In order to agree on the fundamental aspects related to the management of pregnancy in patients with systemic lupus erythematosus (SLE) and antiphospholipid syndrome (APS), the Spanish Societies of Gynaecology and Obstetrics, Internal Medicine and Rheumatology set up a working group for the preparation of three consensus documents.
MethodsEach of the Scientific Societies involved proposed five representatives based on their experience in the field of pregnancy control in patients with autoimmune diseases. The recommendations were developed following the Delphi methodology.
ResultsThis second document contains the recommendations regarding the management of pregnancy in women with SLE and APS, including complications such as lupus activity, congenital heart block, thrombotic and obstetric manifestations of APS and placental vascular disease.
ConclusionsThese multidisciplinary recommendations are considered decision-making tools for clinicians involved in the care of patients with SLE/APS during pregnancy.
Las sociedades españolas de ginecología y obstetricia, de medicina interna y de reumatología han constituido un grupo de trabajo paritario para la elaboración de 3 documentos de consenso sobre el control del embarazo en mujeres con lupus eritematoso sistémico (LES) y síndrome antifosfolípido (SAF).
MétodosCada una de las sociedades científicas implicadas propuso 5 representantes en base a su experiencia en el área del control del embarazo en pacientes con enfermedades autoinmunes. Las recomendaciones se elaboraron siguiendo la metodología Delphi.
ResultadosEn este segundo documento se incluyen las recomendaciones que abordan el manejo del embarazo normal y sus complicaciones en mujeres con LES/SAF. Se presentan las recomendaciones relacionadas con el seguimiento del embarazo, la actividad lúpica, el bloqueo cardíaco congénito, las manifestaciones trombóticas y obstétricas del SAF y los defectos de placentación.
ConclusionesEstas recomendaciones multidisciplinares se consideran herramientas en la toma de decisiones para los clínicos involucrados en la asistencia a pacientes con LES/SAF durante el embarazo.
Following on from the first part on preconception assessment, infertility and ovarian preservation, this second document specifically addresses the control of the patient from time of conception to delivery. Issues relating to the basic follow-up of the pregnancy and the treatment of the different complications are raised, those directly related to systemic lupus erythematosus (SLE) and antiphospholipid syndrome (APS) and those associated with placental defects and vascular complications, which are a particular risk in these conditions.
Material and methodsAs detailed in the first part of this consensus document, the recommendations were drawn up following the Delphi methodology. The specific working group for this section included 2 representatives from the Spanish Society of Gynaecology and Obstetrics (SEGO), 2 from the Systemic Autoimmune Diseases Group (GEAS) of the Spanish Society of Internal Medicine (SEMI) and 2 from the Spanish Society of Rheumatology (SER), as well as a coordinator.
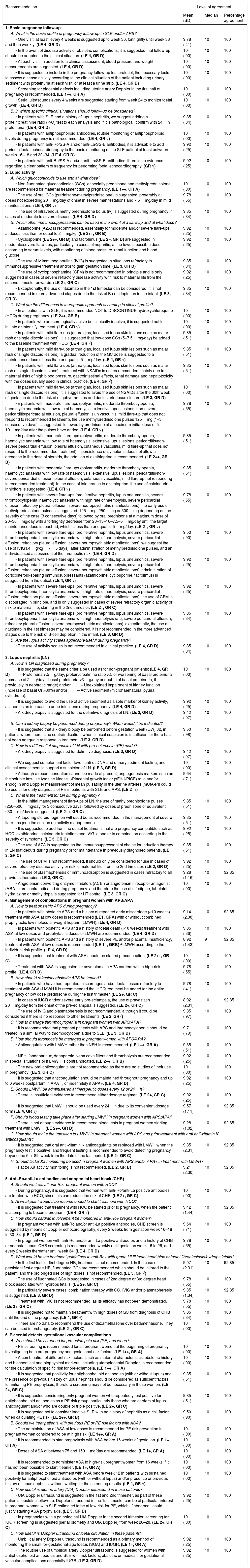
Final consensus documentAll the recommendations are contained in Table 1.
Recommendations on pregnancy control in patients with systemic lupus erythematosus and antiphospholipid syndrome.
| Recommendation | Level of agreement | ||
|---|---|---|---|
| Mean (SD) | Median | Percentage agreement | |
| 1. Basic pregnancy follow-up | |||
| A. What is the basic profile of pregnancy follow-up in SLE and/or APS? | |||
| • One visit, at least, every 4 weeks is suggested up to week 36, fortnightly until week 38 and then weekly. (LE 4, GR D) | 9.78 (.41) | 10 | 100 |
| • In the event of disease activity or obstetric complications, it is suggested that follow-up should be adapted to the clinical situation. (LE 4, GR D) | 10 (.00) | 10 | 100 |
| • At each visit, in addition to a clinical assessment, blood pressure and weight measurements are suggested. (LE 4, GR D) | 10 (.00) | 10 | 100 |
| • It is suggested to include in the pregnancy follow-up test protocol, the necessary tests to assess disease activity according to the clinical situation of the patient including urinary sediment with proteinuria at each visit, or at least a urine strip. (LE 4, GR D) | 10 (.00) | 10 | 100 |
| • Screening for placental defects including uterine artery Doppler in the first half of pregnancy is recommended. (LE 1++, GR A) | 10 (.00) | 10 | 100 |
| • Serial ultrasounds every 4 weeks are suggested starting from week 24 to monitor foetal growth. (LE 4, GR D) | 10 (.00) | 10 | 100 |
| B. In which specific clinical situations should follow-up be broadened? | |||
| • In patients with SLE and a history of lupus nephritis, we suggest adding a protein:creatinine ratio (P/C) test to each analysis and if it is pathological, confirm with 24h proteinuria. (LE 4, GR D) | 9.85 (.34) | 10 | 100 |
| • In patients with antiphospholipid antibodies, routine monitoring of antiphospholipid levels during pregnancy is not recommended. (LE 4, GR √) | 10 (.00) | 10 | 100 |
| • In patients with anti-Ro/SS-A and/or anti-La/SS-B antibodies, it is advisable to add periodic foetal echocardiography to the basic monitoring of the SLE patient at least between weeks 16–18 and 30–34. (LE 4, GR D) | 9.92 (.25) | 10 | 100 |
| • In patients with anti-Ro/SS-A and/or anti-La/SS-B antibodies, there is no evidence regarding a clear pattern of frequency for performing foetal echocardiography. (GR √) | 9.92 (.25) | 10 | 100 |
| 2. Lupic activity | |||
| A. Which glucocorticoids to use and at what dose? | |||
| • Non-fluorinated glucocorticoids (GCs), especially prednisone and methylprednisolone, are recommended for maternal treatment during pregnancy. (LE 1++, GR A) | 10 (.00) | 10 | 100 |
| • The use of oral GCs (prednisone/methylprednisolone) is suggested, preferably at doses not exceeding 20mg/day of onset in severe manifestations and 7.5mg/day in mild manifestations. (LE 4, GR √) | 9.78 (.55) | 10 | 100 |
| • The use of intravenous methylprednisolone bolus (iv) is suggested during pregnancy in cases of moderate to severe disease. (LE 4, GR D) | 9.85 (.34) | 10 | 100 |
| B. Which other immunosuppressants can be used in the event of a flare-up and at what dose? | |||
| • Azathioprine (AZA) is recommended, essentially for moderate and/or severe flare-ups, at doses less than or equal to 2mg/kg. (LE 2++, GR B) | 9.92 (.25) | 10 | 100 |
| • Cyclosporine (LE 2++, GR B) and tacrolimus (LE 2−, GR D) are suggested in moderate/severe flare-ups, particularly in cases of nephritis, at the lowest possible dose according to serum levels, with monitoring of blood pressure, renal function and blood glucose. | 9.92 (.25) | 10 | 100 |
| • The use of iv immunoglobulins (IVIG) is suggested in situations refractory to immunosuppressive treatment and/or to gain gestation time. (LE 3, GR D) | 9.85 (.34) | 10 | 100 |
| • The use of cyclophosphamide (CFM) is not recommended in principle and is only suggested in cases of severe refractory disease activity with risk to maternal life from the second trimester onwards. (LE 2+, GR C) | 9.92 (.25) | 10 | 100 |
| • Exceptionally, the use of rituximab in the 1st trimester can be considered. It is not recommended in more advanced stages due to the risk of B-cell depletion in the infant. (LE 3, GR D) | 9.85 (.34) | 10 | 100 |
| C. What are the differences in therapeutic approach according to clinical profile? | |||
| • In all patients with SLE, it is recommended NOT to DISCONTINUE hydroxychloroquine (HCQ) during pregnancy. (LE 2++, GR B) | 10 (.00) | 10 | 100 |
| • In patients who are serologically active but clinically inactive, it is suggested not to initiate or intensify treatment. (LE 4, GR √) | 10 (.00) | 10 | 100 |
| • In patients with mild flare-ups (arthralgias, localised lupus skin lesions such as malar rash or single discoid lesions), it is suggested that low-dose GCs (5–7.5mg/day) be added to the baseline treatment with HCQ. (LE 4, GR √) | 9.85 (.51) | 10 | 100 |
| • In patients with mild flare-ups (arthralgias, localised lupus skin lesions such as malar rash or single discoid lesions), a gradual reduction of the GC dose is suggested to a maintenance dose of less than or equal to 5mg/day. (LE 4, GR √) | 9.85 (.51) | 10 | 100 |
| • In patients with mild flare-ups (arthralgias, localised lupus skin lesions such as malar rash or single discoid lesions), treatment with NSAIDs is not recommended, mainly due to maternal risks of high blood pressure, gastrointestinal effects, renal damage and hepatotoxicity with the doses usually used in clinical practice. (LE 4, GR √) | 9.85 (.51) | 10 | 100 |
| • In patients with mild flare-ups (arthralgias, localised lupus skin lesions such as malar rash or single discoid lesions), it is suggested to avoid the use of NSAIDs after the 30th week of gestation due to the risk of oligohydramnios and ductus arteriosus closure. (LE 3, GR D) | 10 (.00) | 10 | 100 |
| • n patients with moderate flare-ups (polyarthritis, moderate thrombocytopenia, haemolytic anaemia with low rate of haemolysis, extensive lupus lesions, non-severe pericarditis/pericardial effusion, pleural effusion, skin vasculitis, mild flare-up that does not respond to recommended treatment), the use methylprednisolone pulses 125mg (1–3 consecutive days) is suggested, followed by prednisone at a maximum initial dose of 5–10mg/day after the pulses have ended. (LE 4, GR √) | 9.78 (.55) | 10 | 100 |
| • In patients with moderate flare-ups (polyarthritis, moderate thrombocytopenia, haemolytic anaemia with low rate of haemolysis, extensive lupus lesions, pericarditis/non-severe pericardial effusion, pleural effusion, cutaneous vasculitis, mild flare-up that does not respond to the recommended treatment), if persistence of symptoms does not allow a decrease in the dose of steroids, the addition of azathioprine is recommended. (LE 2++, GR B) | 9.85 (.51) | 10 | 100 |
| • In patients with moderate flare-ups (polyarthritis, moderate thrombocytopenia, haemolytic anaemia with low rate of haemolysis, extensive lupus lesions, pericarditis/non-severe pericardial effusion, pleural effusion, cutaneous vasculitis, mild flare-up not responding to recommended treatment), in the case of intolerance to azathioprine, the use of calcineurin inhibitors is suggested. (LE 4, GR √) | 9.85 (.51) | 10 | 100 |
| • In patients with severe flare-ups (proliferative nephritis, lupus pneumonitis, severe thrombocytopenia, haemolytic anaemia with high rate of haemolysis, severe pericardial effusion, refractory pleural effusion, severe neuropsychiatric manifestations), the early use of methylprednisolone pulses is suggested, 125mg, 250mg or 500mg depending on the severity of the case (3 consecutive days) followed by oral prednisone at a maximum dose of 20–30mg/day with a fortnightly decrease from 20–15–10–7.5–5mg/day until the target maintenance dose is reached, which is less than or equal to 5mg/day. (LE 2−, GR √) | 9.78 (.55) | 10 | 100 |
| • In patients with severe flare-ups (proliferative nephritis, lupus pneumonitis, severe thrombocytopenia, haemolytic anaemia with high rate of haemolysis, severe pericardial effusion, refractory pleural effusion, severe neuropsychiatric manifestations), we suggest the use of IVIG (.4g/kg×5 days), after administration of methylprednisolone pulses, and an individualised assessment of the thrombotic risk. (LE 4, GR D) | 9.50 (.90) | 10 | 100 |
| • In patients with severe flare-ups (proliferative nephritis, lupus pneumonitis, severe thrombocytopenia, haemolytic anaemia with high rate of haemolysis, severe pericardial effusion, refractory pleural effusion, severe neuropsychiatric manifestations), administration of corticosteroid-sparing immunosuppressants (azathioprine, cyclosporine, tacrolimus) is suggested from the outset. (LE 4, GR √) | 9.92 (.25) | 10 | 100 |
| • In patients with severe flare-ups (proliferative nephritis, lupus pneumonitis, severe thrombocytopenia, haemolytic anaemia with high rate of haemolysis, severe pericardial effusion, refractory pleural effusion, severe neuropsychiatric manifestations), the use of CFM is discouraged in principle, and is only suggested in cases of severe refractory organic activity or risk to maternal life, starting in the 2nd trimester. (LE 2+, GR C) | 9.92 (.25) | 10 | 100 |
| • In patients with severe flare-ups (proliferative nephritis, lupus pneumonitis, severe thrombocytopenia, haemolytic anaemia with high haemolysis rate, severe pericardial effusion, refractory pleural effusion, severe neuropsychiatric manifestations), exceptionally, the use of rituximab in the 1st trimester may be considered. It is not recommended in the more advanced stages due to the risk of B-cell depletion in the infant. (LE 3, GR D) | 9.85 (.34) | 10 | 100 |
| D. Are the lupus activity scales applicable/useful during pregnancy? | |||
| • The use of activity scales is not recommended in clinical practice. (LE 4, GR D) | 9.85 (.34) | 10 | 100 |
| 3. Lupus nephritis (LN) | |||
| A. How is LN diagnosed during pregnancy? | |||
| • It is suggested that the same criteria be used as for non-pregnant patients: (LE 4, GR D)– Proteinuria >.5g/day, protein/creatinine ratio >.5 or worsening of basal proteinuria (increase of 2g/day if basal proteinuria <3g/day or double of basal proteinuria, if previously in nephrotic range) and/or– Unexplained impairment of kidney function (increase of basal Cr >30%) and/or– Active sediment (microhaematuria, pyuria, cylindruria). | 10 (.00) | 10 | 100 |
| • It is suggested to avoid the use of active sediment as a sole marker of kidney activity, as there is an increase in urine infections during pregnancy. (LE 4, GR D) | 9.92 (.25) | 10 | 100 |
| • A kidney biopsy is suggested for the definitive diagnosis of LN. (LE 3, GR D) | 9.42 (.97) | 10 | 100 |
| B. Can a kidney biopsy be performed during pregnancy? When would it be indicated? | |||
| • It is suggested that a kidney biopsy be performed before gestation week (GW) 32, in patients where there is no contraindication, when clinical suspicion is insufficient or there has not been adequate response to treatment. (LE 3, GR D) | 9.50 (.98) | 10 | 100 |
| C. How is a differential diagnosis of LN with pre-eclampsia (PE) made? | |||
| • A kidney biopsy is suggested for definitive diagnosis. (LE 3, GR D) | 9.42 (.97) | 10 | 100 |
| • We suggest complement factor level, anti-dsDNA and urinary sediment testing, and clinical assessment to support a suspicion of LN. (LE 3, GR D) | 10 (.00) | 10 | 100 |
| • Although a recommendation cannot be made at present, angiogenesis markers such as the soluble fms-like tyrosine kinase 1/Placental growth factor (sFlt-1/PlGF) ratio and/or endoglin and Doppler measurement of mean pulsatility in the uterine arteries (mUtA-PI) could be useful for early diagnosis of PE in patients with SLE and APS. (LE 2++) | 9.64 (.71) | 10 | 100 |
| D. What is the treatment for LN during pregnancy? | |||
| • In the initial management of flare-ups of LN, the use of methylprednisolone pulses (250–500mg/day for 3 consecutive days) followed by doses of prednisone or equivalent ≤30mg/day is suggested. (LE 2++, GR C) | 9.85 (.51) | 10 | 100 |
| • A tapering steroid regimen will used be as recommended in the management of severe flare-ups (see the section on activity management). | 9.85 (.51) | 10 | 100 |
| • It is suggested to add from the outset treatments that are pregnancy compatible such as HCQ, azathioprine, calcineurin inhibitors and IVIG, alone or in combination according to the severity of symptoms. (LE 3, GR C) | 9.92 (.25) | 10 | 100 |
| • The use of AZA is suggested as the immunosuppressant of choice for induction therapy in LN that debuts during pregnancy or for maintenance in previously diagnosed patients. (LE 3, GR C) | 9.85 (.51) | 10 | 100 |
| • The use of CFM is not recommended. It should only be considered for use in cases of severe refractory disease activity or risk to maternal life, from the 2nd trimester. (LE 2, GR D) | 9.92 (.25) | 10 | 100 |
| • The use of plasmapheresis or immunoadsorption is suggested in cases refractory to all previous therapies. (LE 3, GR C) | 9.28 (1.16) | 10 | 92.85 |
| • Angiotensin-converting enzyme inhibitors (ACEi) or angiotensin II receptor antagonist (ARA-II) are contraindicated during pregnancy, and therefore the use of nifedipine, labetalol, hydralazine or methyldopa is suggested for HT control. (LE 3, GR C) | 10 (.00) | 10 | 100 |
| 4. Management of complications in pregnant women with APS/APA | |||
| A. How to treat obstetric APS during pregnancy? | |||
| • In patients with obstetric APS and a history of repeated early miscarriage (<10 weeks) treatment with ASA at low doses is recommended (LE1, GRA) with or without combined prophylactic low molecular weight heparin (LMWH). (LE 4, GR D) | 9.14 (2.38) | 10 | 92.85 |
| • In patients with obstetric APS and a history of foetal death (>10 weeks) treatment with ASA at low doses and prophylactic doses of LMWH are recommended. (LE 4, GR D) | 9.85 (.36) | 10 | 100 |
| • In patients with obstetric APS and a history of severe PE and/or placental insufficiency, treatment with ASA at low doses is recommended (LE 1−, GRB) ±LMWH according to the individual risk profile. (LE 4, GR D) | 8.92 (1.43) | 9 | 92.85 |
| • It is suggested that treatment with ASA should be started preconception. (LE 2++, GR C) | 10 (.00) | 10 | 100 |
| • Treatment with ASA is suggested for asymptomatic APA carriers with a high-risk profile. (LE 4, GR D) | 9.78 (.55) | 10 | 100 |
| B. How should refractory obstetric APS be treated? | |||
| • In patients who have had repeated miscarriages and/or foetal losses refractory to treatment with ASA+LMWH it is recommended that HCQ treatment be added for the entire pregnancy or low dose prednisone during the first trimester. (LE 2+, GR C) | 9.78 (.41) | 10 | 100 |
| • In cases of IUGR and/or severe early pre-eclampsia, the use of pravastatin 20mg/day from the onset of the pre-eclampsia is suggested. (LE 2+, GR C) | 8.92 (2.31) | 10 | 92.85 |
| • The use of IVIG and plasmapheresis is not recommended, although it could be considered if there is no response to other treatments. (LE 2, GR√) | 9.35 (.97) | 10 | 100 |
| C. How to manage thrombocytopenia in pregnant women with APS/APA? | |||
| • It is recommended that pregnant patients with APS and thrombocytopenia should be treated in a similar way to thrombocytopenia due to SLE. (LE 3, GR D) | 9.71 (.79) | 10 | 100 |
| D. How should thrombosis be managed in pregnant women with APS/APA? | |||
| • Anticoagulation with LMWH rather than NFH is recommended. (LE 1++, GR A) | 9.85 (.51) | 10 | 100 |
| • NFH, fondaparinux, danaparoid, vena cava filters and thrombolysis are recommended in special situations or if LMWH is contraindicated. (LE 2++, GR B) | 9.92 (.25) | 10 | 100 |
| • The new oral anticoagulants are not recommended as there are no studies of their use in pregnancy. (LE 3, GR C) | 10 (.00) | 10 | 100 |
| • It is suggested that anticoagulation should be maintained throughout pregnancy and up to 6 weeks postpartum in APA −, or indefinitely if APA+. (LE 4, GR D) | 9.92 (.25) | 10 | 100 |
| E. Should LMWH be administered at therapeutic doses every 12 or 24h? | |||
| • There is insufficient evidence to recommend either dosage regimen. (LE 2+, GR C) | 9.92 (.25) | 10 | 100 |
| • It is suggested that LMWH should be used every 24h due to its convenient dosage form (LE 4, GR √) | 9.57 (1.11) | 10 | 92.85 |
| F. Should blood testing take place after starting LMWH in pregnant women with APS/APA? | |||
| • There is not enough evidence to recommend blood tests in pregnant women starting treatment with LMWH. (LE 2++, GR B) | 9.28 (1.82) | 10 | 92.85 |
| G. How should make the transition to LMWH in pregnant women with APS and prior treatment with oral anti-vitamin K anticoagulants? | |||
| • It is suggested that oral anti-vitamin K anticoagulants be replaced with LMWH when the pregnancy test is positive, and frequent testing is recommended to avoid detecting pregnancy beyond the 6th–8th week from the date of the last period. (LE 2+ GR C) | 9.35 (2.31) | 10 | 92.85 |
| H. Should factor Xa monitoring be used in pregnant women with APS and/or APA+ in treatment with LMWH? | |||
| • Factor Xa activity monitoring is not recommended. (LE 2, GR B) | 9.21 (2.30) | 10 | 92.85 |
| 5. Anti-Ro/anti-La antibodies and congenital heart block (CHB) | |||
| A. Should we treat all anti-Ro+ pregnant women with HCQ? | |||
| • During pregnancy, it is suggested that women with anti-Ro/anti-La positive antibodies are treated with HCQ, since this can reduce the risk of CHB. (LE 2+, GR C) | 10 (.00) | 10 | 100 |
| B. At what point would it be recommended to start treatment with HCQ? | |||
| • It is suggested that treatment with HCQ be started prior to pregnancy, when the patient is attempting to become pregnant. (LE 4, GR √) | 9.42 (1.44) | 10 | 92.85 |
| C. How should cardiac involvement be monitored in anti-Ro+ pregnant women? | |||
| • In pregnant women with anti-Ro and/or anti-La positive antibodies, CHB screen is suggested by means of Doppler echocardiography, every 2 weeks from gestation week 16–18 to 30–34. (LE 4, GR D) | 9.64 (.71) | 10 | 100 |
| • In pregnant women with anti-Ro and/or anti-La positive antibodies and a history of CHB or neonatal lupus, CHB screening is recommended weekly until gestation week 16 to 26, and every 2 weeks thereafter until week 34. (LE 4, GR D) | 9.78 (.55) | 10 | 100 |
| D. What would be the treatment guidelines in anti-Ro+ with grade I,II,III foetal heart bloc or foetal fibroelastosis/hydrops fetalis? | |||
| • In the first test for first-degree HB, treatment is not recommended. In the case of persistent first-degree HB, fluorinated GCs are recommended which should be tailored to the patient, and the prolonged use of high doses is not recommended. (LE 3, GR √) | 9.07 (2.31) | 10 | 92.85 |
| • The use of fluorinated GCs is suggested in cases of 2nd degree or 3rd degree heart block associated with hydrops fetalis. (LE 2+, GR C) | 9.78 (.55) | 10 | 100 |
| • In particularly severe cases, combination therapy with GC, IVIG and/or plasmapheresis is suggested. (LE 3, GR D) | 9.35 (1.34) | 10 | 92.85 |
| • Treatment with IVIG is not recommended, as its efficacy has not been demonstrated. (LE 2+, GR C) | 9.78 (.55) | 10 | 100 |
| • It is suggested not to maintain treatment with high doses of GC from diagnosis of CHB until the end of the pregnancy. (LE 4, GR √) | 9.85 (.34) | 10 | 100 |
| • There are no data to recommend the use of dexamethasone over betamethasone. They can be used interchangeably. (LE 2+, GR C) | 10 (.00) | 10 | 100 |
| 6. Placental defects, gestational vascular complications | |||
| A. Who should be screened for pre-eclampsia risk (PE) and when? | |||
| • PE screening is recommended for all pregnant women at the beginning of pregnancy, investigating both pre-pregnancy and gestational risk factors. (LE 1++, GR A) | 10 (.00) | 10 | 100 |
| • A combination of different risk factors, such as maternal characteristics, obstetric history and biochemical and biophysical markers, including uteroplacental Doppler, is recommended for the calculation of specific risk for pre-eclampsia. (LE 1++, GR A) | 10 (.00) | 10 | 100 |
| • It is suggested that positivity for antiphospholipid antibodies (with or without lupus) and the presence or previous history of lupus nephritis should be considered as sufficient factors for initiating PE prophylaxis, therefore screening may not be necessary in these women. (LE 2+, GR C) | 9.85 (.51) | 10 | 100 |
| • It is suggested considering only pregnant women who repeatedly test positive for antiphospholipid antibodies as a PE risk group, particularly those who are carriers of lupus anticoagulant and/or who are double or triple positive. (LE 2+, GR C) | 9.85 (.51) | 10 | 100 |
| • It is suggested not to consider inactive SLE with no history of nephritis as a risk factor when calculating PE risk. (LE 2++, GR B) | 9.50 (.90) | 10 | 100 |
| B. Should we treat patients with previous PE or PE risk factors with ASA? | |||
| • The administration of ASA at low doses is recommended for PE risk prevention in pregnant women considered to be at high risk. (LE 1++, GR A) | 10 (.00) | 10 | 100 |
| • It is recommended to start prophylaxis with ASA before 16 weeks of gestation. (LE 1+, GR A) | 10 (.00) | 10 | 100 |
| • Doses of ASA of between 75 and 150mg/day are recommended. (LE 1+, GR A) | 10 (.00) | 10 | 100 |
| • It is recommended to administer ASA to high-risk pregnant women from 16 weeks if it has not been possible to start it earlier. (LE 1+, GR A) | 10 (.00) | 10 | 100 |
| • It is suggested to start treatment with ASA before week 12 in patients with sustained positivity for antiphospholipid antibodies (with or without lupus) and/or presence or previous history of lupus nephritis, without waiting for the screening results. (LE 4, GR √) | 10 (.00) | 10 | 100 |
| C. How useful is uterine artery (UtA) Doppler ultrasound in these patients? | |||
| • UtA Doppler ultrasound is suggested in the 1st and 2nd trimester, as part of these patients’ obstetric follow-up. Doppler ultrasound in the 1st trimester can be of particular interest in pregnant women with SLE estimated to be at low risk for PE, which, if abnormal, could justify starting ASA prophylaxis. (LE 3, GR D) | 9.92 (.25) | 10 | 100 |
| • In pregnancies with a pathological UtA Doppler in the second trimester, screening for IUGR screening is suggested (serial biometry and UtA Doppler) from week 26–28. (LE 2+, GR C) | 10 (.00) | 10 | 100 |
| D. How useful is Doppler ultrasound of foetal circulation in these patients? | |||
| • Umbilical artery Doppler ultrasound is recommended as a primary method of monitoring the small-for-gestational-age foetus (SGA) and IUGR. (LE 1+, GR A) | 9.92 (.25) | 10 | 100 |
| • The routine use of umbilical artery Doppler ultrasound is suggested for women with antiphospholipid antibodies and SLE with risk factors, obstetric or medical, for gestational vascular complications especially IUGR. (LE 3, GR D) | 9.92 (.25) | 10 | 100 |
This research study has received no specific support from public sector agencies, the commercial sector or non-profit organisations.
Conflict of interestsE. Rodríguez Almaraz has received funding for presentations, courses and conferences from Novartis, Roche, GSK, Menarini, Grünenthal, Abbvie, UCB and Lilly, and research grants from MSD.
V. Martínez-Taboada has received financial support from Roche for an independent research project and from Sanofi for presentations.
The remaining authors have no conflict of interests to declare.
Please cite this article as: Rodríguez Almaraz E, Sáez-Comet L, Casellas M, Delgado P, Ugarte A, Vela-Casasempere P, et al. Control del embarazo en pacientes con lupus eritematoso sistémico/síndrome antifosfolípido. Parte 2: seguimiento del embarazo. Reumatol Clin. 2021;17:125–131.
Consensus document of the Spanish Society of Gynaecology and Obstetrics (SEGO), the Systemic Autoimmune Diseases Group (GEAS) of the Spanish Society of Internal Medicine (SEMI) and the Spanish Society of Rheumatology (SER).