Entheses are regions of fibrocartilage located predominantly in extra-articular areas and constitute a major target in psoriatic arthritis (PsA), with a prevalence rate of 35%,1 as well as in spondyloarthritis (SpA), notably in HLA-B27 (human leukocyte antigen - B27)-negative patients.2 They have a specific immune microenvironment triggered by mechanical stress, genetic susceptibility, and microorganisms3 and their main function as a component of the enthesis-organ complex is to diffuse the concentration of mechanical stress on the bone surface away from the attachment.4 Although enthesophytes are typically seen on plain X-rays in an asymptomatic elderly population, the occipital enthesophyte (OE) is present in 41% of all adults under the age of 30 years.5
To the best of our knowledge, OE has not been documented in inflammatory rheumatic diseases; therefore, our aim was to determine its prevalence in PsA, SpA, and rheumatoid arthritis (RA) and to compare it with patients with mechanical neck pain (MNP). We designed a retrospective descriptive study of the plain cervical X-rays in lateral projection of individuals over 18 years of age who attended the rheumatology department of a university hospital between July 2022 and January 2023; a total of 30 patients per group (120 in total) were studied. The reason for requesting the radiograph was neck pain in the MNP group (excluding traffic accidents and neck surgery) and RA, and as part of the diagnostic protocol in the PsA and SpA groups. The following variables were obtained: sex, age at the time the X-ray was performed, OE (yes/no) assessed by a rheumatologist with 25 years of experience and by a fourth-year rheumatology resident. The results are presented descriptively; Cohen’s Kappa coefficient was calculated to quantify the degree of agreement between the two rheumatologists; sex and prevalence were compared using the χ2 test, applying the Yates correction, and ANOVA was used for mean age.
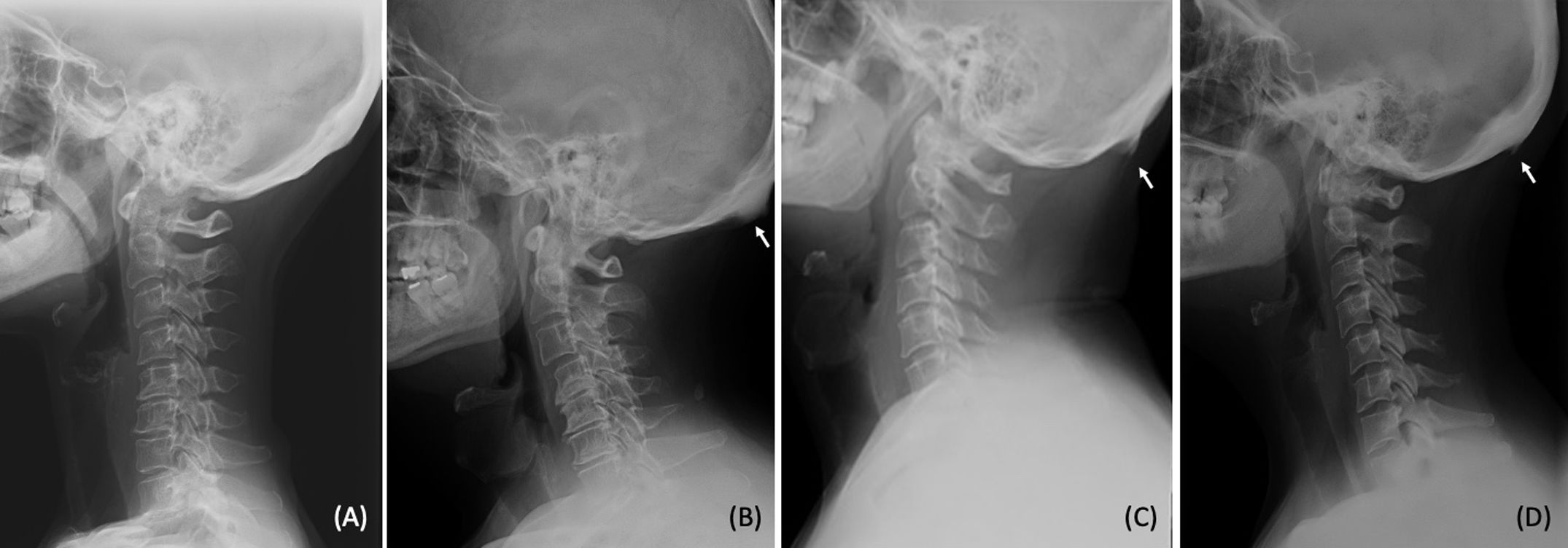
Seventy-eight per cent (78%) were female and the mean age of the sample was 58.5 ± 15 years. The four groups were homogeneous in terms of sex and age, and stratified analysis failed to reveal any difference (p = 0.2 and p = 0.06, respectively), only a tendency toward greater presence in the elderly in the MNP group. Fifty-one per cent (51%) had OE, 23% in the MNP group and 60% in inflammatory diseases (70% SpA, 70% AP, and 40% RA), with OE being statistically significant in inflammatory rheumatic diseases (p < 0.001). Substantial agreement was reached overall (89%) and almost perfect agreement in SpA and PsA (97%). To describe them macroscopically, different OE morphologies were seen to be thicker in the SpA and PsA groups and thinner in the RA group (Fig. 1).
In psoriatic patients the burden of bone erosions is not significantly greater than in healthy controls, whereas the differences in enthesophytes are far more pronounced.6 The prevalence of asymptomatic enthesopathy with Doppler signal on ultrasound was significantly higher in psoriatic patients (77%) than in controls7 and has been proven to be specific to peripheral enthesitis in SpA.8 Given that this was an exploratory study, there are several limitations: we did not correlate this enthesopathy with pain, type of psoriasis, HLA-B27 genetic predisposition, physical activity, or BMI. consequently, we will assess this in future studies using other imaging tests to determine whether it might be helpful in the early diagnosis of psoriasis patients without PsA7 or with nascent PsA and negative SpA-B27, and whether it might be a predictive factor for developing a more severe form of the disease.
FundingThis research has not received any specific support from public sector agencies, the commercial sector, or non-profit organisations.
The authors would like to acknowledge Dr Jesús Sanz for having noted this enthesophyte and proposing for having noticed this enthesophyte and proposing that it be designated, as a secondary term, Sanz's sign.