Scabies is a parasitosis caused by Sarcoptes scabiei var. hominis; Norwegian scabies is a rare, highly contagious subtype that is common in immunosuppressed patients.
Case ReportThe patient was an 82-year-old woman with a history of hypertension, insulin-dependent diabetes mellitus and polymyalgia rheumatica, being treated with oral corticosteroids. She was referred to the dermatology department with a 9-month history of generalized pruritus, accompanied by hyperkeratotic plaques and numerous lesions in the form of linear burrows, predominantly on her scalp and breasts and in the interdigital spaces of both hands.1 She had applied topical corticosteroids, which had had a negative effect on her clinical status.2 It was also interesting to know that individuals with whom she lived were also affected (Figs. 1 and 2).
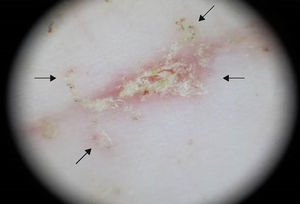
The suspected diagnosis was reached on the basis of the clinical signs and the results of dermatoscopic examination. The microscopic study of skin scales disclosed the presence of mites and their feces and eggs, and the diagnosis was confirmed. It important to include diseases such as ichthyosis and psoriasis in the differential diagnosis (Figs. 3–5).
Treatment is based on oral ivermectin, 5% salicylate vaseline in hyperkeratotic lesions and, in certain lesions, surgical debridement to facilitate the penetration of the topical treatment.
As a result of her comorbidities, the patient died of a respiratory tract infection before treatment for scabies could be initiated.
DiscussionWhen a patient receiving immunosuppressive therapy has generalized pruritus—predominantly at night—with crusted lesions,3 and the individuals with whom the patient lives are affected, it is essential to perform a differential diagnosis that includes Norwegian scabies, which occurs relatively frequently in these individuals. Moreover, the incidence is rising as a consequence of the increasingly widespread use of immunosuppressive agents.
Ethical DisclosuresProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of dataThe authors declare that they have followed the protocols of their work center on the publication of patient data.
Right to privacy and informed consentThe authors declare that no patient data appear in this article.
Conflicts of InterestThe authors declare they have no conflicts of interest.
The authors thank Juan Carlos Álvarez of the Pathology Department of Complejo Hospitalario Universitario de Ferrol. Ferrol Health Area, SERGAS, Ferrol, A Coruña, Spain.
Please cite this article as: Varela-Veiga A, Vilas-Sueiro A, Monteagudo B, Fernández-Jorge B. Lesiones hiperqueratósicas y prurito en paciente inmunodeprimida. Reumatol Clin. 2016;12:107–108.