In recent years, the Rheumatology Day-Care Hospital Units (DHUs) have undergone extensive development. However, the quality standards are poorly documented and mainly limited to structure items rather than including broad and specific areas of this specialty.
ObjectiveTo develop specific quality standards for Rheumatology DHUs.
MethodsAfter a systematic review of the literature and related documents, a working group (WG) involving 8 DHU-experienced rheumatologists developed an initial proposal of the quality standards, under the supervision of an expert methodologist. A second round was held by the WG group to review the initial proposal and to consider further suggestions. Once the content was agreed upon by consensus, a final report was prepared.
ResultsSeventeen structure standards, 25 process standards and 10 results standards were defined, with special emphasis on specific aspects of the Rheumatology DHU. The proposal includes: (1) essential standards to (2) excellent standards, (3) a Rheumatology DHU services portfolio and (4) performance criteria.
ConclusionsThe proposed quality standards are the basis for developing the indicators and other management tools for Rheumatology DHU, thereby ensuring a patient-oriented practice based on both the evidence and the experience.
En los últimos años, las Unidades de Hospitalización de Día (UHdD) en Reumatología han experimentado un amplio desarrollo. Sin embargo, existe escasa documentación respecto a estándares de calidad, que mayoritariamente se limita a la estructura y no incluye aspectos específicos de la especialidad.
ObjetivoDesarrollar estándares de calidad específicos para las UHdD en Reumatología.
MétodosTras una revisión sistemática de la literatura y de documentos relacionados, un grupo de trabajo (GT) de 8 reumatólogos, bajo la supervisión de un metodólogo experto, elaboró una primera propuesta de estándares de calidad. Se realizó una segunda ronda para su revisión y sugerencias por todo el GT. Consensuado el contenido, se realizó un informe final.
ResultadosSe definieron 17 estándares de estructura, 25 de proceso y 10 de resultados, con especial énfasis en aspectos específicos de una UHdD de Reumatología. La propuesta incluye: 1) estándares imprescindibles; 2) estándares de excelencia; 3) cartera de servicios de una UHdD reumatológica, y 4) criterios de funcionamiento.
ConclusionesLos estándares de calidad propuestos son la base para la elaboración de indicadores y de otras herramientas de gestión para las UHdD reumatológicas que garanticen una práctica homogénea, centrada en el paciente y basada en la evidencia y en la experiencia.
DHU is defined as hospital units that care for patients for a few hours, either for diagnostic issues, clinical research and/or multiple examinations, as well as to administer treatments that cannot be performed in the outpatient clinic, but do not justify a stay in hospital.1 As an organizational and specific health management formula, and depending on the range of services it offers, the DHU requires structural and functional conditions to ensure both efficiency, quality and patient safety.
The first DHU emerged in the field of Hematology and Oncology to meet the needs of intravenous administration of chemotherapy and supportive care of a group of patients with specific monitoring needs. This, coupled with its monovalent nature, has led to most of the information in our environment in terms of management or efficiency indicators being generated by oncologists and hematologists.2 Internationally, there have been descriptions about the remarkable efficiency of DHU, monographic or polyvalent, in areas such as HIV/infectious, psychiatric and geriatric patients or patients with multiple diseases,3–6 but the literature on quality standards in the DHU remains very low.7,8
Based on this limited documentation, in 2009, the Ministry of Health, Social Services and Equality of Spain developed a set of quality standards and recommendations for DHU, including aspects relating to the rights and interests of the patient, safety, organization and management of DHU, its structure, materials and human resources, as well as the quality of care provided.1
In the field of Rheumatology, DHU have arisen since the introduction of intravenous biologic therapies, a little over a decade ago, for the treatment of rheumatoid arthritis and spondyloarthritis.9 However, they have ended up covering diagnostic and therapeutic needs in many other autoimmune and metabolic diseases. This development not only has resulted in a significant increase in the efficiency of care for patients who previously needed more resources, but has resulted in better quality of life and patient satisfaction.10
The objective of this document is to provide rheumatologists, as well as governments, managers and other health professionals, with criteria to further promote generalization of Rheumatology DHU by developing specific quality standards and other indicators, thus contributing to the improvement in the security and quality of their practice, in all its dimensions.
Materials and MethodsThis document forms part of the proceedings and the methodology of the Icarus Plan to improve quality of care in Rheumatology, draft of the Spanish Society of Rheumatology (SER) (http://www.ser.es/investigacion/Proyectos/Icaro/Icaro.php), which promotes the development of quality standards for implementation in clinical practice.
In connection with this project, initiated in December 2010, an expert methodologist performed a systematic literature search in Medline, Embase and Cochrane Central. In addition, other relevant documents on DHU generated in Spain by rheumatologists and included in previous research projects with a similar approach11,12 were analyzed. A synthesis of the information obtained was performed and a working paper focused on developing standards was developed. Prior to the definition of standards, the selection of quality criteria was adjusted to the usual practice in rheumatology and in line with the dimensions proposed by the Ministry of Health, Social Services and Equality of Spain1: (1) rights and guarantees of patients, (2) patient safety; (3) organization and management of DHU Rheumatology, (4) physical structure and material resources of these units, (5) human resources, (6) quality of care, and (7) review criteria and monitoring standards and recommendations.
A specific working group (WG) was formed, which included a panel of 8 experts of 5 different regions with extensive professional experience in the field and who had expressed particular interest in DHU projects. In a nominal group meeting, in addition to explaining the methodology of the project the results of the previous reviews were presented and discussed, experiences and knowledge were incorporated, new materials were developed and tasks assigned. Once all the material produced was collected, a standards proposal was developed and a second round was set for review, with suggestions made throughout the WG under the methodological supervision of an expert. Once the content had been agreed upon, the final report was written in March 2012, which served as the basis for writing this article.
ResultsIn the concept of a framework with a structure of its own, with common core standards to ensure high quality,1 the WG considered defining relevant portfolio performance and the performance criteria of rheumatic DHU, which in turn determine the structure, process and more specific results standards.
Service Portfolio of Day Hospital Units of RheumatologyThe portfolio of services must be adapted to the individual and contextual circumstances of each center.
In this regard, the provisions included in the portfolio of DHU (Table 1) are divided into essential and optional. The first are what all DHU should offer, with points 1 and 2, being the fundamental basis for these units. The latter contribute to its character and excellence contemplating the optimization of the unit with diagnostic, teaching (undergraduate and graduate), training and research activities. Regarding the diagnostic examinations referred to as optional (Table 1, points b, c, d and e paragraph II) (1), its implementation will be performed by appropriate specialists and post-procedure care may be shared with the doctor in charge of the DHU.
Portfolio of Services of the Day Hospital Rheumatology Unit.
| (I) Essential benefits |
| (1) Administration of intravenous treatments |
| (a) Biological treatment (infliximab, tocilizumab, rituximab, abatacept, and belimumab) |
| (b) Cyclophosphamide |
| (c) Bisphosphonates (zoledronic acid and pamidronate) |
| (d) Corticosteroids bolus |
| (e) Prostaglandins and analogs |
| (f) Iron |
| (g) Gamma globulins |
| (h) Transfusion |
| (i) Antibiotic |
| (2) Clinical monitoring of patients with rheumatic diseases |
| (II) Optional features |
| (1) Diagnostic techniques, including post-procedure care |
| (a) Ultrasound-guided puncture |
| (b) Bronchoscopy |
| (c) Or transthoracic FNAB of soft tissue |
| (d) Thoracentesis |
| (e) Biopsy (liver, muscle, bone, pleural, renal, etc.) |
| (2) Therapeutic procedures |
| (a) Articular lavage |
| (b) Arthrocentesis and infiltrations, including ultrasound-guided |
| (3) Education of patients and caregivers |
| (4) Other techniques and procedures |
| (a) Salivary gland biopsy |
| (b) Lumbar puncture |
| (c) Epidural catheters |
| (d) Vertebroplasty and kyphoplasty |
| (e) Wound care |
| (f) Subcutaneous infusion pump |
| (g) Care of central venous catheter and subcutaneous reservoir |
| (5) Clinical research: clinical trials |
| (6) Specific undergraduate and graduate training (doctors and nurses) |
| (7) Emergency or rheumatologic consultations outside normal hours |
The general criteria for the design of a functional DHU program (Annex 1) are fully described in another document1 and depend essentially on the specific care functions and characteristics of the population served, but eventually could include aspects such as teaching or clinical research. The functional program, along with the performance criteria of the units (Table 2), allows the organization and planning of DHU, and serves as a guide to define the care circuits, always tailored to individual circumstances and the resources of each center.
Performance Criteria and Configuration Episode of the Day Hospital Rheumatology Units.
| Criteria | Clarification/Advice |
| Planning agendas and receiving patients | The appointment will be made with electronic media, with applications for the registration of the patient's arrivalPatients were scheduled in a personalized way, according to their characteristics and preferences whenever possibleSome appointments are in separate outpatient agendas, for therapeutic control and treatmentsTelephone confirmation of appointment the day before |
| Blood samples | The indication or confirmation of treatment may require the evaluation of the results of previous clinical analysis. Optionally, the blood sample can be performed the day before or at health centers |
| Consultations | The consultation aims to clinically evaluate the patient for treatment or confirm management and monitoring of patient progress. A single integrated visit is recommended for analysis and medical assessment of the day procedureNursing consultations are recommended with specific training: welcoming patients, informing them about the structure and functioning of the DHU and patient and family education |
| Prescription | The prescription process shall be electronic whenever possible. We recommend integrating therapeutic orders, formalizing the procedures associated with the prescription, preparation and administration of treatments |
| Preparation of treatment | The preparation should be completed for administration without requiring handling and ensuring the composition and stability, security and the prevention of environmental pollutionThe treatments should be available by the time of the programmed patient allocation.The option of preparing DHU treatments, subject to the availability of resources and proper conditions, may be considered and it is shown that this improves the quality and efficiency of the unit |
| Treatments | The organization of the operation of the unit must conform to the times of administration of each prescription scheme |
| Continuity of care | We recommend assigning a specific doctor for DHU's, ideally a rheumatologistThere must be a method to treat patients requiring unscheduled care, preventing from coming to the emergency in order to ensure continuity of careIt is advised to have a telephone consultation, ideally managed by the nursing staff, identifying the person to contactThe discharge sheet should contain specific instructions on aftercare for: the patient, the Rheumatology doctor responsible for the patient, the Primary Care doctor and nurse |
DHUs: Day Hospitalization Units.
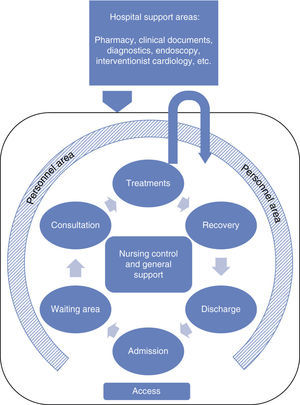
In this regard, in outline, the optimal circuit for setting the episode of care in these units is illustrated in Fig. 1. Ideally, the design of the physical structure of a DHU must consider the logical sequence of activities for which it is conceived: physical access, admission, waiting, consultation, treatment or procedure, recovery and medical discharge. All areas must be properly labeled, be of adequate dimensions and ensure patient privacy. For a polyvalent DHU (i.e., shared by more than one specialty), most areas are shared with other hospital services, but should include: reception area, spaces for administration of treatment, nursing and general support, administrative and support areas for staff.1
Along with the spaces dedicated to providing treatment, DHU's should have at least one medical area for clinical evaluation, information, obtaining consent and eventually performing diagnostic processes. The control area must allow nursing observation of patients during administration of treatments and recovery, so the central location with direct view of patients is the most appropriate. Ideally, the incorporation of a nursing area with its own telephone would facilitate the implementation of the various standards described below.
Quality StandardsIn total, 52 quality standards were developed and agreed upon: 17 related to structure (Table 3), 25 to process (Table 4) and 10 to results (Table 5).
Structure Standards of Day Hospital Rheumatology Units.
| n | Standard structure | Clarification/Advice |
| 1 | All rheumatology departments must have or have access to a DHU | If not monographic, at least have access to a multipurpose DHU |
| 2 | Adequate physical structure | Main physical areas: reception, DHU positions, the nurses and general support, administrative area and support for staff |
| 3 | Suitable access and location | DHUs should ideally be at street level and always with good wheelchair accessibility conditions |
| 4 | Broad attention hours | If possible daily and morning and afternoon shifts |
| 5 | Privacy during the visit/stay | Individualized consultation for physical examination or other procedures and the possibility of privacy in the room for the delivery of treatment, using curtains, screens, etc. |
| 6 | Electronic format that can be used by information systems | Connected to the hospital for the management of patients and agendas, financial and administrative management and general services, electronic prescribing, registry of data collection and monitoring (such as clinical unit and system-evaluation scorecard) |
| 7 | The boxes will be located around direct support spaces in a single, centralized disposition | |
| 8 | Air conditioning | |
| 9 | Logging and defining lines of responsibility | Responsibilities, reporting lines, responsibilities and competencies must be clearly defined |
| 10 | DHU's must have at least one administrative worker with experience to support those responsible for the unit, managing admissions and waiting lists | The management of clinical documentation correspond to the admission and clinical documentation unit or equivalent |
| 11 | Have a person responsible (ideally a rheumatologist) for management. | It may be the same person as that responsible for the administration of the treatments. That person is responsible for organizing and coordinating unit staff, with appropriate use of resources, program activities, quality assurance and management of waiting list |
| 12 | The unit must have a physician (rheumatologist) for administration of treatments | This person will be responsible for patient care (prescription, clinical monitoring), plus monitoring. If the physical presence of the rheumatologist is not possible in the Unit, there should be one located and accessible |
| 13 | The unit must have trained nursing staff in rheumatologic processes and procedures | Even if it is a multipurpose DHU |
| 14 | Have a responsible nursing staff | Its function is to coordinate care planning, scheduling activities of nursing staff and control the availability of material resources |
| 15 | Provide a nursing assistant | |
| 16 | Physical or electronic availability of key documents | 1) Service Portfolio2) Medical Records3) Informed consents4) Admission program5) Guidelines and/or clinical practice protocols6) Protocols of confidentiality and legal access to patient data7) Standard Working Procedures8) Procedures required in clinical trials8) Reports of medical discharge9) Registration of complaints and suggestions10) Operation Manual11) Hospital Code of Ethics13) Insurance of responsibility14) Plan for self-protection against possible disasters |
| 17 | Plan for self-protection | This will establish the organization of human and material resources available to prevent risk of fire or equivalents and immediate intervention to ensure against possible disasters |
DHU: Day Hospital Unit.
Standards Processes of the Day Hospital Rheumatology Units.
| n | Quality standards | Clarification/Advice |
| 1 | Quality plan tailored to each DHU | It includes, among others, analysis, archiving, review and updating of consensus, CPG, technical specifications of drugs, protocols, and operating organization and operation of the DHU |
| 2 | Organization and operation manual | This must include organizational, resources, physical layout of the DHU, care organization and standards and services portfolios |
| 3 | Ensure optimum cleanliness and hygiene | Cleaning protocol for the dependencies, facilities, equipment and supplies and equipment |
| 4 | Provide contact and telephone consultation to patients and caregivers | With identification of the contact person |
| 5 | Give ID card of the contact person | |
| 6 | Have a system of appointments and appointment confirmation | |
| 7 | Providing a delay guarantee for access to the DHU | The waiting list for access to the unit should be limited and defined according to each treatment or procedure (e.g. differentiate steroid boluses from Zoledronic acid for osteoporosis) |
| 8 | Have a reception procedure | Information that includes at least a description of the different phases that the patient go through and related special warnings or advice |
| 9 | Provide written information about the DHU and all processes related to the patient | (a) Advance directives on admission and access to the DHU(b) Instructions for patient stays, for caregiver and roommates(c) Instructions for immediate aftercare and post-discharge(d) The probable issues that the patient may present due to medication and the care that should be given(e) Forms of access to continued resources |
| 10 | Patient record | Should include, among others, the identification of hospital or, physician/nurse responsible for the care, post-discharge, patient identification, dates and discharge |
| 11 | Ensure efficient coordination between the pharmacy and DHU | No delay between prescription and administration, with the possibility of preparing drugs in the same DHUThe definitive validation for medication preparation should be made following confirmation of patient care and, once reviewed, show no impediment for administration |
| 12 | Updated protocols (medical, nursing, pharmacy, administrative, management) | Must be accredited with the update date and person responsible |
| 13 | Have and use a checklist of tasks to perform | Includes reception, validation procedure to start medical and nursing care (analytical, clinical evaluation, etc.) during the procedure (infusion tests), monitoring and discharge (report, appointment, etc.). |
| 14 | Have a contingency plan for key processes | In case of fever, adverse events, patients who do not come to appointment, death, etc. Ability to appoint another patient on that day |
| 1 | Activity log and contents coding | Electronic format preferred |
| 16 | Offer integrated unique visit opportunity | Lab analytics, medical assessment, procedure and discharged on the same day |
| 17 | Provide health education and self-care | Education for self-care, including, among others: healthy lifestyle, recognition of alerts and management for pain and other symptoms, treatment compliance, etc. |
| 18 | Dispense appropriate treatment to the patient and their caregivers | |
| 19 | Perform systematic and periodic evaluation of care received by patients | Through surveys of satisfaction, perceived quality |
| 20 | Delivery discharge report and treatment plan to the patient | Always or in special situations: at baseline, changes in medication, last discharge, in case of adverse events, etc. with a detailed specification of the post-discharge care |
| 21 | Promote coordination with primary care professionals | To ensure continuity of care |
| 22 | Undergraduate and graduate DHU training | For medical students and nursing and rheumatology residents |
| 23 | Provide care coordination programs within the center itself | To identify user needs and guide or provide social resources |
| 24 | Provide and promote specific training programs for DHU staff | At all levels of health workers: medical, nursing, ancillary, administrative, orderlies, etc. |
| 25 | Perform specific clinical sessions in Rheumatology DHU | Monographic sessions or within the service |
CPG: clinical practice guideline; DHU: Day Hospital Unit.
Results of Standards in Day Hospital Rheumatology Units.
| n | Quality standards | Clarification/Advice |
| 1 | DHU must have electronic application that allows to obtain (daily, monthly, quarterly or annual) information on the activity | Implementation of an appropriate information system to monitor the results of the activity-No. total procedures performed-No. total patients seen-No. total suspended proceedings and causesTotal No. of each procedureAverage daily patientsAverage patients per DHU post |
| 2 | Regular and systematic evaluation of DHU staff performance | Including all health care staff and those responsible for management and administration |
| 3 | Regular and systematic evaluation of adherence to protocols | For example, by random audit of medical records |
| 4 | Regular and systematic evaluation of patient satisfaction | User surveys, to determine the degree of acceptance and satisfaction of the method, and to establish a diagnosis of problems in the development of the service |
| 5 | Registration of adverse events and incidents | All those that occurred during the procedureLater: at least serious events attributable to the procedure or treatment |
| 6 | Registration of all DHU discharges | Encoded by the MSD center or other specific coding |
| 7 | Provide the estimated time and cost for each DHU procedure | |
| 8 | Regular Economic evaluation of drugs | Minimum: costs; preferred cost/effectiveness or cost/utility. Period: at least annually |
| 9 | Electronic application that allows to obtain (monthly, quarterly or annual) information on results | Percentage of patients requiring admissionRate of adverse events during the procedureCrude death rateSpecific outcomes collected per patient by disease: rates of activity, function, quality of life, etc. |
| 10 | External quality certification | For example, ISO 9001-2008 |
MSD: minimum set of databases; ISO: International Standard Organization; DHU: Day Hospital Unit.
Regarding the structure standards, these must cover all activity of the DHU and all those involved in these units, so the creation of a multidisciplinary working group for its development and implementation was recommended. Aspects of the physical structure and the necessary materials were included in first place. One of the recommendations that the panel considered a priority is the use of new technologies and information systems for better management.
Second, standards relating to human resources and organization were included. Rigorous logging and strict definition of the DHU lines of responsibility are imperative, so the obligations, rights and responsibilities of all personnel, as well as the hierarchical structure should be clearly defined. There needs to be a dedicated line for management of responsibility and another one for patient care. However, it is contemplated that both can coincide on the same person. Key documents that should be available, located and accessible, either on paper or electronic format, for all personnel involved (Table 3) in the structure standards.
Process standards listed in Table 4 provide for any activity within the unit, not only in terms of care, but also administrative or management. The WG points out that, among strategic processes, the development of a manual of organization and operation, which will direct the translation of key processes.
Regarding support processes, one of the core standards is to ensure efficient coordination between the Hospital Pharmacy and DHU without delay between prescription and administration, including the possibility that the medication preparation is done by the DHU itself.
The WG considered relevant to introduce a quality standard process that advocated taking advantage of DHU stays, prolonged sometimes for hours, for health education to the patient, to become involved in managing their own health and managing their illness. Education should also include family members or caregivers.
As for the discharge patient report and given the regular and frequent nature of many therapeutic procedures, the WG states that this is not necessary in every patient coming to the DHU, but must be done in the following situations: definitive discharge from the DHU, changes in medication or dosage, in case of adverse events and other circumstances, including the patient's decision, involving changes in treatment. The report should include detailed discharge aftercare.
Finally, standards of performance, shown in Table 5, indicate how we should measure the result of the structure and processes of all DHU. It is considered essential to have an electronic system that allows the recording and periodic analysis of both the activity and the results. Health outcomes assessed should be able to register, through the preset specific outcomes, manifestation and analysis according to disease. Indices of activity and function in: rheumatoid arthritis (e.g., DAS28, Simplified Disease Activity index, Clinical Disease Activity Index, HAQ), spondylitis (BASDAI, Ankylosing Spondylitis Disease Activity Index, BASFI, etc.), systemic lupus erythematosus (SLEDAI, SLICC, etc.), vasculitis (BVAS, Five factor score, etc.), scleroderma (Raynaud severity indices and digital ulcers, modified Rodnan skin index), osteoporosis (new fractures, bone mineral density) and other specific diseases or manifestations which may be seen at the DHU, and whose enumeration exceeds this document. It is considered highly recommended to also record quality of life indices, which allow, among other things, a more rigorous evaluation of direct costs than a simple economic evaluation.
Regular assessment of performance and competence of staff, both assistance care as well as the management and administration staff, also should be performed.
Considering that one of the pillars of quality is safety, registration and evaluation of adverse events and incidents is imperative. Finally, the perceived quality through surveys of patient satisfaction should be assessed.
All the proposed standards are subject to change and should be reviewed periodically in the light of developments, with the best available evidence and experience in a given context. Generically, the process and outcome should be evaluated annually, and structure at least every 5 years.
DiscussionDay hospitalization has been a considerable development in recent years in Rheumatology departments, becoming an important part of their daily work and their service portfolio. Although the performance and characteristics of each of the13 DHU's is highly heterogeneous, the progressive increase in performance and complexity on the appropriate management portfolio transcends, in many cases, the mere organizational formula to become a real model servicing complex rheumatologic patients. Additionally, DHU have become an essential element in clinical research, both due to the need for clinical trials, as well as for the support in data collection and sampling for epidemiological and basic research.
The contribution of this work is novel in that it addresses the development of quality standards, both in structure and operating results for DHU, specifically in the field of Rheumatology. The recent development of these units explains that the standards developed previously collected more specific aspects of our specialty. Publications of other health institutions outside our country thoroughly focused on structural requirements and the benefits of Rheumatology are only mentioned7,8 in the updated guidelines of the English National Health System as part of their service portfolio.7 Agencies such as the Joint Commission, with recognized expertise in the creation of standards aimed at accreditation, do not provide this type of care provision and only refer to treatment programs as ‘partial’ hospitalization targeting healthcare providers in behavioral disorders (http://www.jointcommission.org/accreditation/bhc_seeking_accreditation.aspx).
In rheumatology, we find several studies in Spain that describe the degree of implementation of DHU and their distribution,14 and begin to raise the variability in their characteristics and operation.12,13 In these publications, key issues for the operation of DHU, as well as identifying weaknesses and areas for improvement, and as a need to establish standards for operation on the basis of quality criteria.11,12 The first approach is based on these criteria in the definition of the process map of Rheumatology DHU and reaches a consensus in a set of quality criteria for strategic key and support processes which are then analyzed in various DHU in a benchmarking process.12 The results of this study, in line with other general standards already published by the SER,15 represent a breakthrough because they provide recommendations and specific management tools for use at the local and institutional level.
Regarding the structure standards, the comprehensive description of basic criteria, whether of mono or polyvalent units, has not been the subject of this article and could represent a limitation, but the WG understands that the requirements of human resources and equipment, either themselves or those of an already defined DHU1,7,8 are widely available in the final extensive report (http://www.ser.es/investigacion/Proyectos/Icaro/Icaro.php). The panel, however, wanted to emphasize some aspects considered crucial such as the definition and dissemination of the portfolio of services, the need for involvement of rheumatologists in the management of DHU, the presence of nurse training and specific training, key documents that should be accessible electronically or necessary for the registration and management of all processes. The protocols, a fundamental and essential part of any health care activity, acquire special relevance in this mode, because they ensure uniformity in very standardized practices and prevent unjustified variability.
In addition to the scarcity of previous publications, regarding the processes and results, one must add the constant change and new opportunities in the use of DHU in Rheumatology. Here, in our country, many of the DHU have become the framework for monitoring and centralized prescription of all biological drugs, either subcutaneous or intravenous. The need for risk management and their rational use and other therapies have contributed to the development of Rheumatology DHU, whose expansion and staffing requirements has driven parallel development of advanced nursing skills in Rheumatology.16 DHU's have emerged as one of the suitable frameworks for the application of these skills, as evidenced by publications and experiences in our country.17 Similarly, the development of specific nursing clinics, either in the framework of the DHU or outpatient clinics, is one strategy that has contributed to the efficient management of outpatient rheumatic patients and has led the SER to publish their own quality standards.18 Part of these standards collect requirements, nursing skills and competencies that can be applied at DHU's, and underscore their relevance in many key processes: the safe administration of drugs, telephone consultation, patient and caregiver education or their contribution to the monitoring of illness, which facilitates patient management guidelines and recommendations tailored to a more rational and drug use.
The WG also highlighted other irrevocable standards, and the use of standardized work and informed consent procedures, provided these are indicated. The need for a rapid access of new patients to DHU's, which should be no more than 15 days later, was found. However, the consensus of acceptable waiting days is more complicated, because it varies depending on the resources of each center and the relative urgency of the procedure.
One limitation of this study may lie in the limited number of experts who participated. However, the actual study is part of a previous project in which rheumatologists from 21 different hospitals defined quality standards and recommendations, also with methodological support.12 Also, in the situational analysis of this proposal, we have taken into account the available data on the current DHU status and different organizational contexts in our country.13,14
The proposed quality standards should form the basis for each service to develop the indicators needed to ensure a good practice, evaluate their activities and identify areas for improvement in the DHU, also incorporating experience. In the current economic climate, generating outcome indicators, electronic records for the prescription, administering, dispensing and monitoring of drugs, with an integrated control panel, is a unique opportunity for efficient management of complex patients.
Since feasibility is not uniform, the document contains, along with essential standards, other proposals that will shape excellence care, as the existence of administrative staff or DHU clinical research, the dissemination of specific research activities as publications or the quality certification of the units. In this context, we believe that the contribution of this study, together with the generation of indicators, can lead to the creation of an individualized quality plan for each of the DHU's, offering multiple opportunities for advancement to the services that use them (Table 6).
Opportunities Arising From a Quality Plan for Day Hospital Rheumatology Units.
| 1 | Increased portfolio of a Unit of Rheumatology |
| 2 | Setting of excellence for comprehensive care of complex rheumatologic patients in which the most innovative aspects of the specialty are reflected |
| 3 | Teaching, continuing medical education, continuing professional development |
| 4 | Research and innovation |
| 5 | Leadership as specialty knowledge of rationality and peculiarities of use of biological therapies |
| 6 | Rational use of high-cost therapies and commitment to sustainability |
| 7 | Education for self-care and “activation” of patients and caregivers |
| 8 | Quality management that allows continuous evaluation to improve and achieve external accreditation |
| 9 | Greater involvement in managing tasks in the future for greater independence/self-management Rheumatology services |
Ultimately, rheumatologic DHU's are much more than mere organizational formula to provide an intermediate service between hospitalization and outpatient clinics. In this context, one of the most important contributions to the quality standards that are proposed is to create management tools to ensure consistent, patient-centered, evidence-based and experienced practice and be able to define the indispensable quality requirements for excellence.
Ethical ResponsibilitiesProtection of people and animalsThe authors declare that this research did not perform experiments on humans or animals.
Confidentiality of dataThe authors state that patient data do not appear in this article.
Right to privacy and informed consentThe authors state that no patient data appear in this article.
FinancingFunded by the Spanish Foundation of Rheumatology (FER) with a grant from Bristol-Myers Squibb (BMS). The company has not participated in the project design and has not been involved in writing the findings or final report of this manuscript.
Conflict of InterestDr. García-Vicuña has received funding for research and training and fees for consulting and presentations: Roche, BMS, MSD, UCB, Pfizer, Actelion and Hospira.
Dr. Montoro declares conflicts of interest concerning Abbvie, BMS, Glaxo, MSD, Pfizer, Roche, UCB.
Dr. Bustabad has received research funding, consulting and presentation fees from Abbvie, Pfizer, Roche and MSD.
Dr. Centeno Gómez has received grants from Pfizer, payment for lectures from Pfizer, Abbvie, BMS, Roche, MSD and Menarini, Roche advisory payments and MSD, and Pfizer for attending conferences.
Dr. Pérez-Pampín declared conflicts of interest related to BMS, MSD, Pfizer, Roche, UCB.
Dr. Roman Ivorra has received research funding or honoraria for consulting and lectures from Roche, MSD, Pfizer, Abbvie, UCB, GSK, BMS, Actelion, Amgen.
Dr. Balsa has received research funding or honoraria for consulting and lectures from UCB, Pfizer, Roche, BMS, Abbvie, GSK, MSD and AMGEM.
Dr. Loza reports receiving payment for providing professional services from Abbvie, Roche, MSD, BMS.
Drs. Egues Dubuc and Muñoz-Fernández declare no conflict of interest related to this article.
Special thanks to the participants in the project for Excellence in Day Hospitals in Spain (HD-Reumatolex),12 for their previous contribution to this project: Dr. Pedro Barceló, University Hospital Vall d’Hebron, Barcelona; Dr. Alberto Bermúdez, University Hospital Virgen de la Arrixaca, Murcia; Dr. Luis Carreno, Hospital General Universitario Gregorio Marañón, Madrid; Dr. Eduardo Collantes, Hospital Universitario Reina Sofía, Córdoba; Dr. Alicia Garcia, Hospital Universitario Virgen del Rocío, Sevilla; Dr. Juan Gomez-Reino, Hospital Clinico Universitario, Santiago de Compostela, La Coruña; Dr. Gennaro Grana, Hospital Universitario Juan Jinx, La Coruña; Dr. Manuel Guzman, University Hospital Virgen de las Nieves, Granada; Dr. Emilio Martín Mola, Hospital Universitario La Paz, Madrid; Dr. Isabel Mateo, Hospital Universitario 12 de Octubre, Madrid; Dr. Joan Maymó, Hospital del Mar, Barcelona; Dr. Juan Mulero, Hospital Universitario Puerta de Hierro, Madrid; Dr. Federico Navarro, University Hospital Virgen Macarena, Seville; Dr. Joan Miquel Nolla, University Hospital of Bellvitge, Barcelona; Dr. Eliseo Pascual, General University Hospital of Alicante; Dr. Arturo Rodriguez de la Serna, University Hospital Santa Creu i Sant Pau, Barcelona; Dr. Raimón Sanmartí, Corporació Sanitària Clínic, Barcelona; Dr. Eduardo Ucar, Hospital de Basurto, Bilbao.
| Demographic analysis of the environment (with particular reference to the population included in the capture area of the unit and the selection criteria of patients) |
| Study of DHU theoretical demand of treatments, considering the volume of procedures performed. The pervasiveness of the unit in its environment should be taken into account, once it is fully operational |
| Analysis of the architectural infrastructure where the activities of DHU (definition of new or modification of existing infrastructure) will be developed |
| Analysis of the production capacity, according to varying scenarios efficiency |
| Study of the need for staff and equipment, based on the demand, the planned activity and portfolio of existing services in the hospital |
| Definition of operation with reference to the policy manual, including schematics of movement of patients, staff, family and materials |
| Configuration the care circuit (forms of patient access, administrative processing of receipt, transit within DHUs, alternatives to output, etc.), forms of medical care and post-discharge functional relationships with other environment structures (central services, emergency, critical care units, primary care, etc.). |
| Functional Plan, according to the specific characteristics of its organization |
| Economic survey, in which both the amount of the planned investment in infrastructure and equipment as well as the estimated running costs of personnel, supplies and maintenance for the activities and economic and health impact of the operation will be reflected on the institution it depends from. |
Reproduced with permission from the reference Working Group for the preparation of “DHU Standards and Recommendations”.1
Source: Ministry of Health, Social Services and Equality.
Please cite this article as: García-Vicuña R, Montoro M, Egües Dubuc CA, Bustabad Reyes S, Gómez-Centeno A, Muñoz-Fernández S, et al. Estándares de calidad en una Unidad de Hospitalización de Día reumatológica. Propuesta del Grupo de Trabajo de Hospitales de Día de la Sociedad Española de Reumatología. Reumatol Clin. 2014;10:380–388.