We present a case series of 5 patients with psychosis associated with SLE according to the ACR 1999 criteria. It presented as an initial clinical manifestation, clinically they had visual and auditory hallucinations, all the patients were women, average age 25 years, the accompanying manifestations were mostly mucocutaneous, articular and renal. Two patients presented antiphospholipid syndromes. The remission induction treatment was based on pulses of steroids and cyclophosphamide with a complete response in 4/5 patients, maintenance was left with mycophenolic acid and azathioprine.
Presentamos una serie de casos de 5 pacientes con psicosis asociados a LES según los criterios ACR 1999. Se presentó como manifestación clínica inicial, clínicamente tenían alucinaciones visuales y auditivas, todas las pacientes fueron mujeres, edad promedio 25 años, las manifestaciones acompañantes fueron en su mayoría mucocutáneo, articular y renal. Dos pacientes presentaban síndromes antifosfolípidos. El tratamiento de inducción a la remisión se baso en pulsos de esteroides y ciclofosfamida con respuesta completa 4/5 pacientes, el mantenimiento se dejó con ácido micofenólico y azatioprina.
Systemic lupus erythematosus (SLE) is an autoimmune disorder which may affect any organ systemically, with a broad clinical presentation. Manifestations may be neuropsychiatric which may occur before or around the diagnosis of SLE, in 25%-75% of cases.1 Psychiatric manifestations are rare, among which is psychosis that is characterised by delusions and hallucinations. It is a complex presentation of neuropsychiatric SLE (NPSLE).2 It has been associated with a lupus-specific autoantibody against ribosomal P, although inconsistently and due to its rarity, the number of clinical studies has been limited and most consist of case series.3 Our main objective is to describe the clinical aspects and management of five patients with NPSLER in a tertiary level hospital.
Patients and methodsFive patients presented and were retrospectively identified through revision of their medical records, from a referral centre in the North East of Mexico, located in Monterrey, Nuevo León. They had been diagnosed with SLE and had presented with psychosis, in accordance with the ACR 19994 criteria. They had been assessed by the psychiatric department for a period of 20 years.
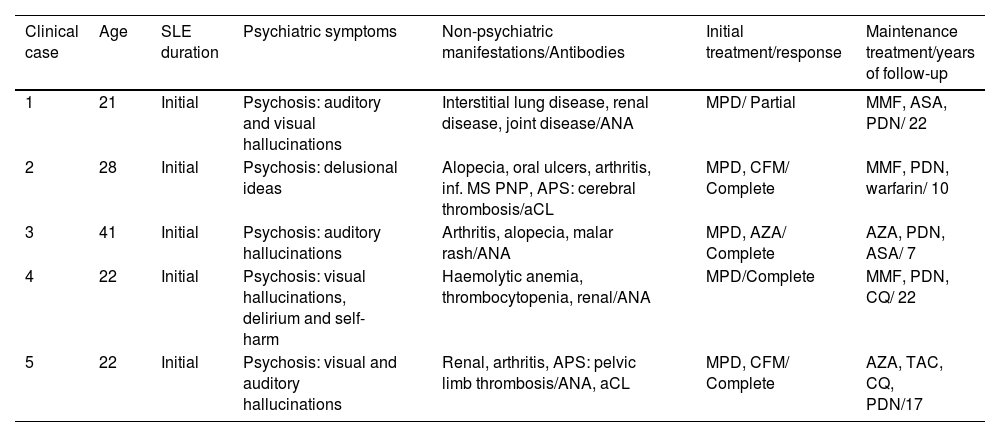
ResultsTable 1 contains the demographic and clinical characteristics of the five patients.
Clinical and demographic characteristics of 5 women with psychiatric lupus.
| Clinical case | Age | SLE duration | Psychiatric symptoms | Non-psychiatric manifestations/Antibodies | Initial treatment/response | Maintenance treatment/years of follow-up |
|---|---|---|---|---|---|---|
| 1 | 21 | Initial | Psychosis: auditory and visual hallucinations | Interstitial lung disease, renal disease, joint disease/ANA | MPD/ Partial | MMF, ASA, PDN/ 22 |
| 2 | 28 | Initial | Psychosis: delusional ideas | Alopecia, oral ulcers, arthritis, inf. MS PNP, APS: cerebral thrombosis/aCL | MPD, CFM/ Complete | MMF, PDN, warfarin/ 10 |
| 3 | 41 | Initial | Psychosis: auditory hallucinations | Arthritis, alopecia, malar rash/ANA | MPD, AZA/ Complete | AZA, PDN, ASA/ 7 |
| 4 | 22 | Initial | Psychosis: visual hallucinations, delirium and self-harm | Haemolytic anemia, thrombocytopenia, renal/ANA | MPD/Complete | MMF, PDN, CQ/ 22 |
| 5 | 22 | Initial | Psychosis: visual and auditory hallucinations | Renal, arthritis, APS: pelvic limb thrombosis/ANA, aCL | MPD, CFM/ Complete | AZA, TAC, CQ, PDN/17 |
aCL: anticardiolipin antibody; ANA: antinuclear antibodies; APS: antiphospholipid syndrome: ASA: acetylsalicylic acid; AZA: azathioprine; CFM: cyclophosphamide; CQ: chloroquine; MMF: mycophenolate acid: MPD: methylprednisolone: PDN: prednisone: PNP: polyneuropathy; SLE: systemic lupus erythematosus; TAC: tacrolimus.
The sample comprised five patients with a diagnosis of SLE with neuropsychiatric involvement (psychosis) as part of the initial manifestation. All patients were female, with an average age of 25 (21-42) years. Among the non-psychiatric manifestations, they presented with arthritis, alopecia, ulcers, malar erythema, renal involvement, haematological involvement. Two patients presented with antiphospholipid syndrome. Among the immunological manifestations we found positive antinuclear antibodies (ANA) and antiphospholipid (APL) antibodies.
Methylprednisolone and cyclophosphamide were used as induction treatment, with four patients having a complete response after three months. Maintenance treatment was with oral steroids, mycophenolic acid, azathioprine and chloroquine. 80% of the patients have remained relapse-free in the long term (Table 1).
DiscussionThe prevalence of lupus psychosis (LP) varies from 2%-11%,1 using the ACR definition. However, in a study presented by Hanly et al., prevalence was 1.5%.4,5 According to the diagnostic protocol, other causes such as infections and adverse effects of medications6 must be ruled out. LP frequently occurs in association with additional neuropsychiatric manifestations such as seizures and/or depression. However, LP may appear as an onset sign/symptom or in the first year after diagnosis of SLE.7 Both the activity of SLE and the presence of other previous neuropsychiatric manifestations are risk factors for developing LP. Recovery from LP is usually complete within a year with adequate SLE treatment. There are usually no relapses if there is good control of the underlying autoimmune disease, even without antipsychotics as we reported in our case series.7,8
The symptoms of psychosis mostly presented paranoid delusions, and auditory and visual hallucinations. They therefore did not differ from a conventional psychosis condition and diagnosis continued to be one of exclusion; infectious processes at the central nervous system level were ruled out in all our patients as part of the diagnostic approach.6,9
The anti-P ribosomal antibody is 90% associated with the presence of psychosis or periods of activity, but one limitation of our centre was that we were unable to determine the anti-P ribosomal antibody in these patients to obtain conclusions in this regard.10
Our report was from a single centre with a small series of cases. This is to be expected since LP is a rare complication. For this reason, we consider that the analysis of these patients helped us to identify the clinical manifestations of this presentation of SLE and in doing so provide a timely and adequate treatment leading to a favourable impact on the long-term control of the patients. It is important to highlight that our patients remained free of neuropsychiatric symptoms in the long-term follow-up of 20 years.
The authors have no conflict of interests to declare.