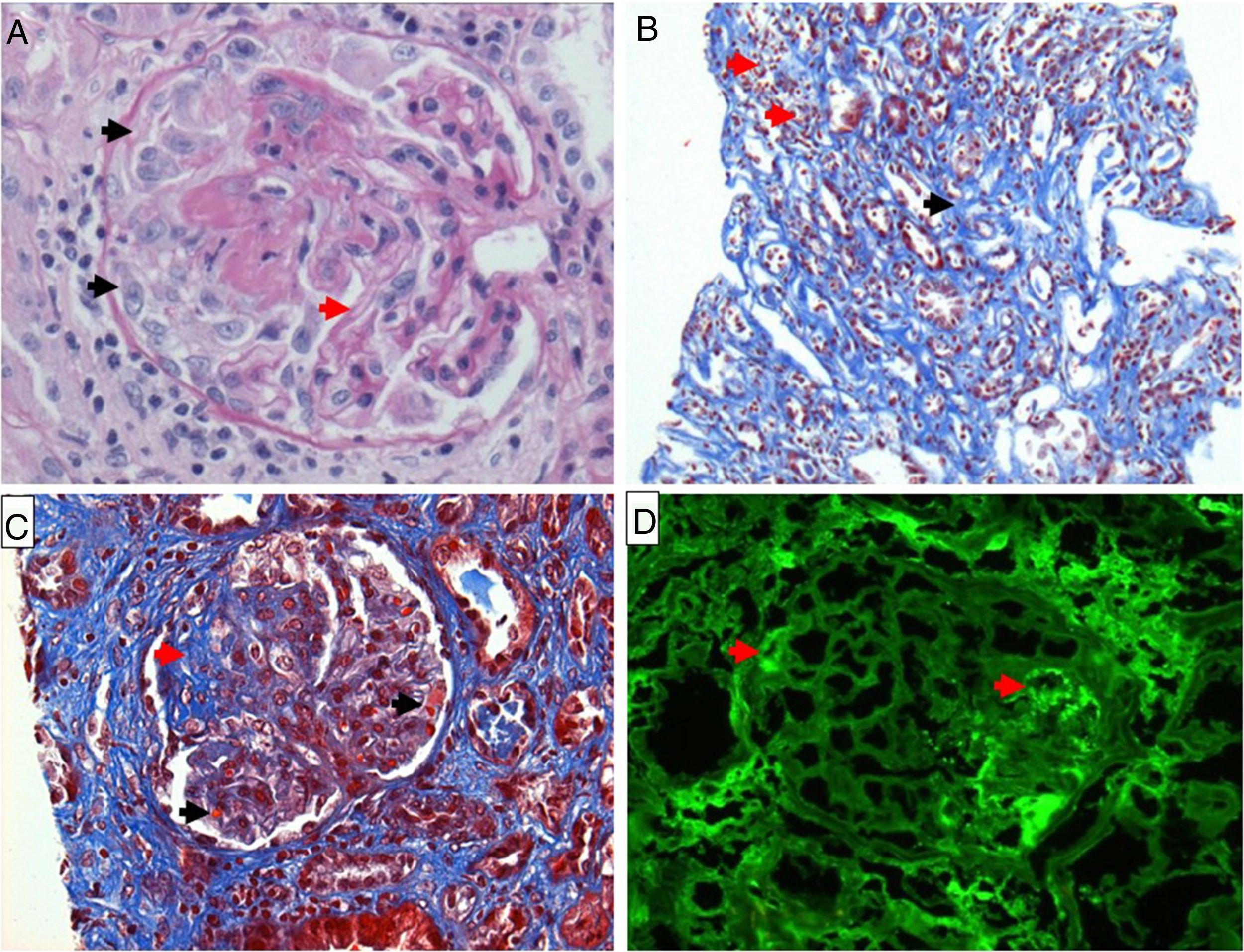
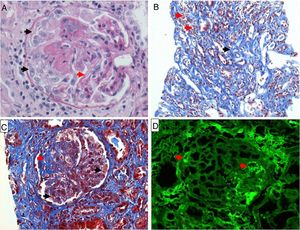
We present a case of a 38-year-old female with a history of right posterior ankle pain for 2 months which worsened with walking and standing up for a long time. There were no complaints in other joints. On physical examination the patient presented swelling of the posterior ankle and complained of pain with forced flexion of the right feet. There was no increase of inflammation parameters in blood tests. Radiographic lateral view of the right ankle demonstrated an enlarged Stieda's process (Fig. 1). The magnetic resonance imaging (MRI) of the right ankle confirmed the Stieda's process (Fig. 1) being able to originate posterior conflict, with a subtle bone marrow edema. A slight effusion was observed in the anterior and posterior compartments of the tibiotalar joint as well as edema of the subcutaneous fat. The patient was told to rest and NSAID were prescribed with resolution of the hindfoot pain.
The posterior ankle impingement syndrome is a condition resulting from soft tissue compression between the posterior process of the calcaneus and the posterior tibia during ankle plantar flexion.1 An important cause of the syndrome is a prominent posterolateral talar process (Stieda's process) or the presence of os trigonum, due to its impact on adjacent structures.2 Patients usually report chronic or recurrent posterior ankle pain caused or exacerbated by forced plantar flexion.3 Other causes of this syndrome may result from flexor hallucis longus tenosynovitis, ankle osteochondritis, subtalar joint disease, and fracture. Diagnosis of posterior ankle impingement syndrome is based primarily on clinical history and physical examination. Radiography, computed tomography, and MRI are useful to detect associated bone and soft-tissue abnormalities.3 MRI can identify the presence of a Stieda's process or a separate os trigonum in addition to secondary findings that suggest posterior ankle impingement as well as: increased signal intensity in the soft tissues posterior to the ankle, thickening of the posterior joint capsule, posterior and subtalar synovitis, flexor hallucis longus tenosynovitis and bone marrow edema pattern in the os trigonum and posterior talus.4•7 Symptoms typically improve with nonsurgical management but surgery may be required in refractory cases. A literature review on conservative treatment of the posterior ankle impingement syndrome suggests that the initial treatment should aim at decreasing inflammation with non-steroidal anti-inflammatory drugs and activity restriction (avoidance of forced plantar flexion).8 Furthermore, a physiotherapy program that includes soft tissue therapy, stretching and mobilizations of restricted joints of the lower kinetic chain should be implemented in conjunction with a progressive strengthening, balance and proprioception enhancement program.8,9 Cortisone injections can be performed in patients with higher levels of pain. These injections into the affected area may reduce the pain and allow the patient to progress into a rehabilitation program.10 It is also suggested to tape or brace the ankle in a protective dorsiflexion position when the patient undertakes intense activities, such as sports.2
This case emphasizes the importance of considering posterior ankle impingement due to a Stieda's process of the talus as a cause of hindfoot pain. In fact, it is an underrecognized cause of posterior ankle pain but imaging can easily make the diagnosis and guide appropriate treatment.
Conflict of interestThe authors declare that they have no conflicts of interest.