Osteitis fibrosa cystica is a bone disease caused by advanced or severe hyperparathyroidism, with a prevalence of about 5% in developed countries. It is not easy to diagnose, since the clinical and radiological features can lead to its being confused with a series of other disorders, such as giant-cell tumors of the bone or even as bone metastases.1 On the other hand, tendon rupture is a complication associated with chronic kidney disease in patients with secondary or tertiary hyperparathyroidism, but its development in primary hyperparathyroidism has scarcely been reported.2
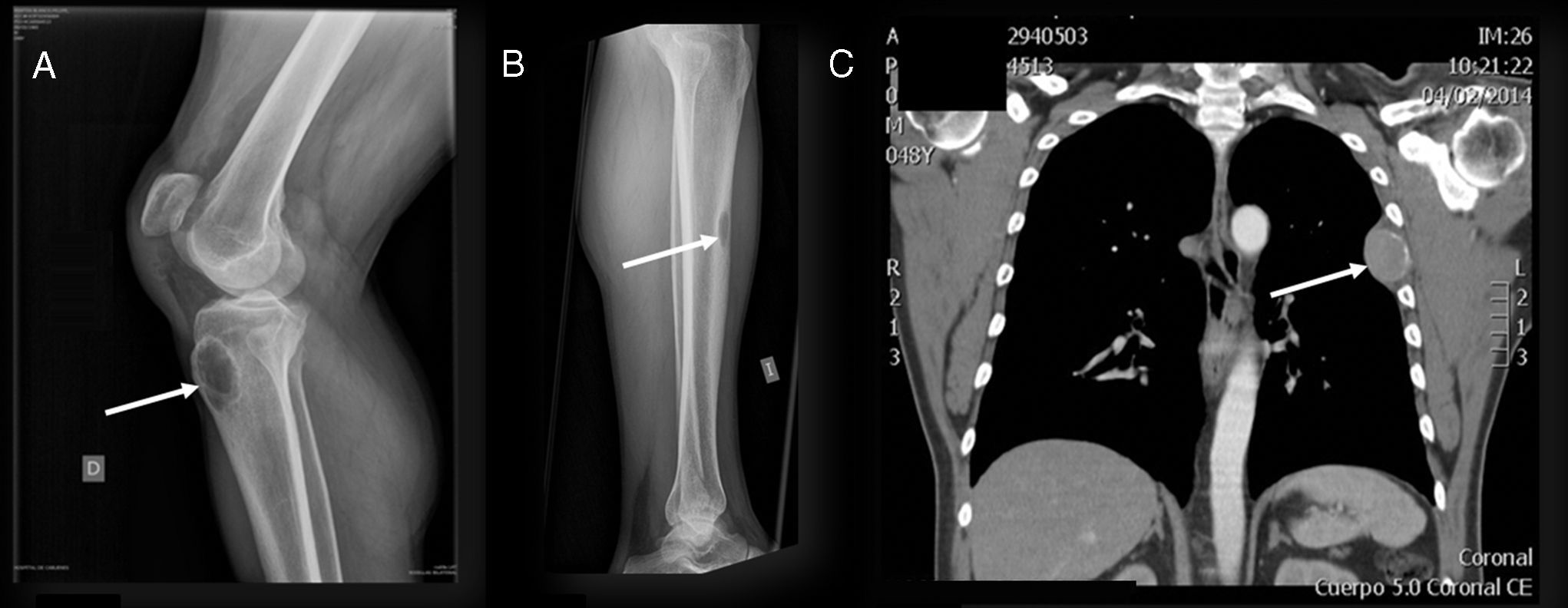
We present the case of a 48-year-old man who had no significant familial or personal history, and was being treated with nonsteroidal anti-inflammatory drugs (NSAID) to relieve widespread pain that had begun months earlier. He was admitted by the orthopedic department due to pain and to the sudden onset of functional incapacity in both knees. The diagnosis was rupture of the patellar tendons, and he was scheduled for surgical reinsertion. A radiograph of lower limbs showed nonossifying fibromas in right anterior tibial tuberosity and in the middle third of left tibia (Fig. 1). In the preoperative study, he underwent a chest radiograph, which revealed a nodular structure in left hemithorax. The study was completed with chest computed tomography, which disclosed the presence of a lytic lesion growing toward the pleura. The lesion, in the left 5th rib, had a diameter of 5cm, and suggested a possible bone metastasis (Fig. 1), although no other changes were observed.
At the same time, an analytical study was performed with the following results: urea 72mg/dL (normal 10–50), creatinine 2.45mg/dL (0.55–1.3), calcium 15.4mg/dL (8.1–10.4) and phosphorus 2.8mg/dL (2–5). Given the existence of hypercalcemia and deterioration of kidney function, additional analyses were requested: parathyroid hormone (PTH) 1027pg/mL (14–72), 25 (OH) vitamin D 12.1ng/mL (30–70), alkaline phosphatase 335I/U (40–117) and urinary calcium 350mg/dL/24h, findings compatible with severe hypercalcemia secondary to primary hyperparathyroidism with probable bone and renal involvement. Thus, localization studies were requested. Neck ultrasound showed a nodular structure beneath the left lower border of the thyroid. It measured 15mm, and was compatible with left inferior parathyroid adenoma, and 99mTc-sestamibi parathyroid scintigraphy showed an increase in uptake in the same region. Abdominal ultrasound revealed the existence of lithiasis in left renal sinus, with no further evidence of disease.
The patient underwent surgery in both knees, with suturing and osteosynthesis involving the patellar tendon, and a specimen was taken of the fibroma in right anterior tibial tuberosity. The pathological report described a giant cell tumor suggestive of a brown tumor associated with hyperparathyroidism, but it was not possible to rule out a giant cell reparative granuloma. After controlling hypercalcemia with intravenous bisphosphonates, neck surgery was performed and a left inferior parathyroid adenoma was resected. As a result, a normal serum calcium level was achieved and there was a partial improvement in renal function. After a year and a half of follow-up, the bone lesions in tibiae and rib have become smaller, although they have not disappeared.
The classical bone manifestation in severe hyperparathyroidism is osteitis fibrosa cystica, highly uncommon at the present time. It develops due to excessive action of PTH on bone, which activates the osteoclasts, and osteocytes are replaced by fibrous tissue, giving rise to microfractures and microhemorrhages. It is characterized by diffuse pain, skeletal deformities and pathological fractures that can be reversible after parathyroidectomy.3 The rupture of both patellar tendons is usually associated with secondary or tertiary hyperparathyroidism with advanced renal failure in patients on hemodialysis. The coexistence of these lesions in primary hyperparathyroidism is unusual.4
Please cite this article as: Riestra Fernández M, Suárez Gutiérrez L, Martínez M, Diéguez Felechosa M. Hiperparatiroidismo primario: una forma infrecuente de presentación. Reumatol Clin. 2017;13:246–247.