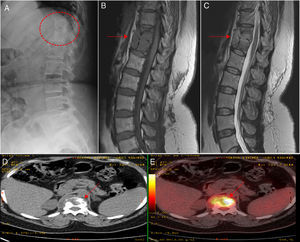
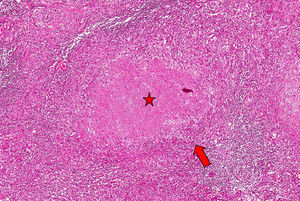
The patient was a 42-year-old woman with controlled intrinsic asthma, receiving chronic treatment with inhaled corticosteroids, but not requiring systemic corticosteroid therapy on a regular basis. Three years before the present consultation, she had undergone chemotherapy with isoniazid for 12 months after a positive Mantoux test, with no evidence of active disease, after being in contact with a relative who had pulmonary tuberculosis. She was admitted with a 3-month history of symptoms including mixed low back pain, with night sweats and a feverish sensation. The radiographic study revealed bone rarefaction in thoracic vertebral bodies T11 and T12, but no changes in lung parenchyma or presence of mediastinal adenopathy. Notable findings in the complementary tests were hemoglobin 11.6g/dL, erythrocyte sedimentation rate 35mm/h, C-reactive protein 1.49mg/dL (normal value<0.5mg/dL) and negative HIV test. Magnetic resonance revealed evidence of spondylodiscitis with a bilateral paravertebral and anterior epidural abscess that affected vertebral bodies T11–T12, a finding confirmed in a metabolic study carried out by positron emission tomography (Fig. 1). The microscopic study and culture of sputum, as well as blood and urine cultures, were negative, even for mycobacteria. As tuberculous spondylodiscitis (TSD) was suspected, the decision was made to perform a computed tomography-guided biopsy and begin treatment with isoniazid, rifampicin, pyrazinamide and ethambutol; analgesia with weak opioids; and the use of rigid orthosis for the lumbar spine. The histopathological study of the lesion revealed the presence of caseating granulomas suggestive of a tuberculous process, although Ziehl-Neelsen staining was negative (Fig. 2). After 12 months of antituberculous therapy, the patient's course was satisfactory, with no sequelae or limited axial mobility.
(A) The radiological study shows bone rarefaction in thoracic vertebral bodies T11 and T12, with marked erosion of their anterior borders. (B) Magnetic resonance study shows a lobulated lesion and collection affecting T11, T12 and their respective intervertebral disc (arrow), which is hypointense on a T1-weighted image. (C) Magnetic resonance study showing hyperintensity on a T2-weighted image (solid arrows). (D and E) Positron emission tomography images confirming the high metabolic activity of the lesions (broken arrows).
Spondylodiscitis is an infection, generally bacterial, that affects the vertebral bodies and their respective adjacent discs, leading to the destruction, instability and subsequent ankylosis of the affected structures.1 The incidence is estimated to be 2.4–6 cases/100000 population/year, with a mortality rate of around 5%.2 The determinant risk factors are the increased life expectancy, the presence of previous vertebral lesions, the presence of immunodeficiency, the use of immunosuppressive therapy and the use of intravascular devices.3–5
Skeletal tuberculosis represents 20% of overall extrapulmonary cases; vertebral involvement or Pott's disease accounts for 50% of the cases affecting the skeleton and from 1% to 5% of all infections by Mycobacterium tuberculosis.6 The spine is the site most frequently involved.7
Tuberculous spondylodiscitis is a rare but very serious clinical condition that can result in a severe deformity and early neurological complications. Despite the present availability of a greater number of effective complementary tests, the diagnosis of TSD continues to be difficult and requires a high index of clinical suspicion.8 The disease can take the form of disseminated tuberculosis or endogenous reactivation of a latent focus.9 Treatment is basically medical, consisting of the tuberculostatic drugs usually employed in pulmonary tuberculosis infection (isoniazid, rifampicin, pyrazinamide or ethambutol), and the mean duration is 12 months.8
Ethical DisclosuresProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of dataThe authors declare that no patient data appear in this article.
Right to privacy and informed consentThe authors declare that no patient data appear in this article.
Conflicts of InterestThe authors declare they have no conflicts of interest.
We thank the Nuclear Medicine and Radiology Departments of Hospital General Universitario de Ciudad Real, Spain, for their collaboration and the facilities they made available to us for the preparation of the present article.
Please cite this article as: Ramírez Huaranga MA, Arenal López R, Anino Fernández J, Villasanti Rivas N. Mal de Pott: una causa infrecuente de dolor dorsolumbar en nuestros días. Reumatol Clin. 2016;12:109–111.