification of idiopathic interstitial pneumonias of the American Thoracic Society/European Respiratory Society, within the category of rare interstitial pneumonias.1
This disease occurs in adults with an average age of around 57 years, affecting both sexes equally1 and without showing any association with smoking.3,5 Its symptoms are usually dyspnoea, unproductive cough, pleuritic pain or weight loss.7 This entity may be idiopathic or secondary to multiple processes: infections, radiation, transplant or neoplasias, including rheumatological diseases3 such as rheumatoid arthritis, myopathies, scleroderma or Sjögren's syndrome.6
The characteristic findings in CTA imaging are the bilateral presence of irregular pleural thickening and fibrotic changes in upper fields of the subpleural parenchyma, and it may coexist with other radiological patterns of pulmonary interstitial disease in different areas of the parenchyma. Anatomic-pathological findings are the presence of pleural and intra-alveolar fibrosis together with elastosis of the alveolar septa.8
Patients with PPFE are at higher risk of pneumomediastinum or pneumothorax,6 either spontaneously or after a pulmonary biopsy for definitive diagnosis based on anatomopathological findings.9 This is why the utility of cryobiopsy as a less invasive diagnostic technique is being evaluated, as it reduces complications of this type.7 Differential diagnosis must be considered against other entities which are found radiologically to predominantly affect the upper lobes, including sarcoidosis or tuberculosis.
PPFE has a highly variable prognosis, and its evolution is sometimes extremely severe.6 Although a case has been described that improved with pirfenidone,10 in general there is no effective treatment. The main causes of death are the progression of the disease and respiratory infections.6 Three cases have been published to date in Spain, all of which evolved unfavourably and required lung transplant.7,9
To conclude, PPFE is a new entity that has recently been included among the interstitial lung diseases, and it may be associated with systemic autoimmune diseases. This is why it is important to be aware of its clinical and radiological characteristics, suspecting it in patients with interstitial pulmonary involvement that is predominantly in the upper fields. It is also highly important to use a multidisciplinary approach to improve its detection and treatment.
We would like to thank the Radiodiagnostic Department of Ramón y Cajal Hospital for their collaboration.
Please cite this article as: Morán Álvarez P, Bachiller-Corral J, Gorospe Sarasúa L, de la Puente Bujidos C. Fibroelastosis pleuroparenquimatosa: un nuevo tipo de neumonía instersticial asociada a conectivopatías. Reumatol Clin. 2020;16:513–514.