Pulmonary-renal syndrome has rarely been reported as the clinical presentation of vasculitis caused by the consumption of cocaine adulterated with levamisole. We report the case of a patient in whom we detected the clinical manifestations and indicate the difficulties that arose in relation to the diagnostic and therapeutic approach.
El síndrome pulmón-riñón rara vez ha sido reportado como cuadro clínico de presentación de vasculitis causada por el consumo de cocaína contaminada con levamisol. Se reporta el caso de un paciente con este cuadro clínico y se señalan las dificultades que se presentaron durante el abordaje diagnóstico y terapéutico.
Cocaine consumption is still a public health problem. The adulteration of cocaine with substances such as levamisole leads to the appearance of additional medical problems. Vasculitis caused by levamisole is highly heterogeneous in terms of clinical symptoms and analytical results, hindering diagnosis.
Clinical observationA 34 year-old male with a history of reactive arthritis and daily marihuana consumption. He denied consuming cocaine. He was admitted for one week due to general discomfort, pallor, a dry cough, thoracic pain and dyspnea. Mucocutaneous pallor, hypoxemia and rale in the base of the lungs. He was normotensive, with no tachycardia or fever.
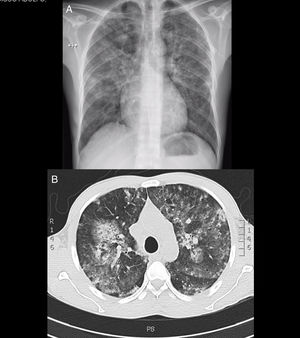
He had severe anaemia, renal dysfunction and mixed opacities in both pulmonary fields (Fig. 1 and Table 1). He was diagnosed pulmonary-renal syndrome and treatment commenced with high doses of steroids and blood cell transfusion. At first the diagnosis of systemic lupus erythmatosus (SLE) was considered due to the finding of hypocomplementemia. Additional studies found multiple antibody positivity: ANCA (antimyeloperoxidase and antiproteinase-3), ANA, anti-Ro, anti-La, lupus anticoagulant, rheumatoid factor and anticardiolipin IgM. Anti-Sm, anti-DNA and anti-basement glomerular membrane antibodies were negative.
Analytical results.
| Analysis | Result |
|---|---|
| Creatinine (0.60-1.10mg/dl) | 2.16 |
| Urine analysis (cells per high power field (HPF) | Proteins 75mg/leukocytes 0-5/CAP/erythrocytes 21-50/HPF (70% crenated) |
| Proteins in urine 24hrs (10-150mg) | 1,410 |
| C Reactive protein (0.01-0.82mg/dl) | 4.13 |
| Haemoglobin (13.0-17.0g/dl) | 3.1 |
| Haematocrit (42.0-52.0%) | 10.1 |
| White cells (4,500-11,000/mm3) | 8,100 |
| Neutrophils (1,500-6,100/mm3) | 2,800 |
| Lymphocytes (1,500-3,500/mm3) | 4,800 |
| Eosinophils (0-700/mm3) | 100 |
| Monocytes (0-1,000/mm3) | 400 |
| Basophils (0-200/mm3) | 0 |
| Platelets (150-450×103/mm3) | 315,000 |
| Ferritine (15-200ng/ml) | 70 |
| Vitamin B12 (124-732pg/ml) | 492 |
| Folic acid (3.5-19.5ng/ml) | 10.3 |
| Complement C3 (82-185mg/dl) | 75 |
| Complement C4 (15-53mg/dl) | 9.9 |
| ANA (dilution, pattern) | 1:640, spotted |
| Anti-Ro (0-20 units) | 118.6 |
| Anti-La (0-20 units) | 87.6 |
| Anti-Sm (0-20 units) | 4.4 |
| Anti-RNP (0-20 units) | 5.3 |
| Native anti-DNA | Negative |
| Anticardiolipins IgM (0-12.5MPL/ml) | 29.5 |
| Anticardiolipins IgG (0-15GPL/ml) | 2.9 |
| Confirmatory lupus anticoagulant | Normalised ratio 1.72 (positive) |
| Anti-ß2 glycoprotein 1 IgG (0-20 units) | .70 |
| Anti-ß2 glycoprotein 1 IgM (0-20 units) | 6.19 |
| ANCA Anti MPO (0-20 units) | 105.5 |
| ANCA Anti PR3 (0-20 units) | 48.7 |
| Anti-glomerular basement membrane IgG (0-20 units) | 3.6 |
| Rheumatoid factor (0-30UI/ml) | 40.6 |
| Prothrombin time (s) | 11.2 |
| Partial thromboplastin time (s) | 31.6 |
Diffuse endocapilar glomerulonephritis was observed in a renal biopsy, with immune complex deposits and tubulointerstitial nephritis. Fibrobroncoscoy confirmed alveolar haemorrhage (haemosiderophages 40%) and ruled out infection. During a subsequent evaluation perforation of the nasal septum was observed and the patient confirmed frequent consumption of cocaine. As well as insisting on the cessation of consumption treatment with prednisolone continued, with good clinical response and a rise in haemoglobin, although there was only partial improvement in renal function, so that additional monthly boli of cyclophosphamide were added.
DiscussionDuring recent years the number of cases of vasculitis associated with levamisole-adulterated cocaine consumption has increased. This disease may compromise multiple organs and systems.1,2
Alveolar haemorrhage is rare. McGrath et al. described a series of 30 cases of levamisole-induced ANCA vasculitis. Three of the cases had alveolar haemorrhage, and it was not possible to prove renal involvement in any of them.3 Cases of pulmonary-renal syndrome are even rarer due to this entity.4
No definitive criteria for diagnosis of this syndrome exist. Diagnosis is based on epidemiological, clinical and analytical findings. In the majority of cases it is not possible to prove contamination by levamisole, as the test is not clinically available and measurement has to take place within 24hrs. of the previous consumption. A high level of suspicion is necessary prior to probing for cocaine consumption. Differential diagnosis is broad. It may be confused with vasculitis associated with ANCA, Goodpasture syndrome and even SLE.
Vasculopathy secondary to levamisole is characterised by high titers of p-ANCA directed against multiple rare antigens, as well as concomitant positivity for c-ANCA,5,6 a rare expression in patients with primary vasculitis. Positivity for multiple antibodies and consumption as a complement may lead to confusion with SLE.
The rate of recurrence in the case of continued cocaine consumption is high. The role of immunosuppressor therapy is unknown, and no treatment patterns have been defined. The patient responded partially to steroids and the suspension of the causal agent. The addition of cyclophosphamide seems to have contributed to his final clinical improvement.
ConclusionsThis case represents a clinical challenge due to its atypical form of presentation, the severity of its manifestations and the difficulty of diagnosis. It is necessary to know the different clinical and analytical manifestations caused by cocaine/levamisole consumption, and to maintain a high level of suspicion regarding the possibility of this consumption, which may be denied by the patient.
Conflict of interestsThe authors have no conflict of interests to declare.
Please cite this article as: Restrepo-Escobar M, Sylva D, Gamboa JG, Echeverri A, Márquez J, Pinto LF. Síndrome pulmón-riñón secundario a vasculitis por cocaína/levamisol: reporte de caso . https://doi.org/10.1016/j.reuma.2018.02.014