We studied a series of 8 patients (5 men and 3 women) who presented with urticaria-like wheals and purpura that had developed more than 24h earlier.
Diagnosis and Disease CourseFour patients were diagnosed with urticarial vasculitis (UV), 2 of them with hypocomplementemia, and another 4 patients with urticaria without vasculitis. None of them had extracutaneous involvement. Their protein profiles and immunoglobulin levels were normal and serological tests for human immunodeficiency virus and hepatitis B and C viruses were negative (other parameters are shown in Table 1).
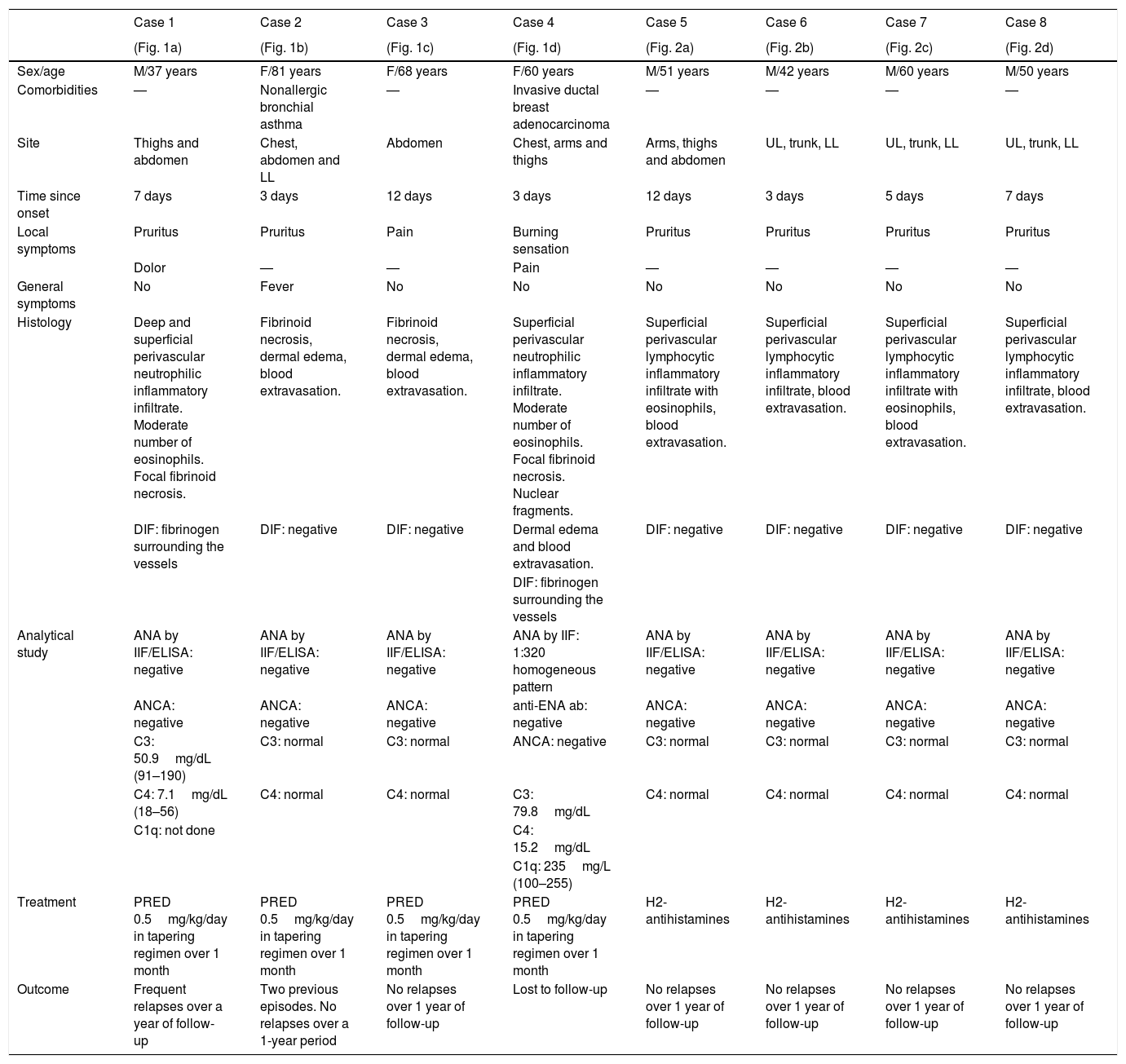
Summary of Clinical and Analytical Data.
| Case 1 | Case 2 | Case 3 | Case 4 | Case 5 | Case 6 | Case 7 | Case 8 | |
|---|---|---|---|---|---|---|---|---|
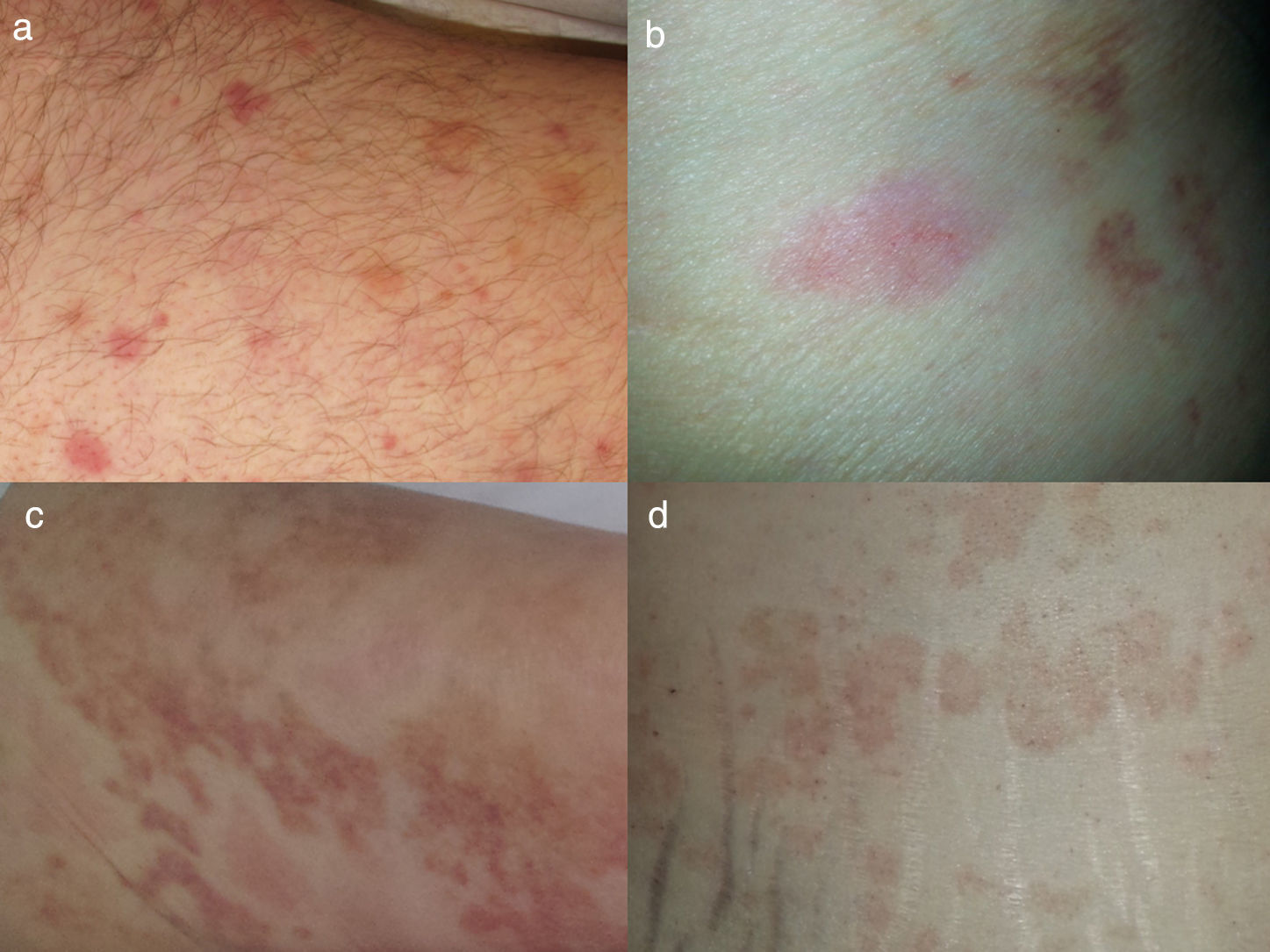
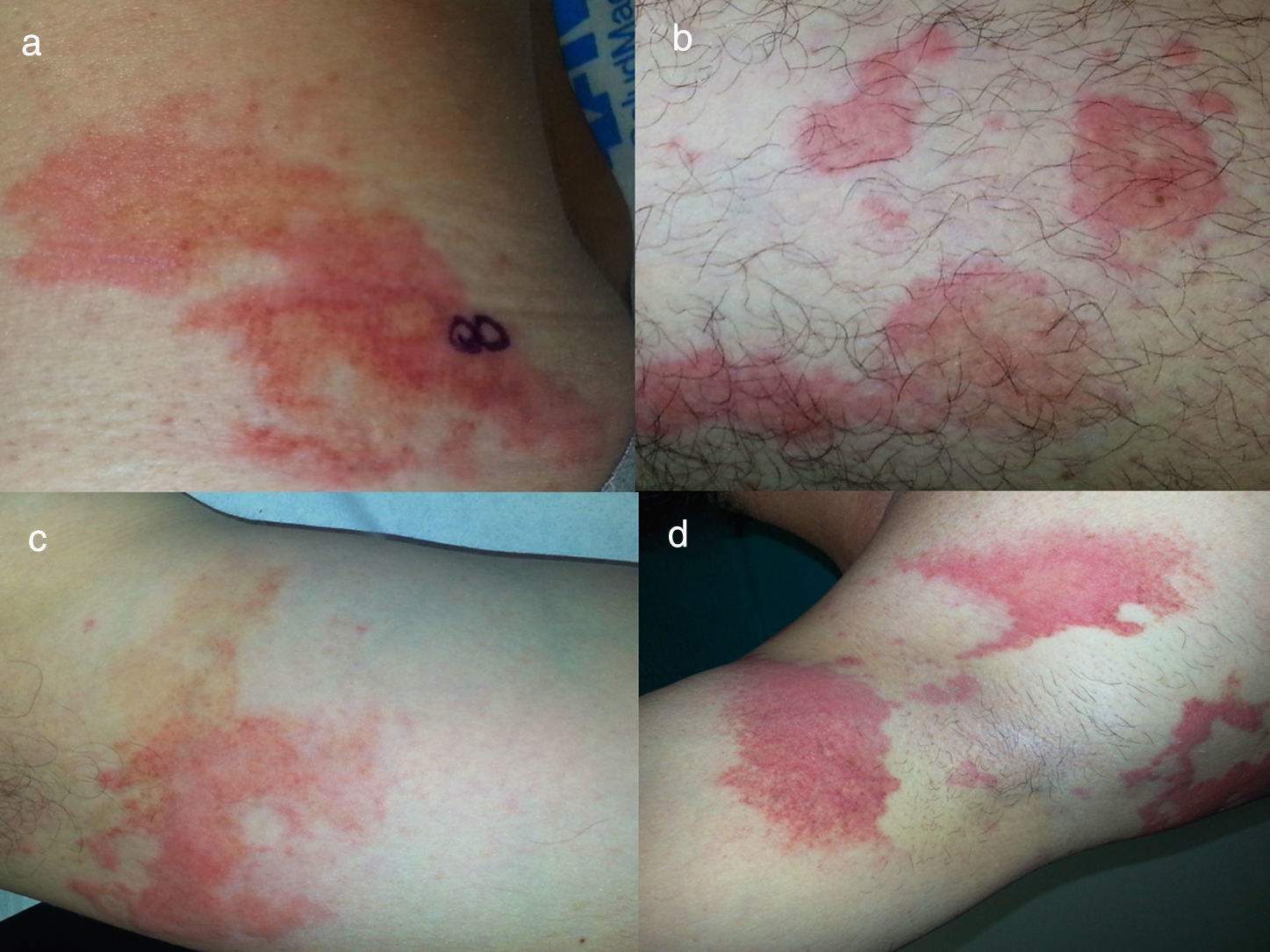
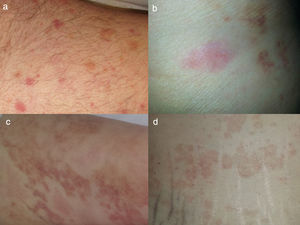
| (Fig. 1a) | (Fig. 1b) | (Fig. 1c) | (Fig. 1d) | (Fig. 2a) | (Fig. 2b) | (Fig. 2c) | (Fig. 2d) | |
| Sex/age | M/37 years | F/81 years | F/68 years | F/60 years | M/51 years | M/42 years | M/60 years | M/50 years |
| Comorbidities | — | Nonallergic bronchial asthma | — | Invasive ductal breast adenocarcinoma | — | — | — | — |
| Site | Thighs and abdomen | Chest, abdomen and LL | Abdomen | Chest, arms and thighs | Arms, thighs and abdomen | UL, trunk, LL | UL, trunk, LL | UL, trunk, LL |
| Time since onset | 7 days | 3 days | 12 days | 3 days | 12 days | 3 days | 5 days | 7 days |
| Local symptoms | Pruritus | Pruritus | Pain | Burning sensation | Pruritus | Pruritus | Pruritus | Pruritus |
| Dolor | — | — | Pain | — | — | — | — | |
| General symptoms | No | Fever | No | No | No | No | No | No |
| Histology | Deep and superficial perivascular neutrophilic inflammatory infiltrate. Moderate number of eosinophils. Focal fibrinoid necrosis. | Fibrinoid necrosis, dermal edema, blood extravasation. | Fibrinoid necrosis, dermal edema, blood extravasation. | Superficial perivascular neutrophilic inflammatory infiltrate. Moderate number of eosinophils. Focal fibrinoid necrosis. Nuclear fragments. | Superficial perivascular lymphocytic inflammatory infiltrate with eosinophils, blood extravasation. | Superficial perivascular lymphocytic inflammatory infiltrate, blood extravasation. | Superficial perivascular lymphocytic inflammatory infiltrate with eosinophils, blood extravasation. | Superficial perivascular lymphocytic inflammatory infiltrate, blood extravasation. |
| DIF: fibrinogen surrounding the vessels | DIF: negative | DIF: negative | Dermal edema and blood extravasation. | DIF: negative | DIF: negative | DIF: negative | DIF: negative | |
| DIF: fibrinogen surrounding the vessels | ||||||||
| Analytical study | ANA by IIF/ELISA: negative | ANA by IIF/ELISA: negative | ANA by IIF/ELISA: negative | ANA by IIF: 1:320 homogeneous pattern | ANA by IIF/ELISA: negative | ANA by IIF/ELISA: negative | ANA by IIF/ELISA: negative | ANA by IIF/ELISA: negative |
| ANCA: negative | ANCA: negative | ANCA: negative | anti-ENA ab: negative | ANCA: negative | ANCA: negative | ANCA: negative | ANCA: negative | |
| C3: 50.9mg/dL (91–190) | C3: normal | C3: normal | ANCA: negative | C3: normal | C3: normal | C3: normal | C3: normal | |
| C4: 7.1mg/dL (18–56) | C4: normal | C4: normal | C3: 79.8mg/dL | C4: normal | C4: normal | C4: normal | C4: normal | |
| C1q: not done | C4: 15.2mg/dL | |||||||
| C1q: 235mg/L (100–255) | ||||||||
| Treatment | PRED 0.5mg/kg/day in tapering regimen over 1 month | PRED 0.5mg/kg/day in tapering regimen over 1 month | PRED 0.5mg/kg/day in tapering regimen over 1 month | PRED 0.5mg/kg/day in tapering regimen over 1 month | H2-antihistamines | H2-antihistamines | H2-antihistamines | H2-antihistamines |
| Outcome | Frequent relapses over a year of follow-up | Two previous episodes. No relapses over a 1-year period | No relapses over 1 year of follow-up | Lost to follow-up | No relapses over 1 year of follow-up | No relapses over 1 year of follow-up | No relapses over 1 year of follow-up | No relapses over 1 year of follow-up |
ab, antibody; ANA, antinuclear antibodies; ANCA, antineutrophil cytoplasmic antibodies; ELISA, enzyme-linked immunosorbent assay; ENA, extractable nuclear antigens; DIF, direct immunofluorescence; F, female; IIF, direct immunofluorescence LL, lower limbs; m, male; PRED, prednisone; UA, upper airway; UL, upper limbs;
Urticarial vasculitis is characterized in clinical terms by urticaria-like wheals and histologically by leukocytoclastic vasculitis (LV). The rash lasts more than 24h and leaves residual purpura.1 In clinical practice, it is not uncommon to see urticaria-like conditions that persist over 24h that are accompanied by a purpuric component. Biopsy only reveals the presence of a superficial perivascular lymphocytic infiltrate. The cause of purpura in the absence of LV is controversial: some authors maintain that the origin is lymphocytic vasculitis2 and others that it is due to scratching.3 Lee et al. combine the 2 types of lesions as characteristics of prolonged urticaria with purpura, granting greater importance to the clinical similarities than to the histological resemblance. In our experience, recent UV has a homogeneous erythematous or purpuric color, and leaves purpura in the entire region of the rash on resolution (Fig. 1). The wheals with the lymphocytic infiltrate have areas of an ecchymotic yellowish color within the acute lesions or extending beyond their bounds (Fig. 2). We consider that, when urticarial wheals persist more than 24h, the residual purpura surrounding the entire area of the lesions supports the diagnosis of UV, whereas a yellowish or ecchymotic discoloration on the periphery or within the wheal corroborates the diagnosis of what Lee et al. classify as prolonged urticaria with purpura in the absence of LV. This could enable the avoidance of biopsy and other studies in single and self-limiting episodes.
Prolonged urticaria without leukocytoclastic vasculitis. The 4 patients had undergone at least one biopsy that revealed the presence of a superficial perivascular lymphocytic inflammatory infiltrate, with or without eosinophils, in the absence of vasculitis. Note the presence of an ecchymotic component within the acute lesions (a and b) and extending beyond the bounds of the wheals (c and d).
The authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of dataThe authors declare that they have followed the protocols of their work center on the publication of patient data.
Right to privacy and informed consentThe authors have obtained the written informed consent of the patients or subjects mentioned in the article. The corresponding author is in possession of this document.
Conflicts of InterestThe authors declare they have no conflicts of interest.
Please cite this article as: Lozano Masdemont B, Horcajada Reales C, Gómez-Recuero Muñoz L, Parra Blanco V. Características del componente purpúrico de la urticaria con vasculitis y de la urticaria sin vasculitis. Reumatol Clin. 2018;14:53–55.